Laparoscopic Cholecystectomy (LC) is the accepted gold standard management for symptomatic gallstone disease since the past 2 decades. With the advantages of a shorter hospital stay, decreased post-operative pain and an early resumption of normal activities, this procedure has now become routine in the treatment of benign gallbladder disease in the general surgical units all over the world. A LC which is performed for benign gall bladder disease rarely results in a diagnosis of unexpected gallbladder cancer. The incidence of gallbladder cancer which is diagnosed during or after a LC has been reported to be between 0.19% to 3.3% at various centres [1–5]. From this study, we are reporting our experience with gallbladder cancer which was incidentally diagnosed during or after a LC which was performed for gallstone disease and cholecystitis.
MATERIALS AND METHODS
The medical records of the patients with symptomatic gallstone disease and acute or chronic cholecystitis who underwent LCs at the Hakeem Abdul Hameed Centenary Hospital during the period from January 2007 to June 2012 were assessed. A total of 622 laparoscopic cholecystectomies were performed at our institute during this period. Six histologically confirmed cases of adenocarcinoma of the gall bladder were identified by the retrospective analysis of the patient records of these 622 cases. The data on the age, sex and the presenting clinical features of these cases were retrieved from the accompanying laboratory request forms, or the patients file records wherever they were available. An abdominal ultrasonography was performed in all the patients. The ultrasonographic and the operative findings were also documented in each of these cases. The histology slides were reviewed and all the cases showed an evidence of adenocarcinoma, mostly in an early pathological stage. All the cases were incidental findings with no preoperative suspicion of a malignancy. The clinical presentation, pre-operative imaging, intraoperative findings and the histological features were analyzed and the results were compared with those in the literature.
RESULTS
This retrospective search of the medical records showed that a total of 622 laparoscopic cholecystectomies were performed at our institute during the study period of five and a half years. In [6] (0.96%) cases, incidental carcinomas of the gallbladder were discovered. The age distribution and the presenting clinical features of these six patients have been summarized in [Table/Fig-1].
Incidental Gallbladder Carcinoma : Age Distribution With Clinical Presentation

| S.NO | Age | Sex | Total (n=108) |
| 1 | 60 | F | Nausea ,Vomiting ,Acute cholecystitis x 10 days |
| 2 | 85 | F | Nausea, Vomiting, Chronic RUQ pain X 4 months |
| 3 | 30 | F | Nausea, Vomiting, Chronic RUQ pain X 2 years |
| 4 | 40 | F | Nausea ,Vomiting ,Acute cholecystitis x 7 days |
| 5 | 45 | F | Nausea, Vomiting,Jaundice, Chronic RUQ pain x 5 months |
| 6 | 58 | F | Nausea, Vomiting, Chronic RUQ pain X 3 months |
The age range was between 38 years to 85 years and all the six patients were females. Nausea, vomiting and pain in the Right Upper Quadrant (RUQ) of the abdomen was the common clinical presentation in all the six cases. One patient, in addition, also had jaundice of 3 weeks duration. Two patients presented with the features of acute cholecystitis, with a positive Murphy’s sign. In the remaining four patients, the symptoms were more chronic in nature and of a longer duration, which ranged from 3 months to 2 years.
A preoperative ultrasound was done in all the 6 cases and the significant findings have been presented in [Table/Fig-2]. The presence of multiple gallstones was the common feature in all the six cases and symptomatic gallstone disease was the indication for which these cases were taken up for surgery. The gallbladder was thickened (>3mm) in 4 cases [Table/Fig-1] and a pericholecystic collection was noted in one case. One case showed a dilated Common Bile Duct (CBD) but no stones were present in it. No mass lesion or polyp was seen in the gallbladder in any of these cases, on sonography. A fatty infiltration of the liver was an incidental finding in one case.
Incidental Gallbladder Carcinoma: Ultrasonographic Findings
| S.NO | Ultrasonographic Findings | Number of Patients (n=6) |
| 1 | Gall bladder stones, multiple | 6 |
| 2 | Thickened gall bladder wall | 4 |
| 3 | Pericholecystic collection | 1 |
| 4 | Dilated common bile duct | 1 |
| 5 | Fatty infiltration of the liver | 1 |
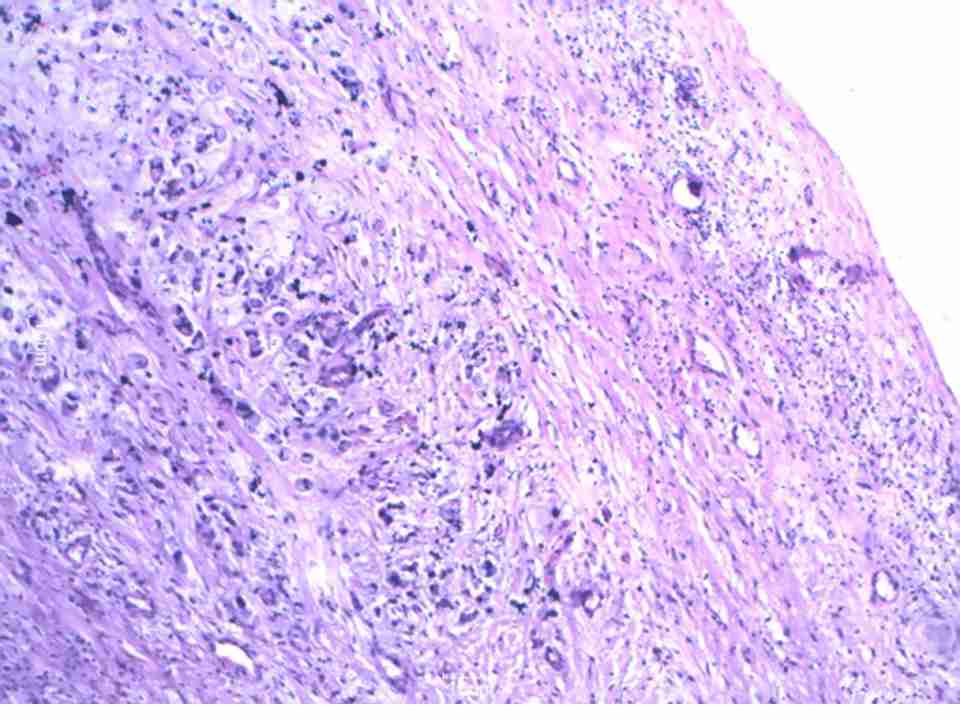
The per-operative and the histopathological findings which include the pathologic stages have been listed in [Table/Fig-3]. Case no 6 showed a distended thick walled gallbladder which was packed with multiple stones. The surgery was characterized by a difficult dissection of the Calot’s triangle due to the dense surrounding adhesions, which led to an intra-operative suspicion of a malignancy. Among the remaining five cases, there was no intra-operative suspicion of a malignancy, three of which showed thick walled gallbladders with calculi and in two cases, the wall was smooth, with multiple calculi. All the 6 cases were reported as adenocarcinomas of the gallbladder [Table/Fig-2]. The tumour staging was based on the 7th edition of the American Joint Committee on Cancer (AJCC) manual [6]. The pathological tumour stages were pT1a in three patients, pT1b in one patient and pT2 and pT3 in one patient each. None of the patients had pT4 disease or any evidence of metastases. Albores-Saavedra and co-workers first described the entity of an Intramucosal Carcinoma (IMC) in 1986, which corresponded histologically to pT1a of the AJCC classification [7]. IMC was an incidental microscopic finding in the cholecystectomy specimens and the tumour was confined to the expanded lamina propria, with no preoperative suspicion of a malignancy, as was seen in 3 cases in this study.
Incidental Gallbladder Carcinoma: Operative and Microscopic Findings with Pathologic Stage
| S.NO | Operative Findings | Pathology and Stage (Pt) |
| Case1 | Lap cholecystectomy. Multiple gallstones. Thick walled gallbladder. | Well differentiated adenocarcinoma(G1). Pathologic Stage: pT1a/Intra Mucosal Carcinoma |
| Case2 | Lap cholecystectomy. Multiple gallstones. Thick walled gallbladder. | Moderately differentiated adenocarcinoma(G2). Resected margin shows tumor involvement. Pathologic Stage: pT3 |
| Case3 | Lap cholecystectomy. Multiple gallstones. Adhesions between gallbladder and liver bed. | Moderately differentiated adenocarcinoma(G2). Pathologic Stage: pT2 |
| Case4 | Lap cholecystectomy. Multiple gallstones. Thick walled gallbladder. | Moderately differentiated adenocarcinoma(G2). Pathologic Stage: pT1a/Intra Mucosal Carcinoma |
| Case5 | Lap cholecystectomy. Smooth walled gallbladder with multiple calculi. | Well differentiated adenocarcinoma (G1). Pathologic Stage: pT1a/Intra Mucosal Carcinoma |
| Case6 | Lap cholecystectomy. Distended gallbladder with multiple gallstones. Dense adhesions & difficult dissection of Calot’s triangle.Suspicion of malignancy. | Poorly differentiated adenocarcinoma,(G3) signet ring cell type. Pathologic Stage: pT1b |
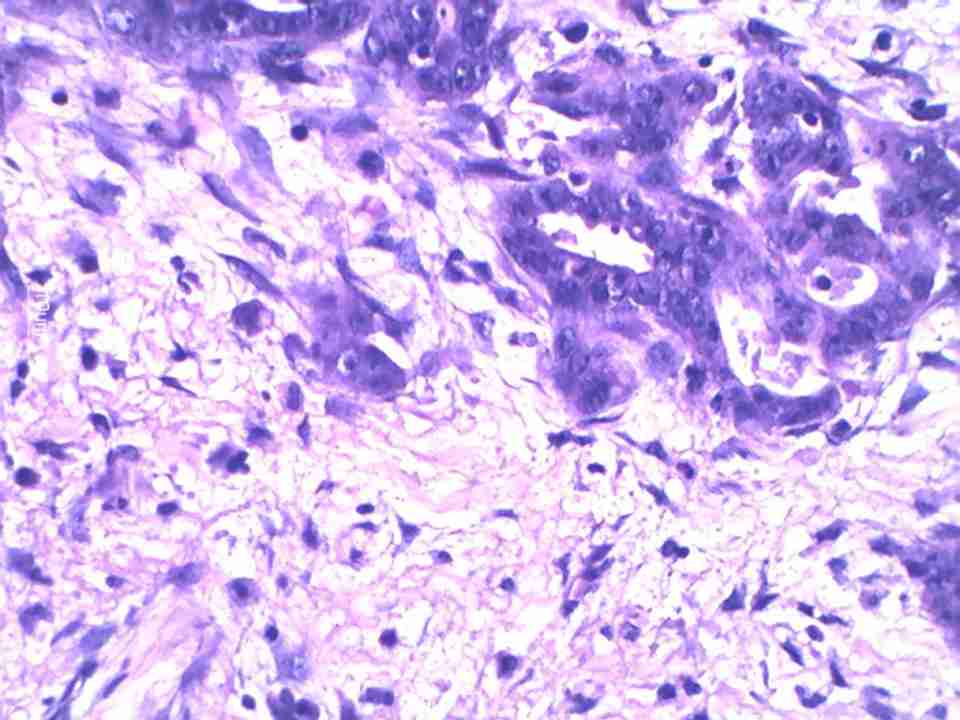
Case no 2 showed malignant glands which invaded the liver bed and the resected margin at the neck of the gallbladder also showed the presence of a tumour. Case no 6 was reported as a poorly differentiated adenocarcinoma of the gallbladder with infiltration of the muscle layer by the signet ring cells which were lying singly and in groups [Table/Fig-3]. After the histological diagnosis, all the 6 patients were referred to the local government oncology treatment centre for post-operative chemotherapy and further management. They were lost to further follow-up, except for case no 5 (pT1a), who was reported to be alive and well 5 months after the diagnosis.
DISCUSSION
Gallbladder Carcinoma (GBC) is the most common malignancy of the biliary tract and the sixth most common malignancy of the gastrointestinal tract worldwide [8]. It is an aggressive and a late symptomatic disease and most of the patients are treated at advanced stages. The prognosis is usually dismal and the 5 year survival rates have been reported to be less than 5% for the more advanced stages [9]. The countries with a high incidence of gallbladder cancer include Chile, Poland, India and Japan. A very high incidence of this cancer has been reported among women in northern India (21.5/100,000) and among female Native American Indians (14.5/1000,000) [10].
The early-stage carcinoma is typically diagnosed incidentally because of the inflammatory symptoms which are related to the coexistent cholelithiasis or cholecystitis. Incidental Gallbladder Carcinoma (IGBC) is the carcinoma of the gallbladder which is suspected for the first time during cholecystectomy or which is found on the histological examination of the gallbladder. With the increasingly widespread acceptance of LC and the difficulties in diagnosing GBC preoperatively, the number of cases of IGBC during and after LCs has increased. The female gender and advanced age are the demographic risk factors for GBC. All the six cases of the incidentally detected gallbladder carcinoma in this series were females and their average age was 53 years. A review of the literature showed that 0.19% to 3.3% of the patients who underwent cholecystectomies for presumed benign diseases were found to have carcinomas of the gallbladder [1-5] Tantia et al., in a study of LC cases from the Indian metropolis of Kolkata, reported an incidence of 0.59% of IGBC [2]. The present study which was based in New Delhi, India showed an incidence of 0.96% of IGBC among LC cases over a five and a half year period.
GBC either remains asymptomatic for a long time or it presents with very non-specific symptoms like pain in the abdomen, vomiting, anorexia, jaundice, a gallbladder mass and fever. In this study, two patients presented with the features of acute cholecystitis and four patients with chronic calculous cholecystitis. The association of GBC with cholelithiasis and chronic gallbladder inflammation is well known. The causes of the gallbladder mucosal inflammation include infection, drugs (such as isoniazid and methyldopa), congenital anomalies (such as choledochal cysts and the anomalous junction of the pancreaticobiliary ducts) and primary sclerosing cholangitis. It has been presumed that a longstanding chronic inflammation which is caused by cholelithiasis plays a role in the tumour progression and that carcinogenesis and gallstones are seen in 54-97% of the patients of GBC [11]. However, while most of the patients of GBC will have a history of cholelithiasis, only 0.3-3% of the patients with gallstones develop GBC. In this series, all the 6 patients who were detected to have IGBC had symptomatic gallstone disease for which LCs were undertaken. The other risk factors include a porcelain(calcified) gallbladder, a typhoid carrier state and gallbladder polyps [12]. Nakajima et al., reported a 45% risk of cancer for the polyps which measured greater than 15mm [13]. A more recent study in which gallbladder adenomas were analyzed in 91 patients, suggested a classification which was based upon the immunophenotype which was expressed, i.e. pyloric, intestinal, foveolar, and biliary and it indicated that these lesions played a minor role in the pathway of the gallbladder carcinogenesis [14].
The ultrasonographic findings in early stage GBCs are subtle, with considerable overlaps with the findings of acute and chronic cholecystitis. The features such as a thickened gallbladder wall, gallbladder or CBD stones, a gallbladder mass and a pericholecystic collection are not characteristic of GBC and they can be associated with cholecystitis. A pseudotumoural inflammatory condition of the gallbladder, xanthogranulomatous cholecystitis, is also known to radiologically simulate GBC [15]. Multiple gallstones were seen in all the 6 cases of IGBC in this series, along with thickened walls (> 3mm) in 4 cases. A pericholecystic collection was noted in one case of acute cholecystitis.
A difficult gallbladder at surgery usually raises the suspicion of cancer. Unusual findings at surgery such as a gallbladder mass, dense adhesions of the organs which are adjacent to the gallbladder and a difficult dissection of the gallbladder from the liverbed are all pointers to the presence of a possible malignancy, as was seen in case no [6]. A severe, destructive inflammation with adhesions is also an important feature of xanthogranulomatous cholecystitis and some series have also reported a simultaneous xanthogranulomatous cholecystitis and a GBC in a small proportion of the cases [16].
Gallbladder carcinomas are epithelial in origin and they account for 98% of all the gallbladder malignancies. Among these, adenocarcinomas account for 90% of all the carcinomas of the gallbladder. A majority (68%) are diffusely infiltrating, while the remainder exhibit intraluminal polypoid growth [17]. The submucosal spread of the infiltrating carcinomas appears grossly as focal or diffuse areas of wall thickening, nodularity or induration in the gallbladder wall. Similar gross features were seen in all the 6 cases of IGBC in this series and none of them showed any intraluminal growth or mass lesion. Because the flat infiltrating GBCs and the GBCs with cholecystitis and numerous stones are difficult to diagnose preoperatively, Yokomuro et al recommended taking frozen sections in that subset of patients who were of advanced ages (older than 70 years), who had a long history of stones, or those who had a thickened gallbladder wall [18]. However, Zhang et al., in their study, showed that frozen section was not a definitive diagnostic procedure and that it does not reliably measure the depth of invasion of the GBCs. One Histologically, all the 6 cases in this series were adenocarcinomas, with 3 cases in pT1a /IMC, and 1 case each in pT1b, pT2 and pT3. The pathologic staging was recognized as an important prognostic factor and a clinicopathological study of 13 cases of IMC suggested that a simple cholecystectomy was curative at this early stage, though a larger series with a long term follow up is necessary to validate this [19]. The authors recommended that the entire gallbladder be submitted for a microscopic examination and that at least 3 levels be obtained from each paraffin block which demonstrated a carcinoma, so as to be certain that the muscularis propria was not invaded. On the other hand, a re-exploration with a liver resection and a porta-hepatis lymph node dissection is a radical procedure which is carried out after further imaging, to rule out disseminated disease, which has proven to be beneficial in T2 and T3 gallbladder carcinomas which were first noted after laparoscopic cholecystectomies [20,21].
CONCLUSION
The incidence of IGBC in this single centre study was found to be 0.96%. Since, our hospital is a secondary care centre, the cases were referred to an oncology centre after the histological diagnosis of the malignancies for further treatment and hence, they could not be followed up for the assessment of the survival rates. The importance of a histological examination of the post-cholecystectomy specimens cannot be underestimated. The nonspecific clinical features and the sonographic findings of the early GBCs make the pre-operative diagnosis difficult and an IGBC has been recorded in every reported series of the LC cases. A meticulous microscopic examination of the specimen, with special attention to the depth of invasion, range of the mucosal spread and the lymphovascular involvement, is critical, as it determines the subsequent management of the case.