Cerebro vascular disease (stroke) is the second leading cause of death worldwide, which occurs predominantly in the mid-age and the older adults. The WHO has estimated 5.7 million deaths which were caused stroke in 2005 worldwide, which was equivalent to 9.9 % of the total deaths. Over 85 % of these deaths occurred in people who were living in the low to the middle income countries. Approximately 33 % of these deaths occurred in people who were aged less than 70 years [1]. Stroke accounts for 2 % of the hospital registrations, 1.5 % of the medical registrations and 9 - 30 % of the neurological admissions in the major hospitals [2].
Stroke is a multi factorial disease that occurs due to a combination of the risk factors, all of which do not all have to be present at the time of its presentation. The major modifiable risk factors are elevated blood pressure, tobacco usage in any form, physical inactivity, low fruit and vegetable consumption in the diet, heavy alcohol consumption, overweight and diabetes. The non-modifi- able risk factors include age, sex and family genetics viz. elderly males are associated with an increased risk of stroke in many populations [1]. The environmental factors are passive smoking and poor access to the medical treatment [1]. The other risk factors may be atrial fibrillation as well as other cardiac diseases [1].
The role of hypercholesteraemia as a risk factor for stroke is still an issue of debate. There is evidence that low total cholesterol levels may be associated with a decreased risk of ischaemic stroke but that they also may be accompanied by higher rates of haemorrhagic strokes [1].
The National Commission on Macroeconomics and Health, India, has estimated 1.67 million stroke cases in India by the year 2015, thus suggesting that stroke will be a rising epidemic in India in the days to come. This may be due to the increasing prevalence of hypertension, diabetes, dyslipidaemia, the fastchanging lifestyles and restructuring of the population [3,4]. The lack of a structured data on stroke from many countries has hampered the efficient coordination of stroke prevention, treatment, and rehabilitation [1]. Due to the future demographic changes, strategies to reduce the stroke burden are urgently needed to ensure adequate health resources.
The WHO STEPS Stroke Surveillance provides the framework for the data collection and for the comparisons between and within populations [1]. The present study was conducted with the aim of generating data which pertained to the clinical profile of stroke in our institution by using the Steps Stroke manual version 2 and of making note of the risk factors and the correlation of the outcome with the Glasgow’s Coma Scale (GCS) at admission and with the Modified Rankin Scale (MRS) on the 28th day.
MATERIALS AND METHODS
The WHO Stroke Surveillance Study step 1 focuses on the hospitalized stroke patients only. This prospective study was conducted from June 2011 through June 2012 at a tertiary care hospital which was located in western region of Uttar Pradesh, India, which has a huge clientage of patients from the rural background, by using the WHO Stroke Steps Manual version 2 1. The evaluation of stroke in the community (step 2 and step 3) was not performed due to various obvious reasons.
The WHO has defined stroke as a clinical syndrome which is characterized by rapidly developing clinical symptoms and/or signs of focal, and at times, global (applied to the patients in deep coma and to those with subarachnoid haemorrhages), loss of cerebral function, with the symptoms lasting for more than 24 hours or leading to death, with no apparent cause which is other than that of a vascular origin [5]. This definition includes the stroke which is caused by a cerebral infarction, a Primary Intracerebral Haemorrhage (PICH), an intraventricular haemorrhage and in most of the cases, a Subarachnoid Haemorrhage (SAH), while it excludes a subdural, epidural or an Intracerebral Haemorrhage (ICH) or infarction which is caused by an infection/tumour [1].
During the 12 months of the study period, a total of 13,538 patients were admitted to this hospital, out of which 157 cases of stroke (as per theWHO definition) were included in the study after taking an informed consent from them. Permission from the ethical committee of the hospital was also obtained prior to the execution of this study.
The observations were noted with the help of the hospital staff who were posted in the Department of Medicine. The clinical presentation, the GCS on admission, the radiological findings, a past history of hypertension, diabetes, coronary artery disease and strokes/TIA and a family history of stroke were taken into account and they were recorded. The evaluations of haemoglobin, the general blood picture, blood sugar and the lipid profile and CT head / MRI of the head were done. The complications were assessed until the day of discharge. The outcome was noted on discharge and on the 28th day following the stroke, by using the modified Rankin score. The data was statistically analyzed.
The following definitions were used to identify the modifiable risk factors:
Atrial fibrillation: The atrial fibrillation in the ECG prior to the stroke (based on the records) or during the hospitalization.
Current tobacco use: Whether the patient was a current tobacco user (smoking and other forms of tobacco), or was a recent tobacco user but had stopped less than 3 months before the acute stroke event.
Diabetes mellitus: Whether the patient had been diagnosed with or had self reported Diabetes mellitus and elevated glycosylated haemoglobin and had been using antidiabetic drugs.
Hypercholesterolaemia: Whether the patient had reported elevated plasma total levels of >220 mg% or LDL cholesterol levels, or had been using lipid-lowering medication.
Raised blood pressure: Whether the patient had diagnosed or self reported a raised blood pressure of >160/90 or had been using antihypertensive drugs.
The outcome was analyzed according to the Modified Rankin Scale on the 28th day following the stroke, in the following manner
| Score | Scale | Description |
| 0 | No symptoms | No symptoms at all |
| 1 | No significant disability | No significant disability |
| 2 | Slight disability | Unable to do all previous activities, able to look after own affair without assistance |
| 3 | Moderate disability able to walk without assistance | Requires some help but able to walk without assistance |
| 4 | Moderate disability Unable to walk without assistance | Unable to walk without assistance and unable to attend to own body needs without assistance |
| 5 | Severe disability | Bedridden, incontinent and requiring constant nursing care and attention |
RESULTS
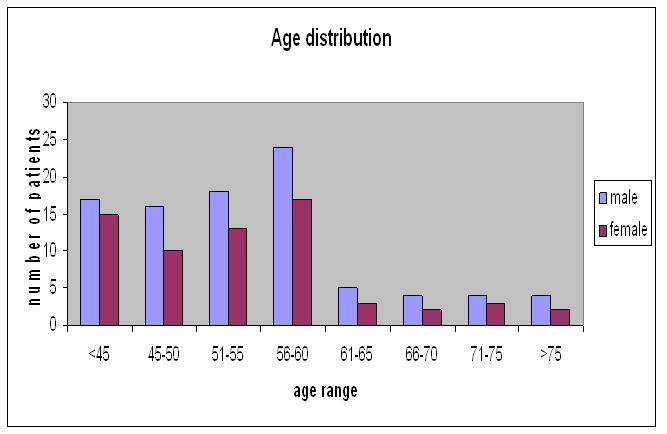
This study comprised of 157 CT/MRI confirmed stroke cases (92 males and 65 females), the distribution of whose ages has been shown in [Table/Fig-1]. The prevalence of stroke was 1.12 % amongst the hospitalized patients. The mean age was 51.6 years, and the ages of the patients ranged from 18-78 years. It was evident that stroke was prevalent in the age range of 56-60 years. It was also noted that 14.6 % of the patients were below 45 years of age.
Prevalence of stroke in various age groups in both the sexes
The risk factor analysis revealed that the most prevalent risk factor was hypertension. Hypertension, either alone or in combination with other risk factors, was seen in 88 (56.1 %) patients, as has been indicated in [Table/Fig-2].
Stroke- Modifiable risk factors analysis with DM /HT/dyslipedimia/smoking as risk factors
Patients without identifiable risk factor =9
Patient with rheumatic heart disease with atrial fibrillation=1
Patients with HT/DM/dyslipedimia/smoking =147 Total =157
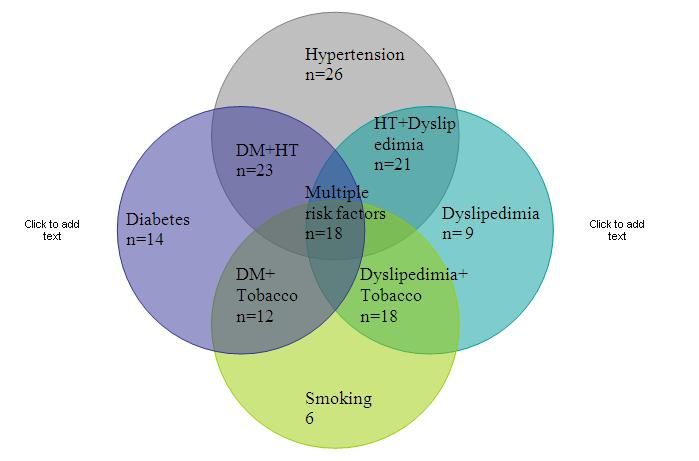
Dyslipidaemia [one or more of the parameter/s in the lipid profile was/were deranged (s. cholesterol >220, TG >150 and LDL >120)] was seen as the only risk factor in nine (5.7 %) patients. Diabetes mellitus was the single risk factor in 14 (8.9 %) patients. The use of tobacco could be attributed as the only risk factor in six (3.9 %) patients. The variable overlapping of the symptoms has been explained by way of Venn diagrams [Table/Fig-2]. No risk factor could be identified in nine (5.7%) patients. One patient had rheumatic heart disease with atrial fibrillation. A past history of stroke was noted in 10 (6.37%) patients. Six (3.9 %) patients had a prior Transient Ischaemic Attack (TIA). A family history of stroke was noted in 13 (8.3 %) patients [Table/Fig-1].
The clinical presentations of stroke were protean [Table/Fig-2]. Hemiplegia/hemi paresis was the most common presentation, followed by aphasia. Fifteen patients presented with status epilepticus. It was noted that ischaemic strokes (71%) were the most frequent kind of strokes, followed by haemorrhagic strokes (29%). The age distribution and the stroke subtype have been presented in [Table/Fig-3]. Amongst the ischaemic infarcts, the anterior circulation infarcts were the most frequent, followed by the posterior circulation, basal ganglion and the paraventricular infarcts [Table/Fig-4].
Other overlapping risk factors amongst 157 patients
| Sl. No. | Risk factors | No. of patients | Percentage |
| 1. | Past history of stroke | 10 | 6.4 % |
| 2. | Past history of TIA | 6 | 3.9 % |
| 3. | Family history of stroke | 13 | 8.3 % |
| 4. | Anemia | 54 | 34.4 % |
Clinical Presentations of stroke amongst 157 patients
| Sl. No. | Clinical presentation | Number of patients | Percentage |
| 1. | Unilateral or bilateral motor impairment (including lack of coordination) | 88 | 56.05 % |
| 2. | Unilateral or bilateral sensory impairment | 14 | 8.91 % |
| 3. | Aphasia/dysphasia (non-fluent speech) | 13 | 8.28 % |
| 4. | Hemianopia (half-sided impairment of visual fields) | 15 | 9.55 % |
| 5. | Forced gaze (conjugate deviation) | 10 | 6.36 % |
| 6. | Apraxia of acute onset | 7 | 4.45 % |
| 7. | Ataxia of acute onset | 6 | 3.82 % |
| 8. | Perception deficit of acute onset | 4 | 2.54 % |
| Total | 157 | |
Deep coma (GCS <3) was observed in 32 patients at the time of the presentation [Table/Fig-5]. These patients had a higher mortality and the commonest aetiology which was noted in them was an intracranial haemorrhage [Table/Fig-6].
Glasgow’s Coma Scale (GCS) on admission and 1 week mortality
| Sl. No. | Hemorrhage (n=45) | Non hemorrhagic infarct (n=112) |
| Recovered | Expired | Recovered | Expired |
| <3 | 9 | 14 | 2 | 7 |
| 4 -8 | 8 | 6 | 24 | 3 |
| 9 - 15 | 5 | 3 | 74 | 2 |
Age distribution and stroke subtypes
| Sl. No. | Age range (years) | Non hemorrhagic infarct | Hemorrhage |
| 1. | <45 | 7 | 8 |
| 2. | 45-50 | 12 | 3 |
| 3. | 51-55 | 28 | 7 |
| 4. | 56-60 | 47 | 10 |
| 5. | 61-65 | 6 | 7 |
| 6. | 66-70 | 5 | 3 |
| 7. | 71-75 | 4 | 3 |
| 8. | >75 | 3 | 4 |
The overall mortality was 22.29 % in the haemorrhagic strokes and in those patients with infarcts who had multiple risk factors. The correlation of the stroke subtype and the outcome after 28 days have been shown in [Table/Fig-7]. The Modified Rankin score of > 3 i.e. a significant residual deficit was noted in 78 patients [Table/ Fig-8].
Radiological Arterial territory affected in infarct cases
| Sl. No. | Area affected in infarct | No. of patients (n=112) | Percentage |
| 1. | Anterior circulation | 65 | 57.14 % |
| 2. | Posterior circulation | 24 | 21.42 % |
| 3. | Basal ganglion | 16 | 15.31 % |
| 4. | Para ventricular | 7 | 6.12 % |
Outcome after 28 days as assessed by Modified Rankin Scale (MRS)
| Outcome | Hemorrhage | Infarct | Total |
| Male | Female | Total | Male | Female | Total |
| Expired | 12 | 8 | 20 | 8 | 7 | 15 | 35 |
| MRS <3 | 8 | 3 | 11 | 17 | 12 | 29 | 40 |
| MRS 3-4 | 5 | 2 | 7 | 19 | 14 | 33 | 40 |
| MRS 4-5 | 5 | 2 | 7 | 18 | 17 | 35 | 42 |
| Total | 30 | 15 | 45 | 62 | 50 | 112 | 157 |
DISCUSSION
The WHO STEPS stroke version 1.1 has been successfully tested in the Indian Collaborative Acute Stroke Study (ICASS), which was a prospective, multi-centric study on unselected CTconfirmed cases of acute stroke (less than 72 hours), who had been admitted to the major university hospitals in India viz. in Chandigarh, New Delhi, Mumbai, Pune, Bangalore, Chennai and Hyderabad [6]. During the study period from 2002 to 2004, reliable information was available on 2162 acute stroke cases (which were CT confirmed). It was evident that the incidence of stroke rose with advancing age; the maximum being in the age band of 41-70 years [7].
During the 12 month study period, we examined 157 patients with a radiologically confirmed diagnosis of stroke prospectively. The mean age was 51.6 years, and their ages ranged from 18-78 years. It was evident that the strokes were most prevalent in the age range of 56-60 years. The information which was generated in this study was comparable to those of other Indian studies [7, 8]. The peak age was one decade later in the developed countries. The male: female ratio was 1.46:1; an overall male preponderance was seen, which was similar to that which was seen in other studies [8].
In the present study, 14.6 % of the patients were below 45 years of age. The Indian studies have shown that about 10- 15% of the strokes occurred in patients who were below the age of 40 years, which was high as compared to that in other countries [8–10].
Hypertension (HT), either alone or in combination with other risk factors, was the most prevalent risk factor, which was found in 56 % patients in our study, which was comparable to the results in the ICASS study [6]. Various observational studies have shown that the usual blood pressure levels were directly or continuously associated with the initial occurrence of stroke. As a consequence, blood pressure has been recognized as an important determinant of the risk of the initial stroke in non-hypertensive as well as in hypertensive patients [11,12].
In the present study, hypertension along with diabetes was observed in 14% patients. Diabetes alone was noted in 8.9% patients, dyslipidaemia was noted in 5.7% patients and the use of tobacco was noted in 3.9% patients. Anaemia was found in 34.4% patients. No risk factor could be identified in nine (5.7%) patients. Only 1 patient had rheumatic heart disease with atrial fibrillation. The major risk factors which were identified in India were hypertension (a diastolic blood pressure of >95 mm Hg), hyperglycaemia, tobacco use, and low haemoglobin levels (<10 gm%) [6,7]. A past history of stroke was noted in 10 (6.37%) patients. Six (3.9%) patients had a prior Transient Ischaemic Attack (TIA). A family history of stroke was noted in 13 (8.3%) patients [Table/Fig-1]. Due to the different designs of the other studies and the populations who were at risk in them, a comparison was not possible; however, the overall trends were similar to those of other such studies [8–13].
The presence of the ≥3 metabolic syndrome components was associated strongly with stroke, as compared to the community and the hospital controls [14]. In our study, 11.46% patients had multiple risk factors [Table/Fig-2] and the outcome was poor in them. Similar observations were made by Pandian et al., (2005), wherein a 20% increase in the mortality was reported when multiple (combination of three or more) risk factors were present [11].
The risk factors may vary depending upon the cultural/ethnic background, as most of the risk factors are related to the lifestyles of the patients [12].
The clinical presentation of stroke depended upon the artery which was involved. Hemiplegia was the commonest presentation, which was similar to that in other epidemiological studies and it was the cause of a residual deficit and debility later in life [15–17].
The ICASS reported that up to 80 % of the strokes were ischaemic in nature [6]. Our study revealed that 71% were ischaemic strokes and that 29% were haemorrhagic strokes. Amongst the ischaemic strokes, 54 % had an anterior circulation infarct, 25% had a posterior circulation infarct, 12.5% had a basal ganglion infarct and 8.5% had bilateral periventricular infarcts. Most of the haemorrhagic strokes were basal ganglion bleeds. These observations were comparable to those of other similar studies which were done in Calcutta [12].
Sulter et al., (1999) defined a poor outcome when death/institutionalization due to stroke/ an MRS of >3 or a BI of <60 was reached [18]. Age, intracerebral bleeds, diabetes mellitus and cardiac disease were also poor predictors of the outcome in the study which was done by Lefkovitis et al., (1992) [19].
We also noticed that age, the male gender and the presence of multiple risk factors were poor predictors of the outcome.
The mortality in our study was 22.3%. The mortality which was reported in other such studies was 13.6 – 19 % [19, 20]. Amongst the patients with intracerebral haemorrhages (n=45) 65% of the patients expired. Similar results were noted in other studies also [20]. 49.7% of the patients had a significant residual deficit (an MRS of >3). In general, these findings were consistent with those of previous researches and they emphasized the necessity of developing interventions like Physical Therapy (PT) and Occupational Therapy (OT) for managing this residual illness [12,19,20].
Though, the window period for initiating the thrombolytic therapy for ischaemic strokes was recently widened from 3 to 4.5 hours [21], many of the patients with ischaemic strokes, who were otherwise eligible for intravenous thrombolysis, could not reach the hospital in the recommended time or the option was found to be more expensive. Still, being at home and the traditional treatment of stroke has been an accepted practice in the rural areas of this part of the country. Many strange culture specific beliefs about the stroke treatment have been prevailing, the most common one being the cure of paralysis by massaging with the fresh blood of pigeon.
Hence, public awareness programmes are needed to be undertaken, to educate the masses for them to recognize stroke and TIA at an early stage and for them to take the patients to the hospital as soon as possible, so that an efficient treatment can be initiated [21]. Also, people should know about the risk factors of stroke i.e. brain attack and they should take precautions for it just as for heart attack.
It is necessary to have an Indian “Fight-Stroke” Program that is specific for our needs [22].
The management of stroke requires skill that overlaps with several clinical specialties e.g. neurology, cardiology, clinical pharmacology, geriatrics, critical care, endocrinology etc. The training of other members of the stroke team can also be undertaken by encouraging the respective societies to co-ordinate their training program with the proposed stroke initiative [22].
Also, there is a need for prospective, representative population based surveys viz. stroke steps 2 and 31. Needless to mention, that ours was a recently established medical college in northern India. Therefore, a large data/sample size will be referred to in the days to come.