Tuberculous Meningitis (TBM) remains an important cause of morbidity and mortality, especially in the developing world, where it accounts for 7-12% of the tuberculosis cases [1]. TBM most commonly affects the children who are in the first three years of life, but it also affects adults, especially HIV positive patients. The laboratory methods play a crucial role, as an early treatment with the Antitubercular Drug (ATT) has been shown to improve the clinical outcomes of the patients and a delay in the diagnosis is directly related to the neurological complications [2].
The diagnosis of TBM depends on radiological and conventional methods like Ziehl Neelsen (ZN) staining of the acid fast bacilli and culture. Often, the clinical and radiological features mimic other causes of meningoencephalitis, thus making the diagnosis difficult. ZN staining is rapid and cheap, but it is neither sensitive (0-20%) nor specific and it requires a minimum bacillary load of 104/ml, which is difficult, as the CSF sample is mostly paucibacillary in nature [3].
Auramine phenol staining is more sensitive than ZN and the smears can be examined at a lower magnification. Thus, a larger area can be covered in the same time.
Culture is more sensitive than the ZN staining with a detection limit of 10-100 bacilli/ml, but it requires a prolonged incubation time of 6-8 weeks due to the long generation time of the tubercle bacilli [4]. The various other diagnostic modalities include the adenosine deaminase assay [5], radioimmunoassay [6] and ELISA [7], which detect the mycobacterial antigen and its antibody in the Cerebrospinal Fluid (CSF). These techniques are less sensitive and they need improvization. A lack of adequate sample volumes, the non uniform distribution of the microorganisms and the lack of an effective sample processing technique are the other noted problems which are associated with the diagnosis of TBM.
Many newer diagnostic modalities like automated microbial detecting systems and molecular methods have come up, which provide an increase in the isolation rate and an early detection of the organism. BacT/ALERT is based upon the colourimetric detection of the pH change which occurs due to the CO2 production by the mycobacteria [8].
Not many studies have evaluated the diagnostic potential of BacT/ALERT for tuberculosis (TB), especially for TBM. IS6110 is a transposone which is present as multiple repetitive elements in the genome of the M. Tuberculosis Complex (MTBC). It is present in variable copy numbers from 0 to 26 in the MTBC strains [8].
MATERIALS AND METHODS
The present study was carried out in the Department of Microbiology, Meenakshi Medical College and Research institute, Tamilnadu, India, during July 2010 to May 2012. Ethical clearance was obtained from the ethical committee of the college. An informed consent was taken from the patients. The patients were divided into cases and controls. Cases- 47 CSF samples were collected from suspected cases of TBM according to the criteria which were proposed by Ahuja et al .,[9].
The criteria were: A) Clinical: Fever and headache which lasted for more than 14 days.
A) Cerebrospinal fluid changes: Pleocytosis with predominantly lymphocytes, ↑protein and ↓sugars level.
C) Radiological: CT studies of the head which showed 2 or more of the following: exudates in the basal cisterns or in the Sylvian fissures, hydrocephalus, infarcts and a gyral enhancement.
D) Extra neural tuberculosis: As was evidenced by appropriate radiological or microbiological tests or by the presence of a caseous necrosis on histopathological examination.
The 4 sub criteria which have been described above were incorporated into the 4 groups in the descending order of sensitivity.
Definite TBM: (i) Clinical criteria (A) (ii) Bacterial isolation from CSF or diagnosis at autopsy.
Highly probable TBM:Clinical criteria (A)
All 3 of (B), (C), (D).
Probable TBM:Clinical criteria (A)
Any 2 of (B), (C), (D).
Possible TBM:Clinical criteria (A)
Any 1 of (B), (C), (D).
Controls-Thirty three control patients were chosen, who were admitted for pyogenic meningitis.
Approximately, 2ml of CSF was collected aseptically from each patient by lumbar puncture for testing by smear and culture, BacT/ ALERT and nested PCR.
Smear and culture: Staining by Ziehl–Neelsen’s technique and the Auramine phenol method for acid fast bacilli and cultures on the Lowenstein – Jensen (L-J) egg based medium were carried out as per the standard methods [10].
BacT/ALERT: The processing of CSF for M. tuberculosis was done on a Biomerieux BacT/ALERT instrument as per as the manufacturer’s instructions [11]. The inoculated BacT/ALERT MP bottles were loaded in a MB/BacT instrument for incubation and the growth was monitored. The BacT/ALERT MP bottle which was positive for the growth of M. tuberculosis produced a colour change in the sensor from dark green to a lighter green or yellow, thus changing the screen colour to yellow. The positive BacT/ ALERT MP bottles were unloaded and vortexed heavily to break the larger clumps to and to suspend them uniformly. The presence of mycobacteria was confirmed by performing ZN staining of the fluid.
The nested polymerase chain reaction: Nested PCR was carried out as per the method which was described elsewhere [12]. The sediment of the centrifuged CSF was added to 50 μl of lysozyme, followed by an overnight incubation. 70 μl of 14% SDS and 6 μl of Proteinase K were added and the mixture was incubated at 650C for 15 minutes. Subsequently, 10 μl of 5M NaCl and 80 μl of 10% CTAB (which was activated at 550C) were added and the mixture was incubated at 650C for 10 minutes. Then, 800 μl of a phenol, chloroform and iso amyl alcohol mixture was added in a ratio of 25: 24: 1, it was centrifuged and the supernatant was added to 600 μl of ice cold isopropanol. This was incubated overnight and centrifuged. After drying, 20 μl of Tris buffer was added to the sediment and it stored at -200C.
The primers were validated by blasting the primer sequence which was used for the detection of M. tuberculosis in the genome database of all the organisms at the web site, (http://www.ncbi.nlm. nih.gov/blast) and they were found to be specific for the organism. The sequences of the TB PCR primers were: for the first set conventional PCR round- forward primer (FL): 5’ CTC AAG TGA AGG AGG CAA CC – 3’ and for the reverse primer (FR): 5’ TGG GCT AGG GTG TTG ATC TC – 3’, where as for the nested PCR: for the forward primer (NFL): 5’ CGT CTG GAG CGT GAC CTA CT – 3’ and for the reverse primer (NFR): 5’ GAC ATC TCG ACG GTC AGT CA – 3’ respectively. The PCR mix consisted of 4μl of the extracted DNA, 10 μl of the 2X readymade master mix, 2μl of the 10μM primer (FL and FR for the 1st round of PCR and NFL and NFR for the nested PCR) and 10μl of milliQ water.
The settings of the thermocycler which were programmed, were similar for both the first round and the nested PCR, except for the primers which were used. A total of 30 cycles were carried out in each round and each cycle comprised of an initial denaturation at 94°C for 5 minutes. The denaturation occurred at 94°C for 60s, annealing occurred at 56 °C for 60s and the amplification occurred at 72 °C for 60s, followed by a final extension at 72 °C for 7 min .
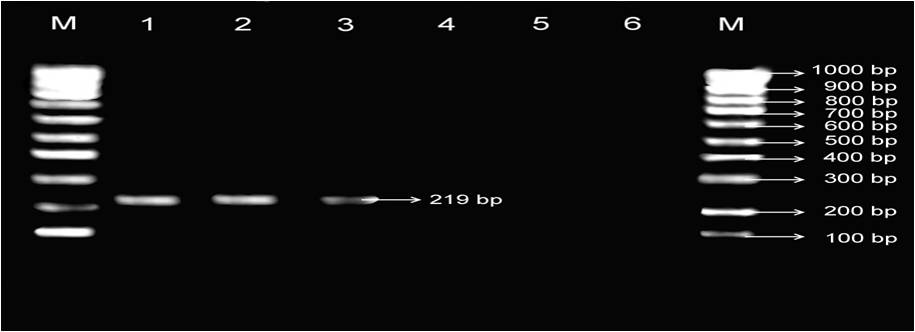
Agar gel electrophoresis was carried out and the bands were visualized under UV rays. The MTB specific nested PCR product size was 219 bp. The bands were separated in the agarose gel according to their molecular weights, which were then checked by comparing them with standard molecular weight markers.
STATISTICAL ANALYSIS
A descriptive statistical analysis was carried out. The results of the continuous measurements were presented as mean ± SD (Min- Max) and the results of the categorical measurements were presented in number (%). The Chi-square/ Fisher Exact test was used to find the significance of the study parameters on a categorical scale between the 2 groups. The 95% confidence interval was computed to find the significant features.
RESULTS
The cases and the controls were age and gender matched, with p values of 0.689 and 0.888 respectively. Fever was the most consistent finding, followed by headache, weight loss and night sweat. The microbiological findings of the various tests have been depicted in [Table/Fig-1]. Acid fast microscopy which was done by both the ZN and the AP staining was found to be negative in all the cases, whereas the culture on the LJ medium showed a 3.22% sensitivity.
Microbiological tests among various subgroups of tuberculous meningitis (TBM)
| Sub groups | No of cases | Number of cases positive for M. tuberculosis by |
| Zn staining | AP staining | LJ culture | BacT/ALERT | Nested PCR |
| Total cases | 62 | 0 | 0 | 02 | 16 | 25 |
| Confirmed TBM | 2 | 0 | 0 | 02 | 02 | 02 |
| Highly probable TBM | 19 | 0 | 0 | 0 | 8 | 12 |
| Probable TBM | 26 | 0 | 0 | 0 | 5 | 09 |
| Possible TBM | 15 | 0 | 0 | 0 | 1 | 02 |
| Control | 33 | 0 | 0 | 0 | 0 | 01 |
BacT/ALERT showed a sensitivity of 25.80% (16 out of 62 cases were positive) and a specificity of 100%. The contamination rates of BacT/ALERT and the LJ culture in the present study were found to be 5.8% and 7.2% respectively. The mean detection time of BacT/ALERT in all the seven isolates was 20.68 days as compared to 31.28 days of the LJ culture. The gel image after the nested PCR targeting IS6110 of M.tuberculosis has been shown in [Table/Fig-2]. The nested PCR showed an overall sensitivity of 40.32% (25 out of 62 cases were positive), which was 100.0% in the confirmed group and it gradually decreased in theother groups. Overall, the diagnostic accuracies of BacT/ALERT and nested PCR were 51.58 % and 60.0% respectively.
Gel image after nested PCR targeting IS6110 of M. tuberculosis
• Lane M : 100bp DNA ladder, Lane 1 : 219bp PCR product of positive control,
• Lane2&3: 219bp PCR product of clinical sample positive for IS6110 of M.tuberculosis,
• Lane 4 to 6 : Clinical samples negative for IS6110 of M.tuberculosis
DISCUSSION
The accurate laboratory diagnosis of TBArt still continues to be a challenge. An early and a prompt diagnosis of this condition contributes to early start of the anti tubercular therapy and prevention of the complications which are caused by this condition.
In the present study, the low sensitivity of the AFB microscopy can be explained on the basis of the paucibacillary nature of CSF. A high bacterial load (>104-105 bacilli/ml) is needed in the specimen, to render an AFB microscopy result positive [5]. Various studies documented similar sensitivities of the smear microscopy for TBM, which ranged from 0-20% [2,13–14]. AP staining, though it has been claimed to be more sensitive than the ZN staining [15], in the present study, we could notice no signifi- cant differences. The sensitivity of the culture on the LJ medium (3.22%) was similar to that which was found in various other studies (2-8%) [13–14] . This could be due to the pacibacillary nature of the CSF (the minimum detection threshold being 10-100 bacilli per ml) or due to the presence of dead bacilli [8].
The BacT/ALERT microbial detecting system showed an overall sensitivity of 25.80% , which was definitely higher than that of the LJ culture (p 0.001) and a specificity of 100%. A higher sensitivity was found in the confirmed subgroup, but it had fallen down in the other subgroups. Of the 16 mycobacterial isolates which were recovered in our study, all (100%) were recovered by BacT/ALERT as compared to the 12.5 % (two isolates) recovery rate of the LJ culture. Other studies also have shown recovery rates of 91% to 94% of BacT/ALERT [16–17]. The contamination rates of BacT/ALERT and the LJ culture in our study were found to be 5.8% and 7.2% respectively. Similar reports have been documented in different studies [16]. The mean detection time of BacT/ALERT in all the 16 isolates was 20.68 days as compared to 31.28 days which were taken by the LJ medium. Various studies documented a mean detection time of 15-16 days for BacT/ ALERT [16–17]. The early detection of the bacilli in these studies could be due to the inclusion of both pulmonary and extrapulmonary specimens in these studies. The earlier isolation of the AFB by BacT/ALERT substantiates its role for an early start of ATT and also to perform the antitubercular susceptibility testing.
In the present study, nested PCR showed an overall sensitivity of 40.32 %, which was higher than that of the culture (p<0.001), but it gradually decreased in the confirmed (100%), highly probable (63.16%), probable (34.62%) and the possible (13.33%) subgroups. Comparable results were found in different studies. In a study which was done at AIIMS, India, by Ahuja et al, who had formulated this criterion, the sensitivities which were documented were 85.71%, 75% and 33.33% in the highly probable, probable and the possible subgroups respectively [9]. Brienze et al., had reported sensitivities of 53%, 50%, 7% and 8% in the confirmed, highly probable, probable and the possible subgroups respectively [13]. The differences in the sensitivities could be due to the use of the MBP 64 nested PCR.
In our study, there were 37 cases which could not be detected by nested PCR (false negative results).
The Reasons for the Lower Sensitivity May Be Many: Firstly, the presence of PCR inhibitors which are found to be more associated with the extrapulmonary specimens as compared to the pulmonary specimens [18–19]. A better extraction procedure like an immunomagnetic separation technique may be used to capture all the M. tuberculosis DNA, but not the inhibitors [18]. Various resin matrixes like ‘Gene releaser preparations’ which absorb the inhibitors without entailing a further loss of DNA may also be used [18]. Secondly, there is a poor lysis of mycobacteria in the extraction procedure due to the complexity of the cell wall [20]. Thirdly, some strains of M.tuberculosis in Asia lack the IS6110 sequence [21–23]. Hence, few of the cases in the present study may have gone undetected if the mycobacteria which were present in these samples lacked the IS6110 sequence. Fourthly, there was a nonuniform distribution of the microorganisms. The use of a single Universal Sample Processing (USP) technique which used the USP solution for smear microscopy, culture and PCR could obviate the dividing of the samples into different parts. It was found that by following the USP technique, the sensitivities of all the tests could be increased [24]. Fifthly, the inability in concentrating the sample (due to less volume). The volume of the sample is of great significance in PCR, especially in TBM, due to low number of bacilli in the sample. When culture, staining, BacT/ ALERT and PCR have to be done, the minimum volume of the sample should be 5-6 ml. Sixthly, the sensitivity also depends on the procedure of processing of the sample. Haldar et al., had depicted that the filtrates of CSF contain a substantiate amount of the mycobacterial DNA as compared to the sediments and that the PCRs which targeted IS6110 and devR were more sensitive in the CSF filtrates compared to the sediments [2].
The overall specificity of nested PCR in our study was 96.97%. The reasons for the false positive results could be cross contamination during the initial handling or an amplicon carry over contamination, which can be overcome by using a single tube nested PCR [18]. It was also found that the use of dUTP/Uracil- N-glycosylase could decrease the amplicon contamination [18].
Twenty Three cases which were detected by nested PCR were rendered negative by the LJ culture. The gain in the sensitivity (37.1%) over the so called “gold standard” can be explained by the low detection limit of the nested PCR, of as few as 10 bacilli per ml [25]. The sensitivity gain in the aetiological diagnosis and the high PPV and NPV of nested PCR substantiate the diagnostic utility of this method. Moreover, nested PCR offers the advantages of a speed in obtaining the results and the option of referring the sample rather than the patient to a specialized centre [26–27].
In conclusion, the diagnosis of TBM is often difficult due to the atypical clinical presentation and the paucibacillary nature of the sample. Nested PCR was found to be more sensitive, followed by BacT/ALERT as compared to the conventional LJ culture and smear microscopy. BacT/ALERT is more sensitive, it takes lesser time to detect the growth and it is associated with a lesser contamination rate as compared to the conventional LJ culture. We suggest that nested PCR deserves a place in the laboratory diagnosis of TBM, but a careful adherence to the test protocol is mandatory. As both false negative and false positive results are reported on PCR, PCR alone should not be used as a criterion for initiating or terminating the therapy. It should be supported by clinical, radiological, cytological and other microbiological findings (smear microscopy and culturing by conventional and automated systems) for guiding the clinicians in the decision making for the appropriate therapy, whenever it is possible.