Renal transplantation is the preferred mode of therapy for the patients with end stage renal failure. Liver disease is a major problem in the renal transplant recipients. A mild hepatic damage which is manifested by an increase in the serum transaminases is common after an exposure to infectious agents, but it maybe transient and it generally does not progress to a clinically apparent disease [1].
Various liver lesions in the renal transplant recipients are considered to be a consequence of the transplantation protocol, which include immunosuppression, drug toxicity, alteration of the immune response to viruses and haemodialysis [2]. Transplantation is, therefore, a therapeutic procedure with side effects like hepatitis [3].
The progressive cholestatic syndrome which is caused by bile duct damage and loss has been seen in renal transplant patients with HCV infections due to the anti-HCV antibodies [4]. This study was conducted with the aim of studying the biochemical parameters and of assessing the liver damage on histopathology among the renal transplant recipients with both the HBV and the HCV infections and to correlate them. It was also attempted to check whether the serum enzymes could be used to predict the histological changes.
MATERIALS AND METHODS
The study group comprised of thirty cases. The enrolment criteria included a coinfection with HBV and HCV, as was evidenced by a positivity for the Hepatitis B Surface Antigen (HBsAg) and the anti HCV antibodies; elevated liver enzymes and recipients of renal allografts. A detailed clinical history was taken and a physical examination was carried out.
All the patients were on pretransplant dialysis at least twenty times. The liver function tests which included alkaline phosphatase, SGOT, SGPT and serum bilirubin levels were carried out by using automated equipment. The percutaneous liver biopsies were carried out by using a Menghini’s needle in all the thirty patients.
The staining methods which were performed on the biopsy slides included hematoxylin and eosin (H and E), van Gieson, reticulin and Perl’s staining methods. The histopathological grading was performed by using the Metavir Scoring System [5]. Immunohistochemistry (IHC) was done wherever it was required, to delineate the ground glass hepatocytes.
The biochemical and the morphological changes in the post-transplant cases were compared with those in the ten patients who were HBC and HCV positive but had not undergone renal transplants.
RESULTS
A total of 30 patients were observed and investigated. The men outnumbered the women in this study. There were 26 males and 4 females. The ages of the patients ranged from 22 years to 50 years. The maximum incidence of the transplants was in the age group of 26 to 30 years (43%) and the least was in the 20 to 25years age group (3.3%).
The leading cause of end stage renal disease was chronic glomerulonephritis. Twenty nine patients received kidneys from live donors and there was one cadaveric transplant. A retransplantation was carried out in one patient who developed acute tubular necrosis. A pretransplant dialysis was carried out in all the patients with an average of 13 peritoneal and 16 haemodialysis.
A history of alcohol intake was positive in 20 cases, with 3 patients giving a history of a heavy intake and the rest being social drinkers. All the patients in the study group discontinued the alcohol intake prior to the transplant after undergoing due counselling.
The transplant patients were put on a regime which comprised of azathioprine, cyclosporine, prednisolone and interferon. The average time span between the transplantation and the liver biopsy was 2.13years.
Three patients were positive for the HBV and the HCV markers prior to the transplants and 27 turned positive within 6 months of receiving the transplants. All the controls were HBsAg and HCV positive, with increased enzyme levels and a clinical evidence of jaundice, but they had not received renal transplants.
Metavir Grade 3 biopsy ( H&E; 40X)

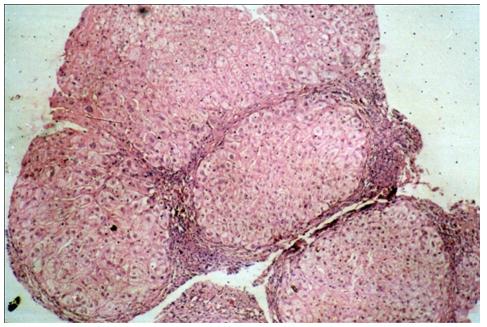
Metavir Grade 4 biopsy ( H&E; 40X)
The SGPT levels were marginally increased in 36% of the study group. A more than 2 fold increase was seen in 64% patients. The controls showed more than a 4 fold increase in the SGPT levels, both in grades 2 and 3. Likewise, the SGOT was marginally increased in 40% patients, with 60% showing more than a 2 fold increase. The controls manifested a 4 fold increase in grades 2/3 and a 2 fold increase in grade [1].
Eight of the 30 patients (26.6%) showed an increase in the alkaline phosphatase levels, which ranged from 175 to 475 IU. Only two of the ten controls showed a marginal increase.
The serum bilirubin levels were normal in 93.3% of the study group. Only 2 patients showed a marginal increase, while 8 controls showed a marked increase in the serum bilirubin levels, having clinically reported with jaundice.
The histopathology was assessed on H and E stained slides, which was supplemented by the reticulin and the van Gieson stains wherever they were required. The grading was carried out by the Metavir Scoring System. One case had a score of 0, 10 were graded as 1, 12 were in grade 2, 2 were in grade 3 and 1 was in grade [4]. One patient had established cirrhosis. Immunohistochemistry was done for seven cases in which ground the glass hepatocytes were ambiguous on the H and E slides. Four of these were positive for the membranous HBsAg.
The incidence of the chronicity in the study group (Metavir grades 2 and above ) was found to be 53.3% in our study.
A correlation of the SGOT, SGPT and the alkaline phosphatase levels of the study group and the controls was carried out with the grading. The paired “t” test at 5% and a test of probability was carried out. There was no statistically significant correlation between the controls and the transplanted patients. It was further surmised that though the serum enzyme levels could be used to predict the histological grade in the control group, the same could not be done in the transplant recipients (p>0.05).
DISCUSSION
The patients with end-stage renal disease are at high a risk for the HBV or the HCV infections. A liver biopsy is necessary for the assessment and the correlation with the biochemical and the virologic parameters before the institution of the therapy [6].
Further, the chronic HBV or the HCV infections are no longer hurdles in the way of the kidney transplantation due to the advances in the antiviral therapy. The pretransplant patients without a bridging fibrosis on the liver biopsies or the clinical stigmata of cirrhosis, are taken up for the kidney transplantation due to their superior survival [7].
The present study was done retrospectively to assess the biochemical and the morphological changes in HBV and HCV infected post renal transplant recipients and to evaluate the correlation between the two. In our study, 3 patients had serological evidences of the HBV and the HCV infections along with abnormalities of the liver function prior to the transplant and 27 developed the same 1 to 2 years later. This differed from the study which was conducted by Freiberger et al., wherein abnormalities of the liver function were detected 3 to 11 months post transplant [8]. The studies which were done on the coexistence of the Hepatitis B and C infections in kidney transplant recipients had found a prevalence of 9% [9].
We found a male predominance in our study (85%), which was seen in previous studies as well [10].
Fourteen of our patients were between 20 to 30 years and 6 were between 41 to 50 years. We screened 9 variables for the progression to cirrhosis, of which, an older age at transplant and a Metavir grade of 2/3 were found to be significant (p<0.05). Additionally, the female patients also exhibited an increased risk for developing cirrhosis in the post transplant period (p<0.1). The earlier studies had found the male sex, the duration of the haemodialysis, HBsAg, HBeAg and antiHCV and the pretransplant abnormal liver function to be significantly related to the development of a chronic liver disease after the transplant [11]. We found the occurrence of the chronicity in the study group (Metavir grades 2 and above ) to be 53.3% in our study. The prevalance of chronic liver disease was found to be to the tune of 40% in the renal transplant recipients with both the infections [9]. It has also been quoted in the literature that advanced chronic liver disease after a transplant, could be a viral cause which was complicated by immunosuppression [12,13].
We did not find a statistically significant correlation between SGOT, SGPT and alkaline phosphatase and the histological grading in the study group, though the enzyme levels could be used to predict the histological grades in the control group. The former was in agreement with the findings of previously conducted studies [10].
We found no significant difference in the levels of SGOT, SGPT , alkaline phosphatase and bilirubin in the various Metavir grades. This was in agreement with the findings of previously conducted studies [10].
CONCLUSION
To conclude, it was surmised that a majority of the post renal transplant recipients with the Hepatitis B and C virus infections had increased serum transaminases with histological evidences of liver damage. However, there was no correlation between the histological grades and the biochemical parameters. The latter, therefore, cannot be used to predict the histological picture and the clinical outcome thereof in such cases.