Introduction
The Human Immunodeficiency Virus (HIV)/Acquired Immunodeficiency Syndrome (AIDS) is one of the most feared infectious diseases of the late 20th century. Since its discovery in 1981, AIDS has emerged as a global health problem of extraordinary proportions and an unprecedented emergency. Thirty years after its discovery, the virus has reached virtually every corner of the globe, making a profound impact on contemporary medical practice, public health priorities and on every aspect of modern society.
The latest statistics of the global HIV and AIDS epidemic published by UNAIDS, WHO and UNICEF in Nov 2011 estimated that 34 million people were living with HIV/AIDS [1].
India has a large number of patients with AIDS, which is the third largest population of this group in the world. According to a report which was made by the National AIDS Control Organization, it has now been estimated that around 2.39 million people in India are living with HIV [2].
HIV causes a wide spectrum of diseases and it is undoubtedly a multisystem disorder, but the ophthalmic disease does affect 70-80% of the patients with HIV infection sometime during the natural history of their infection. Various studies have demonstrated that 40-45% of the HIV infected patients do have some or the other ophthalmic manifestations when they are examined by an ophthalmologist [3]. The spectrum of the HIV associated ophthalmic disease is very broad and it ranges from adnexal disorders to posterior segment disorders, including the optic nerve and the optic tract. These ocular manifestations can be the presenting signs of a systemic infection in an otherwise asymptomatic individual. The sequelae of HIV infection increases as immunocompetency decreases. While the asymptomatic ocular lesions occur in the earlier stages, the relentless destructive and blinding infections, especially the opportunistic ones occur in the later stages of the disease.
Since the first report on the ocular manifestations of AIDS which was made by Holland et al., in 1982 [4], subsequent studies have described several AIDS related conditions in the eye and the orbit [3,5]. Ocular manifestations of HIV in India was first reported in 1995 [6]. Since then, the number of HIV patients has greatly increased. The estimated prevalence of HIV related eye diseases in India is reported to be between 8-45 % [5-9].
The Government of India launched a free public sector ART initiative in 2004 and the access to ART is steadily increasing over the years. The ART Centre at District Hospital, Hassan, Karnataka, was set up in 2006. Patients with HIV/AIDS, who had registered at the ART Centre, were referred to the Ophthalmic OPD for a complete ocular examination. An epidemiological study of these patients was conducted in order to analyze the prevalence and the nature of the ocular lesions and their effect on the vision in HIV infected/AIDS patients from Hassan district.
Materials and methods
This study was undertaken at Hassan Institute of Medical Sciences, Hassan, Karnataka, India, from Jan 2008 to Feb 2012, after obtaining the institutional ethical committee’s clearance. A case proforma was made and a written informed consent was obtained from all the patients. 553 patients with HIV infection/AIDS, who were referred to the Ophthalmic OPD from the ART Centre at Sri Chamarajendra District Hospital, were included in this study. The patients who belonged to all the age groups, those with both high and low CD4 counts and the patients who were in the asymptomatic carrier state to those with full blown AIDS, were included in the study. These patients were evaluated, irrespective of the presence or absence of ocular symptoms and their treatment status (pre ART and ART).
A complete ocular examination of both the eyes was done, which included the assessment of the distant visual acuity by using Snellen’s chart and near vision assessment which was done by using Jaeger’s chart. Refraction was done and the best corrected visual acuity was estimated. Colour vision was assessed by using Ischihara’s chart. Anterior segment examination was done by using a slit lamp biomicroscope and the intra ocular pressure measurement was done. Fundus examination was done by using an indirect ophthalmoscope and +90D biomicroscopy. Standard 45 degree fundus photographs were taken in the presence of posterior segment findings. Attention was given to the presence of any lid retraction and pupillary abnormalities. These patients were followed up every 3 months. Early follow up was indicated in the presence of ocular manifestations, the presence of ocular symptoms and in those with low CD4 counts. However, most of the patients were inconsistent or lost for follow up.
Statistical Analysis
A descriptive analysis was done by using the SPSS +17.0 computer package for statistics. The variables of interest in our study were age, gender, visual acuity and the ocular findings. The results were expressed in terms of proportions.
Results
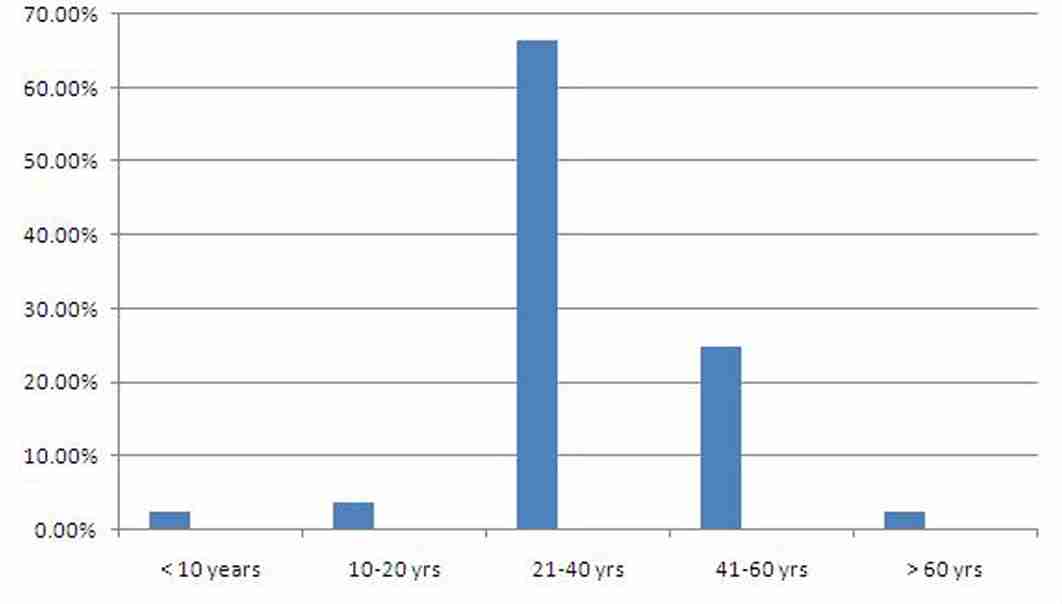
Of the 553 patients who underwent a complete ophthalmic examination, 299(54%) were males and 254 (46%) were females. A majority of the patients ie. 367(66%) were aged between 21-40 years and 138(25%) were in the age group of 41-60 years. 14 patients(2.53%) were less than 10 years of age [Table/Fig-1].
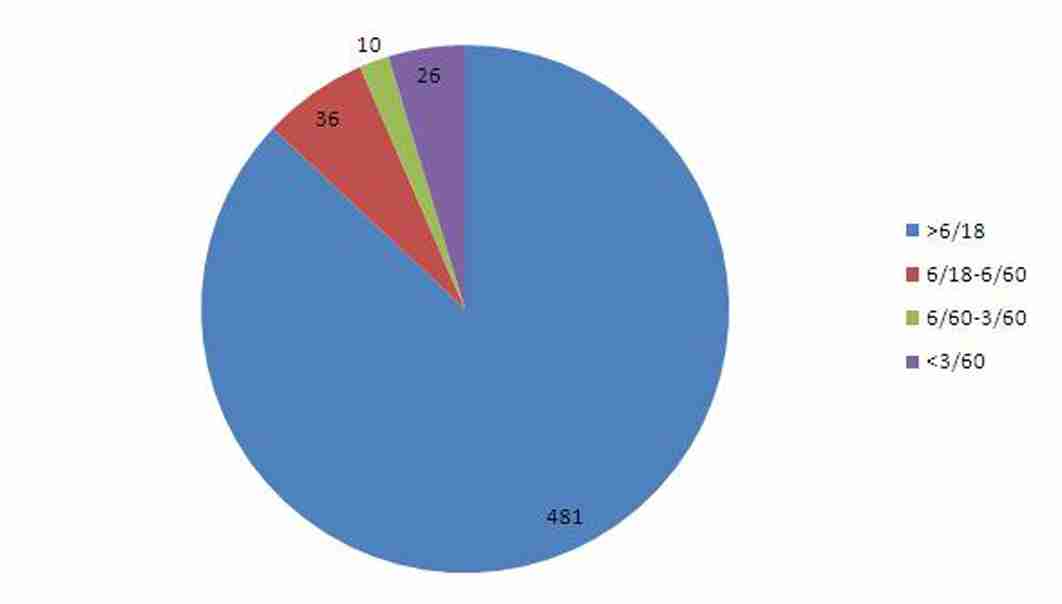
481(87%) patients had a BCVA of >6/18, whereas 26 patients (4.7%) had a vision of less than 3/60 [Table/Fig-2].
208 patients (37.6%) had various ocular manifestations which included both innocuous lesions to vision threatening findings. Anterior segment manifestation was seen in 39 patients (7%). The most common anterior segment manifestation was the occurrence of recurrent lid infections, which was seen in 8 patients. HZO occurred in 5 patients. The other findings included the presence of acute iridocyclitis in 3 patients and healed uveitis in 5 patients. Three patients presented with Molluscum contagiosum of the lids, while 6 patients had corneal opacities. Two children suffered from severe VKC, while 2 adults had conjunctival masses, which on excision biopsy, revealed the presence of OSSN. Dry eye with corneal SPK was seen in 2 patients. One patient had atrophic bulbi. Pseudo membranous conjunctivitis was seen in 2 females who were on ART, which was secondary to the occurrence of Steven Johnson Syndrome [Table/Fig-3].
Posterior segment manifestations were seen in 55 patients (9.94%). The most common posterior segment manifestation was HIV microangiopathy which was seen in 27 patients (5%). A majority of these patients presented with a single cotton wool spot in one eye. The most common opportunistic infection was CMV retinitis which was seen in 14 patients (2.53%), while 5 of these patients presented with retinal detachment as a sequelae to CMV retinitis. Active toxoplasmosis was seen in 2 patients, while 2 patients presented with healed choroiditis. Two patients with co existent anaemia had bilateral multiple superficial haemorrhages with Roth spots. Superotemporal BRVO was seen in 1 patient, while 7 patients had a non-specific, stippled fundus (salt and pepper like) [Table/Fig-4].
Best Corrected Visual Acuity
Anterior segment manifestations
| Manifestations | No of pts |
|---|
| Lid infections | 8 |
| Corneal opacity | 6 |
| Herpes zoster ophthalmicus | 5 |
| Healed anterior uveitis | 5 |
| Acute iridocyclitis | 3 |
| Molluscum contagiosum | 3 |
| Vernal kerato conjunctivitis | 2 |
| Superficial punctate keratitis | 2 |
| Ocular surface squamous neoplasia | 2 |
| Steven Johnson syndrome | 2 |
| Atrophic bulbi | 1 |
Posterior segment manifestations
| Manifestations | No of patients |
|---|
| HIV microangiopathy | 27 |
| CMV retinitis and its sequalae | 14 |
| Stippled fundus | 7 |
| Active toxoplasmosis | 2 |
| Healed choroiditis | 2 |
| Roth spots | 2 |
| Superotemporal BRVO | 1 |
Neuro-ophthalmic Manifestations
| Manifestations | No of patients |
|---|
| Hyperaemic disc | 7 |
| Pupillary abnormalities | 7 |
| Papilledema | 5 |
| Optic neuritis | 3 |
| Disc pallor | 3 |
| Lateral rectus palsy | 3 |
| Ptosis | 3 |
| Primary optic atrophy | 1 |
CD4 count in different opportunistic infections in AIDS
| No of CD4+ T Cells | Diseases at risk |
|---|
| <500 cells/micro litre | Kaposi’s sarcoma, Lymphoma, Tuberculosis |
| <250 cells/micro litre | Pneumocystosis, Toxoplasmosis |
| <100 cells/micro litre | Retinal microangiopathy, Conjunctival microvasculopathy, Keratoconjunctivitis sicca,VZV retinitis, CMV retinitis |
Among the neuro-ophthalmic manifestations, optic neuritis was seen in 3 patients, whereas bilateral papilledema was seen in 5 patients during the late stage of AIDS. Fundus examination also revealed the presence of hyperaemic discs in 7 patients who did not have any visual abnormalities. Three patients had disc pallor, while 1 patient had primary optic atrophy. Lateral rectus palsy with strabismus was present in 3 patients. Three patients presented with ptosis. Pupillary abnormalities without any ocular disease was seen in 7 patients [Table/Fig-5].
One of the unusual manifestations that we encountered in these patients was the presence of bilateral lid retraction, which was seen in 47 patients (8.5%). On testing for colour vision, 35 patients (6.3%) were found to have colour vision abnormalities without any posterior segment pathology.
Discussion
Since its discovery, HIV infection has become one of the world’s greatest public health problem in the recent years. AIDS is a multisystem disorder which is caused by the Human Immunodeficiency Virus (HIV) which belongs to the Lenti virus subfamily of retroviruses. HIV targets the CD4+ T cells, causing a steady decline in the absolute number of these cells, resulting in a progressive immune deficiency, particularly of the cell mediated type. A regular estimation of the CD4+ T cell count is therefore a useful measure of the disease progression.
The CD4+T cell counts are measured every 3 months and a count of less than 200/micro litre implies a high risk of HIV related disease. The ocular manifestations are among the most common clinical features of HIV infection/AIDS patients. These lesions are varied and they affect almost all the structures of the eye. These include:
A non infectious retinal microangiopathy which consists of cotton wool spots with or without intraretinal haemorrhages and microvascular changes like microaneurysms and telangiectasiae.
Opportunistic ocular infections, primarily CMV retinitis.
Unusual neoplasms like Kaposi’s sarcoma.
Neuro-ophthalmic lesions.
Immune Reconstitution Inflammatory Syndrome (IRIS) is a well recognized complication which occurs during the initial weeks of the treatment with ART and HAART.
These ocular manifestations occur throughout the illness, with an increasing HIV virulence and a progressive loss of the CD4+ T cell numbers [Table/Fig-6].
In our study, 37.6% of the patients had ocular findings which included both anterior and posterior segment findings, adnexal lesions and neuro-ophthalmic signs. Unusual findings like lid retraction and colour vision abnormalities were seen in these patients.
Ocular lesions occur in 40- 70% of the AIDS patients, according to various studies [3,5,7-9]. Due to the increased numbers of ART centres, frequent monitoring of the CD4 counts and early initiation of ART, the incidence of ocular findings has decreased considerably. On the other hand, due to an increase in the life span of these patients, it has been estimated that 70-80% of the adult AIDS patients will experience an ocular complication at some point of their illness.
We encountered anterior segment and adnexal manifestations in 7% of the patients. However, reports indicate that > 50% of the HIV infected patients have anterior segment and adnexal manifestations [10].
The most common anterior segment manifestation was recurrent lid infections. Severe blepharitis, styes and lid ulceration may be the initial involvement in AIDS [11]. We observed that the lid infections tend to be more severe, bilateral and recurrent in these patients. Lid hygiene had to be maintained and antibiotics had to be continued for a longer duration in these cases than in normals. Three patients had Molluscum contagiosum of the lids and among these, 1 case had extensive bilateral lesions. A study which was done by Bardenstein DS et al., indicated the occurrence of these lesions in up to 5% of HIV infected cases [12]. Five cases in our series had HZO. Among these, 2 patients presented with severe keratitis with iritis. The incidence of HZO in the HIV population is reported to be 5-15% [13]. In young individuals, it may be the initial manifestation of HIV. Any patient who is less than 50 years of age, with HZO, is a suspect of HIV or any immunosuppression condition [14]. The findings which were suggestive of healed uveitis in the form of posterior synechie, old KP’s and iris patches were seen in 5 patients, while 3 patients presented with active iridocyclitis. Studies have revealed that the incidence of anterior uveitis was less common than that of posterior uveitis and the causes included herpetic uveitis , drug induced and immune recovery uveitis. We encountered 2 patients who presented with rapidly growing conjunctival masses. An excision biopsy revealed the presence of conjunctival squamous cell carcinoma. Conjunctival squamous cell dysplasia and neoplasia have been associated with HIV infection and AIDS in the sub-Saharan African population. OSSN can be the initial manifestation of an asymptomatic HIV disease [15]. We did not encounter any case of Kaposi’s sarcoma in our study. A study which was done by Biswas et al, who followed 100 HIV +ve individuals in India, did not observe a single case of Kaposi’s sarcoma. This could be due to the lower prevalence of homosexual behaviour and the low incidence of the human Herpes virus 8, which are known to be associated with Kaposi’s sarcoma [5]. Pseudomembranous conjunctivitis and keratitis which were seen in 2 patients, were secondary to Steven Johnson’s syndrome. SJS is known to occur in the patients who are on treatment with Nevirapine, which is a part of HAART [16]. Though SJS occurs as a side effect of a variety of drugs, the presence of HIV infection dramatically increases the risk.
Posterior segment manifestation was seen in 9.94% of our patients. This was in contrast to other reports which suggested the incidence of posterior segment lesions in more than 50% of the AIDS patients [17].
HIV related microangiopathy was found to be the most common ocular lesion in AIDS before the introduction of HAART. Cotton wool spots occur in 25-50% of the patients with advanced HIV disease and they are the earliest and the most consistent finding in HIV retinopathy [18]. In our study, HIV micro angiopathy was seen in only 5% of the individuals. Most of the cases presented with a single cotton wool spot. Two patients who were in the late stages of the HIV infection, with co-existent anaemia, presented with Roth spots. Similar lesions have been described in other studies and this could be due to the haemorrhagic abnormalities in these patients. Our study could be compared to Pathai S et al., ‘s study, that had analyzed the prevalence of HIV associated ophthalmic disease in patients who had enrolled for ART and the incidence of HIV microangiopathy was found to be 4.7% [9]. The relative low incidence in our series could be due to the vast number of patients, which had included patients with high CD4+ counts, who were not yet on ART. One patient had superotemporal BRVO. BRAO and BRVO have been seen in patients with HIV [19, 20]. 2.53% of the patients presented with various stages of CMV retinitis. The disease was bilateral in 4 patients. Nine patients had active retinitis, while 5 patients had retinal detachment. CMV retinitis was the most common retinal infection in the patients with HIV, affecting 15 to 40% of the patients in the pre-HAART era [7]. This disease classically occurs when the CD4+ count is < 100 cells per micro litre. Doan et al., in his study ,described CMV retinitis in 1.2% of the cases and this decrease in prevalence was found to have occurred due to the advent of HAART [21].
Active toxoplasmosis was seen in 2 patients, while 2 cases had healed choroiditis. Studies have indicated that 1-2% of the HIV infected patients could present with toxoplasmic retinichoroiditis. Non specific, stippled fundi were seen in 7 patients. Surprisingly, these patients did not have any significant visual abnormalities.
Neuro-ophthalmic manifestations like diplopia, Papilledema, visual field defects, optic neuritis and optic atrophy are known to occur in 15% of the HIV patients [22]. In our series, 5.78% of the patients had neuro-ophthalmic manifestations like optic neuritis, papilledema, disc pallor, lateral rectus palsy, ptosis and non specific pupillary abnormalities, without having any underlying ocular pathology. Papillo-oedema was seen in patients with meningitis in the late phase of HIV infection. We also came across 7 patients who had hyperaemic discs without any symptoms or signs which were suggestive of optic neuritis or papilledema.
Surprisingly, in our study, we observed the presence of lid retraction in 8.5% of the patients. A similar condition was described by Wang G [23]. Weight loss and muscle wasting are frequent occurrences in HIV patients and they are independent markers of mortality. The causes could be multifactorial. However, poor nutrition and an altered metabolism have been implicated.Lid retraction in HIV patients could be secondary to orbicularis oculi weakness and wasting, leading to poor eyelid closure and ocular surface disorders.
All the patients in our study underwent colour vision assessment and 6.3% were found to have colour vision abnormalities without any significant retinal changes. A study which was done by Shah KH et al., revealed the presence of an abnormal contrast sensitivity and colour vision abnormalities in 7% and 9.9% of HIV patients, which were found to occur independently without the presence of any vision threatening retinal lesions or media opacities [24]. These could be attributed to the thinning of the RNFL, which was secondary to damage of the small calibre axons in HIV infected patients [25].
However, there were a few limitations in our study. The follow up findings were not included, as most of the patients were inconsistent or lost for follow up. Other factors like the duration of the HIV infection, any underlying systemic disease and the treatment schedule were not included. The correlation of the CD4+ counts with the ocular manifestations could not be assessed, as the time of the CD4+ count estimation did not coincide with the time of the ocular examination. Since the CD4+ count analysis was not done at the time of the ocular examination, the correlation between these two factors would be inappropriate.
Conclusion
Ocular manifestations are among the most common clinical features in HIV/AIDS patients having various clinical presentations affecting almost all the structures of the eye. Moreover, the ocular findings can be the initial manifestations of the underlying disease. However, diagnosis and management of the ocular diseases in these patients pose a therapeutic challenge to ophthalmologists, due to the atypical disease presentations and the lack of specific investigations which provide a rapid and a reliable confirmation of the clinical diagnosis. Hence, an awareness on ocular lesions in AIDS is important for their early recognition and management or for the early referral of patients to AIDS care centres. The current practice at several ART centres in India is to refer the patients for an ophthalmic examination only on complaint of ocular symptoms. However, it is important to note that many of the ocular manifestations may be asymptomatic. Hence, screening for ocular complaints is not a reliable method for identifying those with ocular morbidities. This highlights the need for a routine ophthalmic screening with a complete ocular examination in all HIV/AIDs patients.
[1]. WHO/UNAIDS/UNICEF (2011)“Global HIV/AIDS response: Epidemic update and health sector progress towards universal access” 2011 [Google Scholar]
[2]. NACO 2011 Annual report 2010-2011 [Google Scholar]
[3]. Holland GN, Pepose JS, Pettit TH, Gottlieb MS, Yee RD, Foos RY, Acquired immune deficiency syndrome: Ocular manifestationsOphthalmology 1993 90:859-73. [Google Scholar]
[4]. Holland GN, Gottlieb MS, Yee RD, Ocular disorders associated with a new severe acquired cellular immunodeficiency syndromeAm J Ophthalmol 1982 93:393-02. [Google Scholar]
[5]. Biswas J, Madhavan HN, George AE, Kumarasamy N, Solomon S, Ocular lesions associated with HIV infection in India: A series of 100 consecutive patients evaluated at a referral centreAm J Ophthalmol 2000 129:9-15. [Google Scholar]
[6]. Biswas J, Madhavan HN, Badrinath SS, Ouclar lesions in AIDS: A report of first two cases in IndiaIndian J Ophthalmol 1995 43:69-72. [Google Scholar]
[7]. Sahu DK, Namperumalsamy P, Walimbe P, Rajalakshmi C, Ocular manifestations of HIV infection /AIDS in south Indian patientsInd J Ophthalmol 1999 47:79 [Google Scholar]
[8]. Shah SU, Kerkar SP, Pazare AR, Evaluation of ocular manifestations and blindness in HIV/AIDS patients on HAART in a tertiary care hospital in western IndiaBr J Ophthalmol 2009 93:8-90. [Google Scholar]
[9]. Pathai S, Deshpande A, Gilbert C, Lawn SD, Prevalence of HIV associated ophthalmic disease among patients enrolling for anti retroviral treatment in IndiaBMC Infectious Diseases 2009 9:158 [Google Scholar]
[10]. Akduman L, Pepose JS, Anterior segment manifestations of acquired immune deficiency syndromeSemin Ophthalmol 1995 10:111 [Google Scholar]
[11]. Biswas J, Madhavan HN, Kumarasamy N, Solomon S, Blepharitis and lid ulcer as initial ocular manifestation in acquired immunodeficiency syndrome patientsInd J Ophthalmol 1997 45:233 [Google Scholar]
[12]. Bardenstein DS, Elmets C, Hyper focal therapy of multiple Molluscum Contagiosum lesions in patients with acquired immunodeficiency syndromeOphthalmology 1995 :102-1031. [Google Scholar]
[13]. Jabs Da, Quinn TC, Pepose JS, Holland GN, Wilhemus KR, Acquired immunodeficiency syndromeOcular infection and immunity. St Louis: Mosby-Year Book 1996 :289-310. [Google Scholar]
[14]. Biswas J, Samanta TK, Madhavan HN, Kumarasamy N, Solomon S, Acute panuveitis with haemorrhagic hypopyon as a presenting feature of acquired immunodeficiency syndromeInd J Ophthalmol 2000 48:311 [Google Scholar]
[15]. Fogla R, Biswas J, Kumar SK, Madhavan HN, Kumarasamy N, Solomon S, Squamous cell carcinoma as initial presenting sign in a patient with acquired immunodeficiency syndrome due to HIV type 2Eye 2000 14:246 [Google Scholar]
[16]. Singh Harminder, Nevirapine induced SJS in an HIV infected patientDrug Watch 2011 43(1):84-86. [Google Scholar]
[17]. Caskey PJ, Ai E, Posterior segment manifestations of AIDSOphthalmol Clin North Am 1990 3:396 [Google Scholar]
[18]. Freeman WR, Lerner CW, Mines JA, Lash RS, Nadel AJ, Starr MB, A prospective study of the ophthalmologic findings in the acquired immunodeficiency syndromeAm J Ophthalmol 1984 97:133 [Google Scholar]
[19]. Teich SA, Sonnabend J, Central retinal vein occlusion in a patient with AIDSArch Ophthalmol 1988 106:1508-09. [Google Scholar]
[20]. Yassur Y, Biedner B, Fabrikant M, Branch retinal artery occlusion in acquired immunodeficiency syndrome prodromeAnn Ophthalmol 1988 20:191-92. [Google Scholar]
[21]. Doan S, Cochereau I, Guvenisik N, Cytomegalovirus retinitis in HIV infected patients with and without highly active antiretroviral therapyAm J Ophthalmol 1999 128:250-51. [Google Scholar]
[22]. Miller NR, Walsh and Hoyt's clinical neuro-ophthalmology 1995 Vol. 54th ed.(Part 2)BaltimoreWilliams & Wilkins:4107-56. [Google Scholar]
[23]. Wang G, McCulley TJ, Eyelid retraction and incomplete eyelid closure secondary to human immunodeficiency virus-associated muscle wastingOphthal Plast Reconstr Surg 2006 22(6):479-80.Nov-Dec [Google Scholar]
[24]. Shah KH, Holland GN, Fei Yu, Natta MV, Nusinowitz S, Contrast sensitivity and color vision in HIV infected individuals without Infectious retinopathyAm J Ophthalmol 2006 142(2):284-92.Aug [Google Scholar]
[25]. Partho S, Holland GN, Fawzi AA, Arantes TE, Fei Yu, Sadun AA, Association between Retinal nerve fibre layer thickness and abnormalities of vision in people with HIV infectionAm J Ophthal 2012 153(4):734-42.Apr [Google Scholar]