Eosinophilic Gastroenteritis: A Diagnosis Behind the Curtains
Neha Agrawal1, Usha K. Rani2, Rohini Sridhar3, S. Dhamayanthi4
1 Registrar, Apollo Speciality Hospitals, Madurai, India.
2 Chief of lab services, Apollo Speciality Hospitals, Madurai, India.
3 Chief Operating Officer/Director of Medical Services, Apollo Speciality Hospitals, Madurai, India.
4 Registrar, Apollo Speciality Hospitals, Madurai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Neha Agrawal, Lab Services, Apollo Speciality Hospitals, Lake View Road, K.K. Nagar, Madurai-625020, India.
Phone: 09489034691
E-mail: neha_doc2005@yahoo.co.in
Eosinophilic gastroenteritis (EG) typically presents with a combination of chronic nonspecific gastrointestinal symptoms which include abdominal pain, nausea, vomiting, diarrhoea, weight loss, and abdominal distension. Approximately 80% of the patients have symptoms for several years. A high degree of clinical suspicion is often required to establish the diagnosis, as this disease is extremely rare.
We are presenting the case of a 19 year old boy who presented with growth retardation and markedly decreased secondary sexual characteristics. Taking the full clinical history and a meticulous investigation finally led to the diagnosis.
Eosinophilic gastroenteritis, Growth retardation, Eosinophils
INTRODUCTION
Eosinophilic Gastroenteritis is a rare gastrointestinal disorder that can present with various gastrointestinal manifestations, depending on the specific site of the affected gastrointestinal tract and the specific layer of the affected gastrointestinal wall. We are presenting a case of a 19-year old male who presented to the Endocrinology Department with the complaints of short stature and decreased secondary sexual characteristics. Taking a detailed clinical history and a meticulous investigation led to the diagnosis of eosinophilic gastroenteritis.
The diagnosis depends on the presence of gastrointestinal symptoms, the histological demonstration of the eosinophilic infiltration in one or more areas of the gastrointestinal tract or the presence of a high eosinophil count in the ascitic fluid (the latter usually indicates a subserosal variety) and no evidence of any parasitic or extraintestinal diseases.
It may mimic a peptic ulcer, an intestinal obstruction, gastroenteritis, irritable bowel syndrome, and inflammatory bowel disease. The long-term personal history of the gastrointestinal symptoms and the course of the disease with relapses and remissions, is the key for the disease to be suspected. Endoscopies, CT scans and sonographic studies may provide the important indirect signs of the disease, but only in combination with a histological examination can the diagnosis can be achieved.
CASE REPORT
A 19-year old male presented to the Endocrinology Clinic with the complaints of short stature and decreased secondary sexual characteristics. A detailed clinical history which was taken, revealed that the patient had recurrent episodes of abdominal pain and abdominal distention since he was 3 years of age. The preliminary investigations showed microcytic hypochromic anaemia with low serum protein levels ( serum protein -2.5g/ dl and serum albumin 1.3g/dl) with normal renal function tests and urine protein excretion. An upper gastrointestinal endoscopy which was done, showed an atrophic gastric mucosa with an otherwise normal picture.
The endoscopic biopsies showed chronic gastritis with Giemsa staining which was negative for H. pylori.
Colonoscopy showed that the entire colonic and the ileal mucosa appeared pale with normal vascularity .Multiple biopsies were taken from the terminal ileum, the caecum , the transverse colon and the rectum.
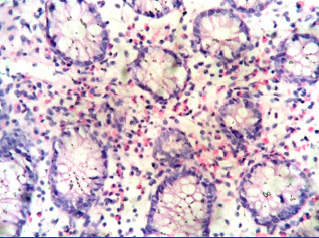
The histopathological examination showed an intense infiltration of the lamina propria of the colonic mucosa by eosinophils (> 25 per high power field ) [Table/Fig-1]. There was no evidence of any parasite or malignancy. Based on these findings, a diagnosis of eosinophilic gastroenteritis was made. The patient was started with a course of oral steroids, to which he responded.
H&E 400X colonoscopic biopsy showing intense infiltration by eosinophils
DISCUSSION
The primary eosinophilic gastrointestinal disorders are defined as the disorders that selectively affect the gastrointestinal tract with eosinophil rich inflammation in the absence of the known causes of eosinophilia like drug reactions, parasitic infections and malignancy. According to the reported literature, the primary sites are the stomach ( in 26- 81% of the cases) and the small intestine ( in 28-100% of the cases) . However, the oesophagus, the large intestine and the rectum may also be affected [1–3]. Eosinophilic gastroenteritis is a rare disease and it was first described in 1937 [4].
1970 saw the classification of eosinphilic gastroenteritis coming up, which was according to predominance of the eosinophilic infiltrate in different layers of the intestinal wall – the mucosa , the muscle layers and the subserosal layers [5]. The clinical presentation varies with the layer which is involved. The mucosal involvement presents with vomiting, dyspepsia , abdominal pain , diarrhoea, blood loss in the stool, iron deficiency anaemia, malabsorption and protein losing enteropathy. Children and adoloscents can present with growth retardation, a failure to thrive and growth retardation, which were the clinical presentations in our case. The patients with the muscle layer involvement typically present with a pyloric or an intestinal obstruction. The serosal involvement usually presents with eosinophilic ascites.
The currently accepted criteria are the presence of gastrointestinal symptoms, a predominant eosinophilic infiltrate on the histopathological examination and the exclusion of other causes of eosinophilia [6].
An endoscopic appearance in eosinophilic gastroenteritis is nonspecific. Because of the mucosal sparing, it is recommended to obtain at least six biopsy specimens from both the normal and the abnormal areas of the bowel [7]. The histopathology will reveal the eosinophilic infiltration of the lamina propria. The diagnostic criteria vary from >20 to >50 eosinophils per high power field [1,8].
There is an evident association between food allergy and EG and the results of the elimination diets are often poor [7]. When the improvement of the symptoms with the diet restriction is poor or not feasible, the next step in the treatment is the use of steroids.
Our patient presented with growth retardation, a short stature and markedly decreased secondary sexual characteristics. The proper clinical history which was taken, unveiled the gastrointestinal symptoms. The patient had recurrent episodes of abdominal pain and distention since the age of 3 years. The clinical constellation of the age group of the patient, the growth retardation, the recurrent gastrointestinal symptoms and the protein losing enteropathy warranted a differential diagnosis of primary intestinal lymphangiectasia [9]. The histopathological examination reflected the correct nature of the lesion, as the intestinal lymphangiectasia was characterized by the dilated intestinal lymph vessels.
One interesting finding in our patient was the absence of peripheral eosinophilia. However, Talley et al1 reported 40 patients with the diagnosis of eosinophilic gastroenteritis and compared them with 10 control subjects. The data showed that the peripheral eosinophil count was normal in 23% of the cases.
We presented this case to emphasize that the clinical symptoms often provide a deceptive picture of the underlying aetiology. There can be occasion when an endocrine presentation is not accompanied by a complementary aetiology. To summarize, eosinophilic gastroenteritis has a broad spectrum of clinical presentations. As such, a high index of suspicion is required to arrive at a correct diagnosis.
[1]. Talley NJ, Shorter RG, Phillips SF, Zinsmeister AR, Eosinophilic gastroenteritis: A clinicopathological study of patients with disease of mucosa, muscle and subserosal tissuesGut. 1990 31:54-58. [Google Scholar]
[2]. Lee CM, Changchien CS, Chen PC, Lin DY, Sheen IS, Wang CS, Eosinophilic gastroenteritis: 10 years experienceAm J Gastroenterol 1993 88:70-74. [Google Scholar]
[3]. Orenstein SR, Shalaby TM, Di Lorenzo C, Putnam PE, Sigurdsson L, Mousa H, The spectrum of paediatric eosinophilic esophagitis beyond infancy. A clinical series of 30 childrenAm J of Gastroenterol 2000 95:1422-30. [Google Scholar]
[4]. Kaijser R, Zur Kenntnis der allergischen Affektionen des Verdauungskanals vom Standpunkt des Chirurgen ausArchKlin Chir. 1937 188:36-64. [Google Scholar]
[5]. Klein NC, Hargrove RL, Sleisenger MH, Jeffries GH, Eosinophilic gastroenteritisMedicine. (Baltimore) 1970 49:299-319. [Google Scholar]
[6]. Khan S, Eosinophilic gastroenteritisBest Pract Res Clin Gastroenterol 2005 19:177-98. [Google Scholar]
[7]. Verheijden NAF, Ennecker Jans SAM, A rare cause of abdominal pain: eosinophilic gastroenteritisNJM 2010 68(11):367-69. [Google Scholar]
[8]. Baig MA, Qadir A, Rasheed J, A review of eosinophilic gastroenteritisJ Natl Med Assoc. 2006 98(10):1616-19. [Google Scholar]
[9]. Vignes S, Bellanger J, Primary intestinal Lymphangiectasia (Waldmann disease)Orphanet J Rare disease 2008 3:5 [Google Scholar]