Post operative pain relief is an essential criterion for the patients who undergo major orthopaedic surgeries [1]. Procedures like Total Knee Replacement (TKR) are still in debate with respect to their post-operative pain management [2,3]. Since central neuraxial anaesthesia cannot provide adequate post-operative analgesia when it is used alone, an alternative analgesic method is usually advised. The systemic analgesics which may include paracetamol, NSAIDs or an opioid alone or in combinations, are necessary many a times. However, these parenteral analgesic supplements are not without side effects and a ‘breakthrough’ pain relief is not always possible. Alternatively, a properly performed Peripheral Nerve Block (PNB) may reduce the requirement of the alternative analgesic methods and thus, it may cause less drug induced morbidity, psychological stress, insomnia and anxiety.
The knee joint is supplied through L2-4 in terms of the femoral nerve (mainly the anterior one) and the sciatic nerve (L4, 5 and S1-3, posteriorly). The blockade of the anterior and the posterior segments through injections of a local anaesthetic solution into the femoral or the sciatic nerves should ideally, completely reduce the pain transmission and improve the analgesia [4]. The combination of the sciatic and the femoral nerve blocks collectively is practised at many centres,[5,6] however, performing the blocks together are limited by certain factors like the position of the patient, toxicity of the local anaesthetics, etc, when an active epidural is in situ. Also, this approach may be too cumbersome in the patients with regional or general anaesthesia and in this direction, the clinical trials are yet to decide their feasibility. Our study was aimed at evaluating the efficacy (in terms of the pain scores, the additional analgesic requirements, sleep, etc) and safety (complications and haemodynamic instability) of a single injection femoral nerve block in the patients with TKR, who had concomitant epidural analgesia. Also, our evaluation was extended for two consecutive days of the surgery. This evaluation is necessary with respect to the (early) ambulation of the patient, duration of the stay in the Post Anaesthesia Care Unit (PACU), the patient’s compliance in the acceptance of the analgesic method, the haemodynamic monitoring and the subsequent opioid and the other analgesic requirements.
Materials and Methods
This study was approved by the institute ethical committee. Twenty four consecutive patients with ASA (American Society of Anaesthesiology) grades 1 and 2, who were anaesthetized by a single anaesthesiologist and were operated upon by a single surgeon, who had been undergoing TKR surgeries over a 5 month period (January 2012 to July 2012), were considered for our retrospective, non-comparative study. ASA 2 included the patients with systemic hypertension and diabetes mellitus which had been well controlled on treatment. The patients with cardiovascular, respiratory, neurological, renal, endocrine, eye or autonomic dysfunctions were excluded. After the pre-operative assessment and the recording of the baseline vitals, the patients, having fasted for 8 hours prior to the surgical procedure, were pre-medicated with tab. ranitidine 150mg. No sedatives or opioids were used as the pre-medicants.
In the operating room, all the patients were inserted with an epidural catheter (18G) at the lumbar L3-4 or L2-3 vertebral level and with the catheter, 3cm inside the epidural space. Following this, a subarachnoid block was performed with a 23G or a 25G spinal needle and with 3ml of 0.5% heavy bupivacaine, below the level of the epidural catheter insertion. After checking the level of the block, the surgery was allowed to continue and it was completed. The vitals of the patients were maintained throughout the procedure.
An epidural test dose with lignocaine and adrenaline (1:200000), 3ml was used to confirm the placement of the catheter. At the end of the surgery, a bolus dose of 20ml of 0.125% of bupivacaine with inj.fentanyl (1 to 2mcg/ml) was administered for the purpose of the postoperative analgesia. Following the same, a single injection femoral nerve block was performed with the patients in the supine position. A 21G, 50mm, 30° nerve locator needle (leucoplex, VYGON, E.C., France) was used for the femoral block; the posterior branch of the femoral nerve was located (by palpation and by the contraction of the quadriceps muscle at a current of 0.5mA). A volume of 30ml local anaesthetic (0.25% bupivacaine + 1500 units of hyaluronidase) was injected into the femoral sheath with a firm and a distal, digital pressure applied.
Postoperatively, the epidural infusion was continued with a solution of the local anaesthetic bupivacaine 0.125% with fentanyl 2mcg/ml , at the infusion rate of 6 ml/hour for two consecutive days. The vitals were monitored throughout the study. Any haemodynamic instability was noted and it was treated accordingly (inj. Atropine, inj. Ephedrine, saline boluses). All the patients were advised to inform the event of acute worsening pain or the pain event when the visual analogue score of the pain assessment was 3 or higher. The time duration after the femoral block till the first appearance of a pain VAS score of 3 was noted. A bolus dose of 10ml of epidural was administered and if the pain did not subside or decrease in intensity, an additional method of analgesia was advised. The additional analgesics included inj. Paracetamol 1gm, I.V. or inj.diclofenac 75 mg I.M., or inj. Tramadol 100mg I.V and this was administered only when it was demanded by the patients on both the days. The total number of patients who required such bolus doses of epidural and additional analgesic drugs was noted.
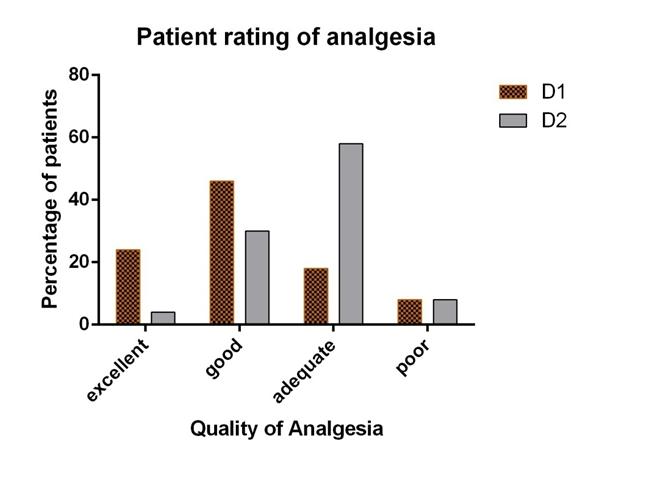
On the evening of day 1 and on the second day of the surgery (D1 and D2, approximately at 8 and 32 hours of the femoral block, respectively), the patients were assessed for their VAS pain scores (D1 and D2, categorical and mean), sleep (D1) and their requirement of the total bolus doses and additional analgesics (D1 and D2). The categorical score pain assessment included mild (VAS 1 to 3), moderate (VAS 4 to 6) and severe (VAS >7) ratings by classification. The individual patient rating for the overall analgesia for both the days (D1 and D2) too was noted (excellent, good, adequate and poor). The total amount of epidural bupivacaine, the epidural volume and the epidural fentanyl for each day too were noted. Any complications which were related to the femoral nerve block were watched for. The epidural related haemodynamic events were monitored carefully and treated, if any.
The data were presented as mean and Standard Deviations (SD). The Student’s t test and the Chi-square test were used wherever they were appropriate. GraphPad Prism, version 6.01 was used to analyze the data and for the preparation of the graphs. A ‘P’ value which was below the level of .05 was taken as statistically significant.
Results
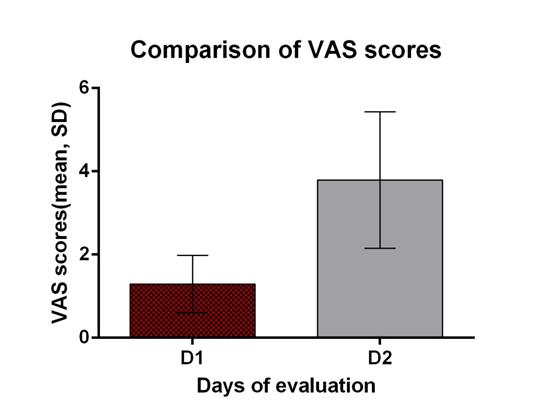
The different data which were obtained have been shown in [Table/Fig -1]. The mean time which was required to develop a VAS score of at least of 3 was 8.55±1.78 hours. The VAS assessment mean scores of day 1 were compared to those of day 2 and the ratio which was obtained was 0.4±0.32. The mean VAS scores were higher on D2 as compared to those on D1 and they were statistically significant (P<.0001, Student’s t test, [Table/Fig-2], [Table/Fig-3].
| 1. Age (years, mean±sd) | 64.3±8.4 |
| 2. Sex[m][f] | 2, 22 |
| 3. VAS: |
| a. Mean time to achieve VAS score of 3 (n=16, hours) | 8.6±1.8 |
| b. VAS /day2 ratio(mean±sd) | 0.4±0.3 |
| 4. Epidural analgesia details |
| a. Total volume of epidural injected (mean±sd) on D1 | 110.7±7.7 |
| Total volume of epidural injected (mean±sd) on D2 | 156.7±7.8 |
| b. Total mg of Bupivacaine injected (mean±sd) on D1 | 88.6±6.5 |
| Total mg of Bupivacaine injected (mean±sd) on D2 | 125.3±6.3 |
| c. Epidural fentanyl infused (mean±sd) on D1 | 177.2±12.7 |
| Epidural fentanyl infused (mean±sd) on D2 | 250.7±12.3 |
| d. Bolus in first 8 hours demanded (number of patients, total number) | 4, 4 |
VAS scores comparisons *P< 0.05,$P<0.001.
| Pain assesment | D1 | D2 |
|---|
| a.VAS scores* | 1.3±0.69 | 3.79±1.64 |
| b. Epidural bolus requrements |
| Number of patients | 4 | 13 |
| Number of boluses | 6 | 16 |
| c. Additional analgesics requirements |
| Number of patients | 5 | 16 |
| Number of boluses | 7 | 24 |
| d. Distribution of pain scores $ (number of patients) |
| Mild | 23 | 14 |
| Moderate | 1 | 9 |
| Severe | 0 | 1 |
Comparison of VAS on two different days of surgery
Patient rating of analgesia on day 1 and day 2
Other events *= not evaluated
| Event | D1 | D2 |
|---|
| Hemodynamic disturbance | 2 | NIL |
| Sleep disturbance | 8 | NE* |
| Vomiting | 9 | 2 |
The categorical score comparison too revealed higher scores on D2 (P<.001, Chi-square test, [Table/Fig-2]. A total of 13 patients (52%, 16 boluses) required bolus doses of epidural analgesia with bupivacaine on D2 as compared to D1 (4 out of 24, 16%, 6 boluses). Additional analgesia on demand was noted in 5 patients (7 doses, total, 21%) on D1 in contrast to 16 patients (24 doses, 67%) on D2 [Table/Fig-2].
The complaint of sleep disturbance was seen 8 patients on D1. The analgesia was rated as excellent by 7 of 24 (29%) patients, as good by 11 of 24 (46%) patients, as adequate by 4 of 24 (17%) patients and as poor by 2 of 24 (8%) patients on D1. Similarly, the ratings as excellent by 1 patient (4%), as good by 7 (29%) patients, as adequate by 14 (58%) patients, and as poor by 2 (8%) patients were recorded on D2, respectively (P<0.001, Chi-square test, [Table/Fig-4].
A haemodynamic instability was observed in 2 patients, which necessitated treatment but it was not life threatening on D1. None of the patients had events which were related to the haemodynamics on D2. Vomiting was noted in nine patients on D1 and in 2 on D2 [Table/Fig-5].
Discussion
Several analgesic regimens express post operative pain relief concerns for the patients ho undergo TKR surgeries [7]. The epidural analgesia is shared with other parenteral methods which are customarily used. However, they allege inadequate pain relief or satisfaction among the patients. The co-administration of nerve blocks gained its importance, owing to its precise action, especially when ultrasonographic guided blocks are performed [8].
The observed mean time which was required to achieve pain scores to a minimum of 3 approximately, was 9 hours after the performance of the block. This observation however was recorded in 67% of the patients who achieved the required pain score. Also, it suggests that the other remaining patients had an even longer duration of the analgesia on D1 and that they had pain scores which were less than the desired score for making a complaint. The smaller SD suggests the uniform duration of action of the femoral block and this may be attributed to the use of an equivalent dose concentration and volume of the local anaesthetics in all of our study patients. The possibilities of physician induced inaccuracies which resulted in varied durations of action were low, as the block was performed in all the patients by a single anaesthesiologist. The regression of the epidural also contributed to the appearance of the pain; however, in such situations, the chief site of the pain will be the posterior aspect of the knee. This is possibly because of the sparing of the thick sacral fibres which supply the above mentioned region, which requires a higher concentration and volume of the epidural infusion. The observed incidence of pain at the posterior knee approximately in 50% of the total study group individuals, as the primary pain site for their first complaint, described the efficiency of the femoral nerve analgesia than that of the epidural method.
A ‘two days’ pain evaluation showed a statistically significant difference in the mean pain scores which were achieved, which indicated the analgesic superiority on D1. The VAS ratio which was lesser than one undoubtedly indicated the unequal distribution of the pain scores for different days of the evaluation. The lower number of bolus requirements and the additional analgesic requirements on D1 as compared to those on D2 explained the role of the femoral nerve block analgesia method with respect to its duration and effectiveness. In addition, the significantly higher quality of the patient’s rating of analgesia as ‘good’ or excellent’, confirmed the superiority of the analgesic method on D1. The ‘bolus’ requirement of the epidural was observed (for 2 days) in more than 50% of the individuals. When we analyzed further into the patient’s needs in the first 8 hour duration of the block, a very low number of patients substantiated the femoral nerve block action as an analgesic method during this period.
The observed higher VAS on the successive day, which necessitated additional analgesics in many patients, may be best co-related to the disappearance of the femoral block action. The femoral nerve block can last long for 12 hours or sometimes even longer, when larger volumes and higher concentrations of the local anaesthetics are used. Had we used a higher concentration of the drug (0.5% bupivacaine), the analgesic duration might have lasted longer; however, it comes with the superfluous price of having a motor blockade of the quadriceps muscle and higher discomfort to the patient.
Performing a combined sciatico-femoral nerve block in a patient with an epidural is not without a trouble-free environment with respect to both the methodological aspects and the convenience. The changes in the position of the patient, the total drug dosage and the elicitation of specific motor responses for the nerve stimulation, are the specific concerns in a patient who has already undergone the surgery. An accurately performed sciatic nerve block through a peripheral nerve stimulator necessitates 30 to 40 ml of the local anaesthetic solution, which adds to the total milligram of the drug which is injected into the body [9]. When a combined femoral nerve block is planned in such a patient, the total dose of the local anaesthetic which is used, has to be appended and thus, it may surpass the toxic dose for a particular local anaesthetic. In many circumstances, when a dilute concentration of the drug is used, either an ineffective block or insufficient duration results are observed. An already activated epidural may further complicate the issue. Since the toxicity of the local anaesthetics [10] can be a life threatening potential event, it may be truly required to titrate the risk benefit ratio of the combined nerve blocks versus aiming for one hundred percent analgesia in the patients who undergo TKR.
The patients with an epidural infusion following the surgery, do not require a second repositioning for performing the femoral block, as the same can be executed with the patients in the supine position. Nerve stimulation and location through a peripheral nerve stimulator will not distress the patients, owing to the earlier anaesthesia and all our patients abided by the block very well without any pain or discomfort at the operated site. Anaesthesiologists will be unable to elicit the specific ‘patellar dance’ response while they perform a femoral nerve block in the patients who had already undergone knee surgeries, owing to the heavy dressings around the operated site. In such situations, one needs to apply the methodology of ‘the palpation of quadriceps contraction’, which validates the correct placement of the nerve stimulator needle. A properly placed needle and an adequate volume of the anaesthetic will warrant a long lasting, adequate analgesia, as we observed in our patients.
The petite number of individuals who manifested the haemodynamic changes was attributed to the blood loss which followed the surgery. The surgical drains from the operated site had a collection of more than 800ml of blood. The haemodynamic changes should be predicted in the patients with blood loss but with no pain at the operative site, especially in those with an ongoing epidural infusion! However, a timely treatment with fluids and vasopressors resulted in no harm. Arterial puncture and haematoma formation, nerve damage, echymosis, tingling and numbness at the site of the injection can also be associated; but we did not observe any such sequel.
Though a multimodal analgesia confirms adequate pain relief in any post-operative patient, it should be titrated with the patient’s risk and benefits. We executed a single injection femoral nerve block alone and we did not combine it with a sciatic block in our patients, to keep it as a simple and an effective mode of analgesia [11,12]. The ongoing epidural infusion will restrict the patients from shifting from the PACU and their mobilization. Thus, on D2, an epidural analgesia is not always possible. A CFNB may be beneficial [13] but it adds to the cost of the anaesthesia and it causes risk for the patient with respect to haematoma and nerve damage, particularly when post operative anticoagulants are used, thus necessitating a post operative close monitoring of the limb function [14]. However, in the patients with a single injection femoral block, the risk of the same is too far and it is definitely less hazardous. A meta-analysis which was done by Paul and colleagues [15]. reported the superiority of the single injection FNB over other methods and the uncertainty of a CFNB and/or a sciatic nerve block. Our study confirmed the femoral nerve block for its ease of performance, effectiveness and safety in the patients with an ongoing epidural analgesia.
Conclusion
Single injection femoral nerve blocks provide adequate analgesia for the patients who have undergone TKR surgeries. It keeps the analgesic mode simple, comfortable and with least complications in the patients with an ongoing epidural local anaesthetic infusion.