The Budd-Chiari Syndrome in a Child: A Case Report and Review of the Literature
Vatsala Misra1, Kachnar Verma2, Dharmendra Kumar Singh3, Sri Prakash Misra4
1 Professor Departments of Pathology, Moti Lal Nehru Medical College, Allahabad, Uttar Pradesh, India.
2 Assistant Professor, Departments of Pathology, Moti Lal Nehru Medical College, Allahabad, Uttar Pradesh, India.
3 Professor, Department Pediatrics, Moti Lal Nehru Medical College, Allahabad, Uttar Pradesh, India.
4 Professor, Department Gastroenterology, Moti Lal Nehru Medical College, Allahabad, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kachnar Varma, Assistant Professor,Department Of Pathology, 4/412, MLN Medical College Campus, Allahabad-211002, Uttar Pradesh, India.
Phone: +91 9453029924; Fax +91 532 2256321
E-mail: varmakachnar@yahoo.co.in
The Budd-Chiari Syndrome is associated with hepatic venous outflow obstruction. This syndrome is rare in infants and children. As this syndrome is uncommon, especially in the paediatric age group, misdiagnoses and delays in the diagnosis are frequent. A high index of clinical suspicion along with a radiological aid and a histopathological correlation can lead to an early diagnosis and an appropriate management in such cases.
This case report highlights the occurrence of this rare condition in the paediatric age group as well as it redefines the salient features of this syndrome.
Hepatic venous obstruction, Venography, Centrizonal congestion, Fibrosis
INTRODUCTION
The Budd-Chiari Syndrome (BCS) is the clinical spectrum which is associated with hepatic vein thrombosis and it is characterized clinically by a triad of ascites, hepatomegaly and right upper quadrant pain. It is diagnosed by radiological imaging and liver biopsies [1]. This condition is uncommon in children as compared to adults. More than half of the cases of classic BCS occur between the ages of 20 and 39 years [2].
Owing to the rarity of this lesion in the paediatric age group, a high index of clinical suspicion is required and the final diagnosis can be made by doing a liver biopsy. Hence, we are reporting this rare case of a 2 year old child with an insidious onset, in whom a liver biopsy along with radiology, confirmed the diagnosis and helped in proper management.
CASE REPORT
A 2 year old girl presented with complaints of progressive abdominal distension and pain. On examination, pallor was found to be present, along with tense ascites. No lymphadenopathy was present. The routine investigations revealed a haemoglobin level of 8.5 g/dl; a total leucocyte count of 18,600 cells/mm3 and a differential leucocyte count of- 88%- neutrophils, 11%- lymphocytes and 1%- monocytes. The platelet count was 2.6 × 105 /mm3.
The liver function tests showed normal serum bilirubin and alkaline phosphatase levels, whereas the alanine and the aspartate aminotransferases (AST/ALT-268/342 IU) were mildly elevated. The total serum proteins were 5.2g/dl, with albumin levels of 3g/dl. The serum electrolytes and the renal function tests were within normal limits. The serum uric acid level was 3 mg/dl.
The ascitic fluid examination showed 5200 cells/mm3 with 93% polymorphonuclear neutrophils and 7% lymphocytes. The biochemical examination showed the protein level to be 3.6 g/dl and the sugar level to be 26 mg/dl respectively.
Ultrasonogram of the abdomen revealed hepatomegaly, ascites with dilated hepatic veins and many collaterals. Colour Doppler studies showed obstruction of the hepatic veins with loss of the normal triphasic flow pattern with flow reversal. The inferior Vena Cava (IVC) showed narrowing near the opening of the hepatic veins. A radiological diagnosis of BCS was given. A liver biopsy was done to confirm the diagnosis.
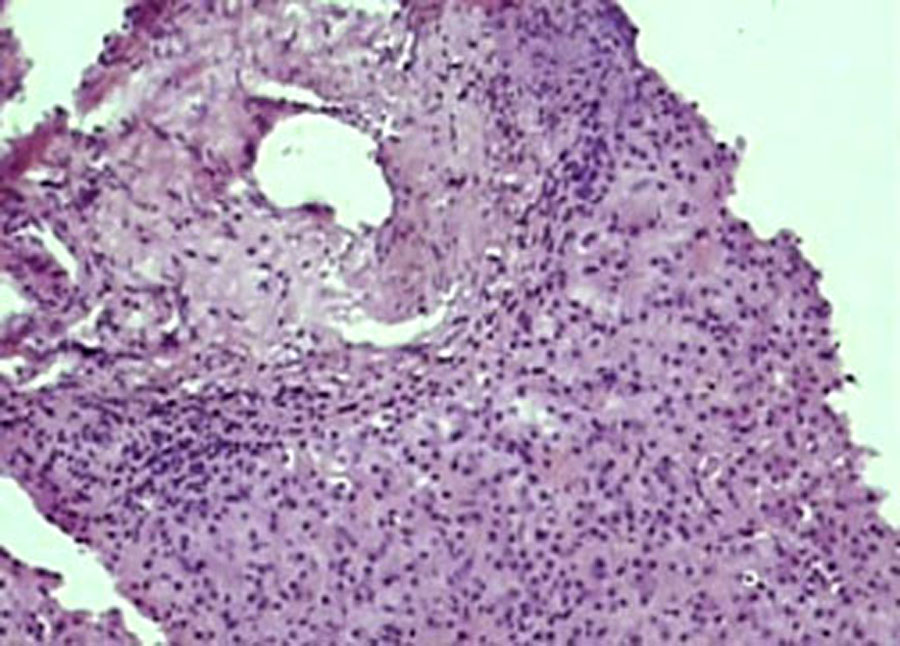
The biopsy material showed a normal liver architecture with focal areas of centrilobular congestion and sinusoidal dilatation. The terminal hepatic veins were dilated and they showed perivenular fibrosis. The histochemical stains (Reticulin and Van Gieson’s) further highlighted the perivenular fibrosis. The perivenular areas showed hepatocyte degeneration and necrosis. The portal tracts were otherwise preserved with a mild fibrous expansion [Table/Fig-1],[Table/Fig-2].
Photomicrograph showing histopathologic features of BCS with centrizonal congestion, perivenular fibrosis.(Hand E stain X 200)
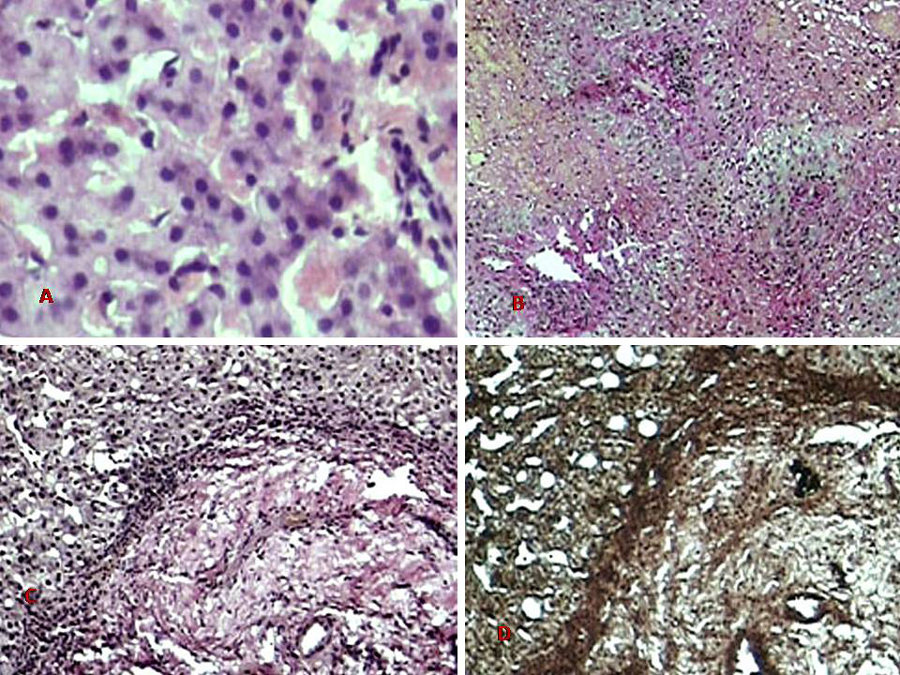
Photomicrograph showing centrizonal congestion and mild degeneration. (H & E X 400)
DISCUSSION
BCS is less common in children as compared to adults. In a study on 177 cases of this syndrome, only 5% were found to be below 12 years of age [2]. The largest paediatric series of 9 cases described south African children with a membranous obstruction of the inferior vena cava [3]. More than one half of the cases of classic BCS occur between the ages of 20 and 39 years, whereas the largest aetiopathological classification of BCS in an eastern Indian population showed the mean age at presentation to be 32.7 +/-10.36 years (range 12-60 years) with a M:F ratio = 21:9 [4]. A chronic presentation is more frequent [2]. Doppler ultrasound, venography and liver biopsy are very helpful in its diagnosis.
The BCS is usually associated with a hypercoagulable state and the other causes can be membranes, neoplasia, infections, trauma, total parenteral nutrition, etc. The primary Budd-Chiari syndrome is related to the thrombosis of the hepatic veins or the terminal portion of the inferior vena cava. This rare disease is usually caused by multiple concurrent factors which include acquired and inherited thrombophilias. Half of the patients with the primary Budd-Chiari syndrome are affected with a myeloproliferative disease, the recognition of which is largely based on the assessment of the V617F Janus Tyrosine Kinase 2 (JAK2) mutation in the peripheral granulocytes [5].
In a long term follow up study which was done over 22 years, a total of 62 patients with primary BCS were followed up in a tertiary hospital. They identified an acquired cause of BCS in 40 out of 62 patients (64.5%), whereas in 6 patients (9.7%), no identifiable cause was found. One or more thrombophilia causes were identified in 56 patients (90.3%). In 19 patients with myeloproliferative diseases, 15 had undergone the Janus tyrosine kinase 2 mutation analyses and the Janus tyrosine kinase 2 positivity was found in 10 patients. In the regression analysis, portal vein thrombosis was found to be the only indicator of mortality, with an estimated instantaneous risk of 8.4 [6].
A diagnosis of Budd-Chiari syndrome should be considered in any patient who presents with acute or chronic liver disease, as the clinical manifestations are extremely diverse. The most common cause in adults is thrombosis, which is secondary to an underlying myeloproliferative disease and in children, the most common cause is a membranous obstruction of the inferior vena cava [7]. In the present case, the aetiology remained idiopathic. The liver biopsy in the acute lesions after the hepatic vein thrombosis showed dilated veins and sinusoids with variable degrees of necrosis, followed by a chronic phase with collagenization of the sinusoids and the formation of a fibrous septa which connected the hepatic veins and spared the portal triads, which was known as venocentric cirrhosis. This accompanied the loss of the contiguous hepatocytes. The histological features cannot be distinguished from heart failure and constrictive pericarditis [8].
Another close histological differential diagnosis of BCS is venoocclusive disease, which is characterized pathologically by the fibrous occlusion of the small branches of the hepatic vein (centri and sublobular), which is caused by pyrozolidine alkaloids, transplants, chemotherapy, arsenic, heroin, etc. Although the liver biopsy in this condition also shows acute and chronic venous congestions, a definitive radiological evidence of an obstruction in the hepatic venous drainage confirms a diagnosis of BCS [9].
A liver biopsy can also be used as a guide for the therapy, with the presence of necrosis, which suggests a need for porto-systemic shunts, whereas an extensive fibrosis favours a liver transplant as the treatment of choice [10]. Transjuglar portosystemic shunts have also been used to treat these patients [11].
To conclude, this case report highlights a rare case of BCS in a child. A high index of clinical suspicion, along with a radiological aid and a histopathological correlation, can lead to an early diagnosis and an appropriate management in such cases.
[1]. Gentil-Kocher S, Benard O, Brunelle F, Hadchouel M, Maillard JN, Valayer J, The Budd-Chiari syndrome in children: a report of 22 casesJ Pediatr 1988 113:30-38. [Google Scholar]
[2]. Dilawari JB, Bambrey P, Chawla Y, Upjeet K, Bhusnurmath SR, Malhotra HS, The hepatic outflow obstruction (the Budd-Chiari syndrome)Medicine 1994 73:21-36. [Google Scholar]
[3]. Hoffman HD, Stockland B, von der Heyden U., Membranous obstruction of the inferior vena cava with the Budd-Chiari syndrome in children: a report of nine casesJ Pediatr Gastroenterol Nutr 1987 6(6):878-84. [Google Scholar]
[4]. De BK, De KK, Sen S, Biswas PK, Das TK, Das S, An etiology based prevalence of the Budd-Chiari syndrome in eastern IndiaJ Assoc Physicians India 2000 48(8):800-03. [Google Scholar]
[5]. Plessier A, Valla DC, The Budd-Chiari syndromeSemin Liver Dis 2008 Aug 28(3):259-69. [Google Scholar]
[6]. Harmanci O, Kav T, Peynircioglu B, Buyukasik Y, Sokmensuer C, Bayraktar Y, A long-term follow-up study in the Budd-Chiari syndrome: a single-center experience in 22 yearsJ Clin Gastroenterol 2012 Apr 10 [Epub ahead of print] [Google Scholar]
[7]. Henderson JM, Warren WD, Millikan WJ Jr, Surgical options, hematological evaluations and pathologic changes in the Budd chiari syndromeAm J Surg 1990 159:41-50. [Google Scholar]
[8]. Kage M, Arakawa M, Kojiro M, Okuda K, Histopathology of the membranous obstruction of the inferior vena cava in the Budd-Chiari SyndromeGastroentrology 1992 102:2081-90. [Google Scholar]
[9]. Alpert LI, Veno-occlusive disease of the liver which was associated with oral contraceptives: a case report and review of the literatureHum Pathol 1976 7:709-18. [Google Scholar]
[10]. Milliken WJ Jr, Henderson JM, Sewell CW, Cranford CA Jr, An approach to the spectrum of the Budd-Chiari syndrome: which patients require a portal decompression?Am J Surg 1985 149:167-76. [Google Scholar]
[11]. Carnevale FC, Caldas J GMP, Maksoud J G, A transjugular intrahepatic portosystemic shunt in a child with the Budd-Chiari syndrome: a technical modification and an extended follow upCardiovascular and Interventional Radiology 2002 25:224-26. [Google Scholar]