Cavernous Hemangioma of the Spinal Cord: A Rare Case
Sonti Sulochana1, Meenakshi Sundaram2
1 Assistant Professor, Department of Pathology, Saveetha Medical College, Thandalam, Chennai-602105, Tamil Nadu, India.
2 Assistant Professor, Department of Pathology, Saveetha Medical College, Thandalam, Chennai-602105, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sonti Sulochana, Assistant Professor, Department of Pathology, Saveetha Medical College, Thandalam, Chennai – 602105, India.
Phone: 09600110836
E-mail: sulochanamaster@gmail.com
Cavernous hemangiomas are composed of dilated vessels which are filled with blood. Their common sites of occurrence include the skin, liver and the superficial and the deep soft tissues. We are presenting a rare case of cavernous hemangioma of the spinal cord.
Intradural, Extramedullary, Hemangioma, Spinal cord
CASE REPORT
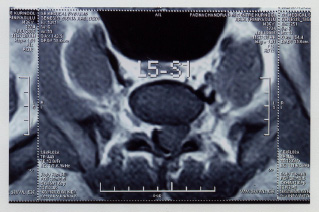
A 36 years old male presented with low back pain which radiated along the back of the thigh, which was there for 1 year. The pain was aggravated with coughing and sneezing. The routine investigations which included a haemogram, were within normal limits. MRI showed an intradural, extramedullary mass lesion which measured 2.6x2.4x1.6cm at the L5 level, with a mass effect. A radiological diagnosis of a nerve sheath tumour was made and an excision was done [Table/Fig-1].
MRI picture shows a lesion involving the spinal cord at L5-S1 level
Pathological Findings
Grossly, the specimen was found to be an oval soft tissue mass of size, 3x2.5x2cm. The cut surface was grey brown [Table/Fig-2].
Macroscopicallybrownish mass of size 3x2x1cm with brownish cut surface

Microscopically, the lesion was found to be poorly circumscribed and to be composed of irregularly dilated blood vessels which were lined by a flat endothelium [Table/Fig-3]. A diagnosis of cavernous hemangioma was made.
Microscopically the lesion showed dilated and congested vascular spaces lined by single layer of endothelial cells

DISCUSSION
Vascular tumours can be benign or malignant. The benign tumours include hemangiomas, vascular ectasia, and bacillary angiomatosis. The malignant tumours include angiosarcomas and hemangiopericytomas [1].
Cavernous hemangiomas, which are otherwise known as cavernomas, are benign vascular lesions which occur commonly in the skin, liver and in the superficial and the deep soft tissues. A cavernous hemangioma consists of irregular vascular spaces which are lined by a single layer of endothelium. Most of the cavernous hemangiomas originate from the abnormal development of the periradicular vessels [2].
Histologically, a cavernous hemangioma must be distinguished from a capillary hemangioma. A capillary hemangioma consists of a myriad of small vessels of capillary size. A cavernous angioma consists of large, dilated hyaline vascular channels which are arranged in diffuse patterns. They often show thrombosis, perivascular hemosiderin deposition and calcifications [3].
The Central Nervous System (CNS) cavernous hemangiomas are rare and they are composed of closely packed, large, sinusoid – like vascular channels with little or no intervening nervous tissue.
They can occur anywhere in the CNS, but they favour the cerebral hemisphere [4]. In the spine, cavernomas are found far more frequently in the vertebral bodies and when they involve the intradural space, they occur primarily within the spinal cord [5]. An intradural, extra medullary location is very rare, with only 23 cases being reported in the literature [6–10]. In our case, the hemangioma was located at the L5-S1 region in the intramedullary and the extradural locations.
SUMMARY
syndromes like the Mafucci’s syndrome, which is a hemangioma with multiple enchondromas, the Kasabach–Merritt syndrome which is consumption coagulopathy with a hemangioma [11] and the blue rubber bleb nevus syndrome with numerous hemangiomas in the skin and in the gastrointestinal tract [12,13]. Our case was not associated with any syndrome.
The reason for presenting this case is its rarity, as compared to the other hemangiomas. The patient was treated with surgery and he recovered well [Table/Fig-4].

[1]. Robbins Cotran Pathologic Basis of disease. Kumar et al. 2010 8e:520-25. [Google Scholar]
[2]. Journal of the Korean Neurosurgical Society 2011June 49(6):377-80. [Google Scholar]
[3]. Nowak DA, Widenka DC, Spinal intradural capillary haemangioma: a reviewEur Spine J. 2001 10:464-72.Artical/Pubmed/ChemPort [Google Scholar]
[4]. Vogiht K, Yasargil MG, Cerebral cavernous haemangiomas or cavernomas: incidence, pathology, localization, diagnosis, clinical features and treatment. Review of the literature and report of an unusual caseNeurochir. (Stuttg) 1976 19:59-68. [Google Scholar]
[5]. Guthkelch AN, Haemangiomas which involve the spinal epidural spaceJ Neurol Neurosurgery Psychiatry 1948 11:199 [Google Scholar]
[6]. Mori K, Ishii H, Tomita Y, Nakajima K, Morimoto K, Maeda M, Intraduralextramedullary spinal cavernous angioma - A case reportNeurol Med Chir (Tokyo) 1991 31:593-96.Pubmed/Chemport [Google Scholar]
[7]. Sharma R, Rout D, Radhakrishnan VV, Intradural spinal cavernomasBr J Neurosurg 1992 6:351-56.Pubmed/Chemport [Google Scholar]
[8]. Rao G P, Bhasker G, Hemaratnan A, Srinivas TV, Spinal intraduralextramedullary cavernous angiomas: a report of four cases and review of the literatureBr J Neurosurg 1997 11:228-32.Artical/Pubmed/ChemPort [Google Scholar]
[9]. Nozaki K, Nomoto T, Taagi Y, Hasimoto N, Spinal intradural extramedullary cavernous angioma. A case reportJ Neurosurg Spine 2003 99:316-19. [Google Scholar]
[10]. Fontane S, Melanson D, Cosgrove R, Bertrand G, Cavernous haemangiomas of the spinal cord: MR ImagingRadiology 1998 166:839-41.Pubmed [Google Scholar]
[11]. Kasabach HH, Merritt KK, A capillary hemangioma with extensive purpura. Report of a caseAmJ Dis child 1961 59:1063-70. [Google Scholar]
[12]. Fine RM, Derbes VJ, Clark WH Jr, The blue rubber bleb nevus syndromeArch Dermatol 1961 84:802-05. [Google Scholar]
[13]. Rice SJ, Fischer DS, The blue rubber bleb nevus syndromeArch Dermatol 1962 86:502-11. [Google Scholar]