Laryngoscopy and tracheal intubation are nearly always associated with an increase in the blood pressure and an increase in the heart rate due to the reflex sympathetic discharge which is caused by an epipharyngeal and a laryngopharyngeal stimulation. This increased sympatho-adrenal activity may result in hypertension, tachycardia and arrhythmias [1].
Though these changes are well tolerated by healthy individuals, they may be fatal in patients with hypertension, coronary artery disease or intracranial hypertension. To ‘blunt’ this pressor response, various pharmacological agents have been tried, which include adrenergic blockers [2], vasodilators [3], calcium channel blockers [4] and lignocaine [5]. Various studies have shown that fentanyl is effective in blunting the pressor response to laryngoscopy and endotracheal intubation [6–10]. If a small dose of fentanyl which is administered 5 minutes before an intubation can prevent this haemodynamic response, it would be well worth it.
The purpose of this study was to compare fentanyl and clonidine for the attenuation of the pressor response to an intubation and to find the most favourable time for the administration of the same.
MATERIALS AND METHODS
A prospective study which involved 150 adult human patients was done. The patients were posted for routine surgical procedures at our institute after getting the approval of the institutional ethical committee. The patients were randomly allocated into three groups, with each group comprising of 50 patients; by using the Random Allocation Software v1.0.0. The power calculations suggested that a minimum of 17 subjects per group were required to detect a 10% difference in the arterial pressure between the groups (a = 0.05, b = 0.80). The patients in group-1 (control) were given normal saline and groups-2 and 3 were given i.v. fentanyl and clonidine respectively. All the patients were ASA-1 or ASA-II.
Inclusion Criteria: The patients who were in the age group of 20- 60 years, who were posted for elective surgeries, who belonged to ASA-1 or ASA-2, after excluding certain patients as per the exclusion criteria, on the basis of the history, clinical examination and relevant investigations.
Exclusion Criteria: The patients with ASA grades 3 and 4, with underlying cardiovascular disease, and the patients with a known hypersensitivity to these drugs.
Exclusion Criteria: The patients with ASA grades 3 and 4, with underlying cardiovascular disease, and the patients with a known hypersensitivity to these drugs.
The patients in group I (control) were given normal saline 4 ml IV over 30 seconds, beginning 5 min before the laryngoscopy. The patients in group 2 were given IV fentanyl 2 ;g/kg and group 3 was given IV clonidine 2 ;g/kg 5 mins before the laryngocopy. All the patients were premedicated with Inj.Midazolam and Inj.Glycopyrrolate 0.02mg/kg i.v.
All the patients were pre-oxygenated with 100% oxygen for 5 minutes. The induction was achieved with Inj. Thiopentone sodium 5mg/kg IV which was given in a 2.5% solution. Succinylcholine was administered at a dose of 2mg/kg IV. The patients were allowed to breath 100% oxygen via a face mask. When the patients’ breathing stopped, they were manually ventilated until the tracheal intubation was done. The laryngoscopy and the intubation were done within 15 to 20 seconds.
The patients’ heart rate, Systolic Blood Pressure (SBP), mean arterial pressure (MAP) and Diastolic Blood Pressure (DBP) were recorded as a preinduction control reading (0 min), immediately after the laryngoscopy (5min) and then after seven (7) minutes and ten (10) minutes. The data at each of the measurement points was compared and analyzed by using the analysis of variance (ANOVA) and the Student’s t test.
The patients who showed an undue pressor response in group – I (control) were administered injection fentanyl and inhalational anaesthetic agents to control the tachycardia and hypertension. These cases were not included in the study.
RESULTS
[Table/Fig-1,2,3,4,5,6,7 & 8]. All the groups were comparable in the age and gender distribution. There was no significant intergroup difference from the baseline.
Comparison of heart rate (bpm) between four groups of patients
| Group I | Group II | Group III | P value* | Diff. between groups** |
| Control | Fentanyl | Clonidine | I-II | I-III | II-III |
| 0 min | 78.34 ±14.34 | 79.06 ±10.52 | 77.18 ±10.01 | 0.219 | NS | NS | NS |
| 5 min | 116.2 ±18.43 | 101.14±15.01 | 86.88 ±10.00 | <.001 | <.001 | <.001 | <.001 |
| 7 min | 112.54±21.05 | 97.70 ±14.97 | 84.18 ±10.32 | <.001 | <.001 | <.001 | <.001 |
| 10 min | 100.32±15.73 | 88.12 ±16.25 | 77.84 ±11.10 | <.001 | <.001 | <.001 | <.001 |
Comparison of SBP (mm Hg) between groups
| Group I | Group II | Group III | P value* | Diff. between groups** |
| Control | Fentanyl | Clonidine | I-II | I-III | II-III |
| 0 min | 119.98±10.6 | 120.42±09.02 | 118.66±8.89 | 0.723 | NS | NS | NS |
| 5 min | 171.12±17.36 | 142.44±11.55 | 127.42±9.30 | <.001 | <.001 | <.001 | <.001 |
| 7 min | 157.72±13.97 | 132.36±13.26 | 118.08±13.7 | <.001 | <.001 | <.001 | <.001 |
| 10 min | 140.84±15.04 | 118.80±9.70 | 108.64±7.23 | <.001 | <.001 | <.001 | <.001 |
Comparison of DBP (mm Hg) between between groups
| Group I | Group II | Group III | P value* | Diff. between groups** |
| Control | Fentanyl | Clonidine | I-II | I-III | II-III |
| 0 min | 74.04±8.77 | 74.42±8.44 | 73.48±9.89 | 0.541 | NS | NS | NS |
| 5 min | 96.40±14.65 | 87.98±9.48 | 78.00±10.31 | <.001 | <.001 | <.001 | <.001 |
| 7 min | 90.30±10.71 | 79.16±11.39 | 72.46±8.82 | <.001 | <.001 | <.001 | <.001 |
| 10 min | 83.42±9.05 | 73.18±10.44 | 67.00±7.30 | <.001 | <.001 | <.001 | <.001 |
Comparison of MAP (mm Hg) between groups
| Group I | Group II | Group III | P value* | Diff. between groups** |
| Control | Fentanyl | Clonidine | I-II | I-III | II-III |
| 0 min | 89.35±8.44 | 90.36±9.23 | 88.54±8.34 | 0.611 | NS | NS | NS |
| 5 min | 121.31±14.26 | 106.13±8.78 | 94.47±9.03 | <.001 | <.001 | <.001 | <.001 |
| 7 min | 112.77±11.05 | 96.89±10.75 | 87.67±8.81 | <.001 | <.001 | <.001 | <.001 |
| 10 min | 102.56±10.04 | 88.39±9.59 | 80.88±6.32 | <.001 | <.001 | <.001 | <.001 |
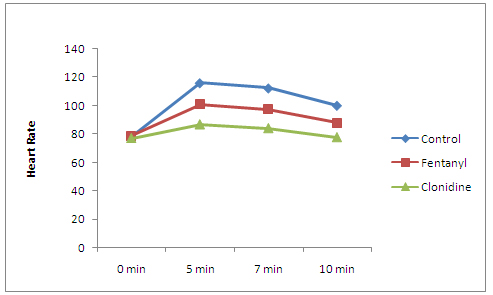
Heart Rate (HR): [Table/Fig-1], [Table/Fig-5]
Comparison of heart rate (bpm) between Groups
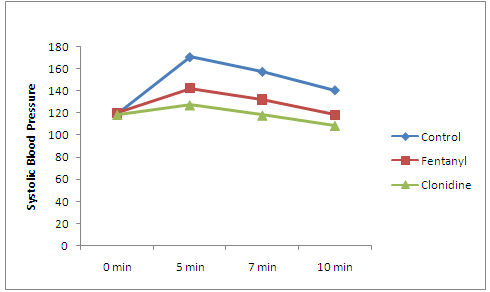
Comparison of SBP (mm Hg) between groups
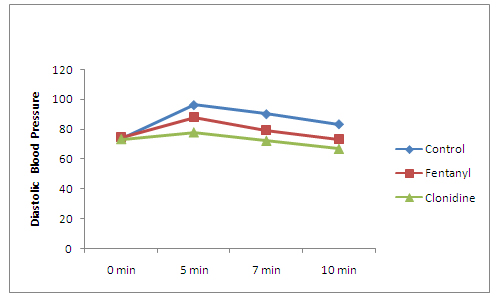
Comparison of DBP (mm Hg) between groups
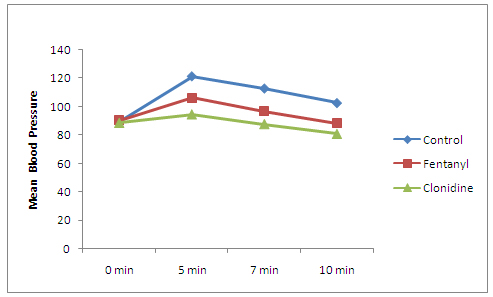
Comparison of MAP (mm Hg) between groups
One way ANOVA study showed significant variations in the heart rate before and after the induction and at time intervals of 5,7 and 10 minutes (P<.001).
The maximum increase in the heart rate was 48.07% (116.2±18.43) at 5 min in the control group and the minimum increase was 12.57% (86.88±10.00), which occurred immediately after the induction and the laryngoscopy (5 min) in the clonidine group. The difference in the heart rate between the clonidine group and the other groups remained statistically significant at all times of the assessment (P<.001) i.e at 5, 7 and 10 minutes.
Systolic Blood Pressure (SBP): The changes in the systolic blood pressure and their statistical comparisons have been presented in the [Table/Fig-2].
No significant variation was found at the pre induction in all the groups.A statistically significant difference was observed among the fentanyl and the control groups at the subsequent assessments (P<.001). The attenuation of the systolic blood pressure was better in the fentanyl group as compared to that in the control group. It returned nearer to the basal values earlier in the fentanyl group at 1.82% (118.80±9.70) below the baseline (120.42±09.02) than in the control group, which was 16.2% (140.84±15.04) above the baseline (119.98±10.6) at 10 minutes.
The attenuation of the rise in the systolic blood pressure was highly significant in the clonidine group. A rise of only 7.38% (127.42±9.30) was observed from its baseline (118.66±8.89) as compared to the 42.62% (171.12±17.36) increase in the control group from its baseline (119.98±10.6) (P<0.01), which occurred immediately after the induction and the laryngoscopy (5 minutes).
The attenuation of the systolic blood pressure was significant in the clonidine group as compared to that in the fentanyl group at 5, 7 and 10 minutes (P<0.001). A maximum rise of only 7.38% (127.42±9.30) was seen (P<0.001), and at 10 minutes, the systolic blood pressure which was recorded was 8.4% (108.64±7.23) lower than the basal value.
Diastolic Blood Pressure (DBP): The changes in the diastolic blood pressure and their comparative statistics are shown in [Table/Fig-3].
One way ANOVA showed no significant difference among all the groups at the preinduction level.
A significant difference was observed from the control in the fentanyl group (P<.001) at all the levels. The maximum rise was 18.22% (87.98±9.48) in the fentanyl group and it was 30.12% (96.40±14.65) in the control group at 5min. The suppression the maximum rise in the diastolic blood pressure by fentanyl was statistically significant (P<.001).
Clonidine was efficient in the attenuation of the diastolic blood pressure at all the time intervals i.e at 5, 7 and 10 minutes. It achieved 1.39% (72.46±8.82) and 8.8% (67.00±7.30) lower values than the basal value (73.48±9.89) at 7 and 10 minutes respectively. It was statistically highly significant as compared to all the other groups (P<0.001). The maximum increase in the diastolic blood pressure was 6.15% (78.00±10.31), which occurred immediately after the induction and the laryngoscopy (5 minutes).
Mean Arterial Pressure (MAP): The changes in the mean arterial pressure and their comparative statistics are shown in [Table/Fig-4].
One way ANOVA showed no significant difference among the three groups at the preinduction level.
A significant difference was seen in all the groups at 5, 7 and 10 minutes intervals (P<0.001).
A significant difference was observed from the control in the fentanyl group (P<.001) at all the levels. The suppression of the maximum rise in the diastolic blood pressure by fentanyl was statistically significant (P<.001). The maximum rise was 18.78% (106.13±8.78) in the fentanyl group and it was 35.77% (121.31±14.26) in the control group, which occurred immediately after the induction and the laryngoscopy (5 minutes).
Among the three study groups, clonidine was highly effective in attenuating the pressure response. Clonidine showed a 0.98% (87.67±8.81) decrease in the mean arterial pressure. But fentanyl showed a 8.43% (96.89±10.75) increase (P<0.001).
The attenuation of the pressor response by clonidine at all the levels i.e. at 5, 7 and 10 min as compared to the control and the fentanyl groups was highly significant (P<0.001). The maximum rise was 6.69% (94.47±9.03) in the clonidine group, whereas it was 35.77% (121.31±14.26) in the control group and 18.78% (106.13±8.78) in the fentanyl group.
DISCUSSION
The endotracheal intubation and laryngoscopy were associated with a rise in the blood pressure, heart rate and the cardiac dysarrythmias. These above mentioned effects may have serious repercussions on the high risk patients like those with cardiovascular disease, increased intracranial pressure or anomalies of the cerebral vessels. Attenuation of such responses is of great importance in the prevention of the perioperative morbidity and the mortality [15].
The haemodynamic response to laryngoscopy and endotracheal intubation has been a topic of discussion since 1940, when Reid et al., [16] found that the stimulation of the upper respiratory tract provoked an increase in the vagal activity. A year later, Burstein et al., [17], totally contradicting Reid’s statement, found that the pressor response was due to an augmented sympathetic activity which was provoked by the stimulation of the epipharynx and the laryngopharynx, which was further confirmed by Prys-Roberts.
A diversity of results exist about the protective measures against the haemodynamic and the catecholamine responses to laryngoscopy and intubation, but no single anaesthetic technique has become generally accepted as being effective in preventing or attenuating these responses. Many techniques have been recommended. The drugs which were used were either partially effective or they produced other undesirable effects on the patients [18].
In any study which is conducted, the criteria for the selection of the appropriate drug to prevent a sympathetic response must include the following. The drug must be applicable, regardless of the patient collaboration and it must prevent impairment of the cerebral blood flow and avoid the arousal of the patient. The administration of the drug should neither be time consuming nor should it affect the duration or the modality of the ensuing anaesthesia. Intravenous fentanyl and clonidine appear to best fulfil the above criteria [19].
Fentanyl is advocated for the attenuation of the sympathetic response to laryngoscopy and intubation. The blunting of the sympathetic response is dose dependent. Fentanyl at 6;g/kg, completely abolishes, while at 2;g/kg, it significantly attenuates the arterial pressure and the heart rate increase during laryngoscopy and intubation. The administration of fentanyl at the optimal time reduces the dose which is required. The optimal injection time of fentanyl is 5 minutes before an intubation, at a dose of 2;g/ kg [20].
The alpha-2 adrenoceptor agonists have been used as premedicants because of their beneficial properties in anaesthesia. The only clinically available alpha-2 adrenergic agonist in our country is clonidine, which is mainly used as an anti hypertensive agent, but it has many properties of an ideal premedicant and it also has beneficial effects on the haemodynamics during stressful conditions like laryngoscopy and endotracheal intubation. It was shown by Zalunrdo et. al., in 1997, that intravenous clonidine was better than oral clonidine in attenuating the pressor response [21]. Hence, in this study, intravenous clonidine was used. The effects of clonidine on the haemodynamic variables are dose related but they increase the dose to more than 4 mcg kg-1 and do not further enhance the efficacy. Hence, in this study, we used 2mcg/kg.
This study was undertaken to compare the effects of fentanyl and clonidine on the attenuation of the haemodynamic response to laryngocopy and endotracheal intubation.
The patients in all the groups did not show any statistically significant differences in their age or sex distributions.We selected the optimal age range of 20 to 60 years. This is because, the variability of the heart rate changes decreases with increasing age and younger patients show more extreme changes. The anesthetic technique was chosen such that the drugs which were administered did not have any significant effects on the heart rate or the blood pressure. All the groups were similarly premedicated regarding anxiolysis. At 0 min i.e., the preinduction values of HR, SBP, DBP and MAP did not show any statistically significant difference in all the three groups.
At 5 minute i.e., immediately after the laryngoscopy and intubation, the rise in the heart rate and the blood pressure was maximum in all the groups. The heart rate rise was 48.07%, 27.75%, and 12.57% in the control (I), fentanyl (II) and the clonidine groups (III) (p<0.001). This finding was in agreement with those of the studies which were done by Smith and Derbyshire et al., [22] and Shribman and Smith et al., [23], who concluded that the plasma catecholamine concentration increased to the maximum at 1 minute after the laryngoscopy. The rise was statistically highly significant within each group.
However, the clonidine group showed better attenuation of the HR as compared to the other 2 groups, which was statistically highly significant (P<0.001). Dipak and Malini have also reported the effectiveness of clonidine in the attenuation of the haemodynamic response to laryngoscopy and endotracheal intubation [24]. They found that the heart rate in the clonidine group returned to the basal value, 1 min after the intubation and that it remained lower than the basal value up to 5 minutes of the intubation. Its values were also statistically highly significant. The decrease in the pulse rate after the clonidine administration was due to the reduction of the sympathetic outflow, the simultaneous increase of the parasympathetic tone of central origin and the influence of clonidine on the neurons which receive the baroreceptor afferents (Sleight p et al.,) [25].
At 7 minutes, there was still a rise from the preinduction values of the heart rate and the blood pressure in all the groups. But the values showed a decline from those at 5 minutes, the decline being more rapid in the clonidine group. In the control group, the heart rate rise was 43.65%. In groups II and III, the heart rate decreased to 23.57% and 9% above the baseline respectively. This was in accordance with the findings of the study which was done by Shribman and Smith, which showed that the plasma catecholamine concentration came down by 3 minutes to 5 minutes after the laryngoscopy. This finding showed a statistically significant attenuation of the heart rate in the clonidine group (P<0.01).
At 10 minutes, the haemodynamic response declined in all the groups. The decline in the heart rate was significant in group III. Group I recorded a rise of the heart rate to 28.05%. In groups II and III, a rise of 11.45% and 0.86% respectively was recorded from the preinduction values.
Overall, the patients in our study showed a definite and a signifi- cant rise in the heart rate and the blood pressure in response to laryngoscopy and intubation. The clonidine premedicated patients showed a lower magnitude of the rise in the heart rate and the blood pressure. There was a statistically significant difference in the magnitude of the rise and the decline between the 3 groups. Both the blood pressure response and the heart rate were attenuated more effectively in the clonidine group as compared to those in the fentanyl group. This finding was in accordance with the data which was available from other studies, such as that from the study which was conducted by H. Talebi in 2010 [25].
In the control group, the systolic blood pressure increased maximally after 5 minutes (42.62%) and it gradually decreased over 10 minutes (17.39%). With the administration of fentanyl, the maximum increase as compared to the preinduction value was 9.91% and it was only 7.38% in the clonidine group. Both, when they were compared with the control, showed a significant suppression (P<.001), with the blood pressure response being attenuated more effectively by clonidine (P<.001). This finding was in accordance with the data which was available from other studies which were done by Michael Muzi et al. They suggest that this may be due to an active baroreflex response to the change in the pressures [26]. The maximum increase in the diastolic blood pressure was 30.12% as compared to the preinduction value in the control group (P<.001) at 5 minutes. It was 18.22% and 6.15% in the fentanyl and the clonidine groups respectively. The attenuation by clonidine was highly significant in contrast to the other groups (P<.001).
Similarly, the mean arterial pressure increased by 35.77% from the preinduction value in the control group at 5 minutes (P<.001) and it gradually decreased over 10 minutes. Fentanyl limited the maximum rise to 18.78% (P<.01), while clonidine limited it to only 6.69% (P<.001). The attenuation of the mean arterial pressure in the clonidine group was highly significant as compared to that in the fentanyl or the control groups (P<.001). This was in concordance with the findings of other studies, which showed that the preoperative administration of clonidine attenuated the stress-induced sympathoadrenal response to painful stimuli and that it improved the intraoperative haemodynamic stability. Sung et al., (2000) have also shown that a premedication with clonidine helped in providing a perioperative haemodynamic stability [27]. Moreover, Yokota et al., (1998) concluded that the clonidine premedication might contribute to a haemodynamic stability during a sedated fiberoptic nasal intubation [28]. Similar results were obtained in other studies (Costello and Cormack) [29]. Nand Kishore Kalra, in 2011 12, concluded that intravenous clonidine showed the best control of the systolic BP and no significant episodes of hypotension.
The results of the present study should encourage the routine use of clonidine as a premedication for the patients who undergo laryngoscopy and intubation. By providing improved haemodynamics, clonidine proved to be beneficial as compared to fentanyl in any clinical setup.
CONCLUSION
Based on the present clinical comparative study, the following conclusions can be made.
In the patients, with no drugs to attenuate the sympathetic response to laryngoscopy and intubation, the maximum increases in the heart rate and the systolic, diastolic and the mean arterial blood pressures were significantly high as compared to the preinduction values.
Clonidine significantly attenuated the sympathetic response to laryngoscopy and intubation.
Fentanyl also reduced the pressor response, but its effect was far lower than that of clonidine in attenuating the response.
This study showed that clonidine was superior to fentanyl in the attenuation of the pressor response and that the ideal time for its administration would be about 5 min before a laryngoscopy and an intubation.
An intravenous bolus dose of clonidine 2;g/kg which is administered 5 minutes before a laryngoscopy and an intubation can be recommended to attenuate the sympathetic response to the laryngoscopy and intubation without any side effects of the drug.