The Management of Retrograde Peri-Implantitis: A Case Report
Jumshad B Mohamed1, Md Nazish Alam2, Gurudeep Singh3, S. C. Chandrasekaran4
1 Senior Lecturer, Department of Dentistry,
2 Senior lecturer, Department of Periodontology & Implantology,
3 Professor, Department of Dentistry,
4 Head, Department of Dentistry, Sree Balaji Dental CollegeChennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. MD. Nazish Alam, Senior Lecturer, Department of Periodontology & Implantology Sree Balaji Dental College Narayanapuram, Velachery Main Road, Chennai-100 (Tamil Nadu), India.
Phone: 91-9884325366
E-mail: dr.naz.ish.alam@gmail.com
Peri-Implantitis is defined as an inflammatory reaction with the loss of the supporting bone in the tissues which surround a functioning implant. The peri-implantitis lesions are often asymptomatic and they are usually detected during the routine recall appointments. Careful probing around the teeth and the implants should be done routinely along with the radiologic evaluation during these check-up appointments. Retrograde peri-implantitis may sometimes prove even more difficult to identify, resulting in the loss of the implant. This paper presents a report of the extensive and the meticulous management of retrograde peri-implantitis and the implant being finally restored to health and the full functional status.
Retrograde peri-implantitis, Peri-apical lesion, Platelet rich-fibrin
Introduction
Retrograde peri-Implantitis (RPI) is defined as a clinically symptomatic periapical lesion which is diagnosed as a radiolucency that develops shortly after an implant insertion, in which the coronal portion of the implant achieves a normal bone-implant interface [1].This condition was first described by McAllister et al., [2]. The endodontic periapical pathology which was associated with either the previously extracted or the neighbouring teeth was present more often (three times) in cases of peri-implantitis as compared to that in the successfully integrated implants, suggesting that the endodontic pathology was the most likely primary aetiology. A recent article which was written by Zhou et al., [3]. Supports this theory because their reported incidence of peri-Implantitis on the implants which were adjacent to an endodontically treated tooth was 7.8%, which is higher than the overall reported incidence. Sussman[4] proposed 2 pathways that may lead to RPI: Type 1 (implant to the tooth) and type 2 (tooth to the implant). Type 1 RPI occurs when the osteotomy preparation causes direct or indirect damage to the adjacent tooth, resulting in devitalization of the tooth pulp and the periapical pathology. Subsequently, the periapically infected tooth inhibits the osseointegration of the implant. Type 2 RPI occurs when an adjacent tooth with a periapical pathology contaminates the fixture and interferes with the osseointegration of the implant.
Case Report
A 27-year-old male patient reported to the Department Of Periodontology at Sree Balaji Dental College and Hospital for the treatment of a fractured tooth #22 [Table/Fig-1]. His dental history revealed a previous trauma for which he was endodontically treated in relation to teeth #11, #21 and #22; the crown of the tooth #22 was subsequently fractured [Table/Fig-2]. The patient was given the option of a fixed partial denture, a cast and a post, and a dental implant. The patient opted for the treatment with a dental implant in relation to #22. Hence, an immediate extraction was done, followed by a dental implant, which was placed in tooth #22. Using a periotome, an atraumatic extraction was done to preserve the structural integrity of the socket [Table/Fig-3]. The socket was completely debrided [Table/Fig-4] and repeated irrigation by using saline and povidone iodine solution was done. This was followed by the placement of the dental implant in the #22 region [Table/Fig-5,6]. In relation to tooth #21, the endodontic treatment was faulty and the patient was advised a retreatment immediately. The patient delayed the endodontic treatment, which led to a root resorption. Also, the patient did not turn up for a recall appointment, leading to the retrograde peri-implantitis. The patient reported after 4 months, at which time the site appeared healthy, but radiographically, a periapical radiolucency was seen in relation to tooth #21 [Table/Fig-7], which extended to the apical portion of the dental implant, but the implant was not mobile. Hence, we felt that it was prudent to treat the site with periapical surgery for accessing the site as well as the debridement and detoxification of the implant site was involved.

Intra-Oral Periapical Radiograph




Immediate Implant Placement

Retrograde Peri-Implantitis

Management of The RPI
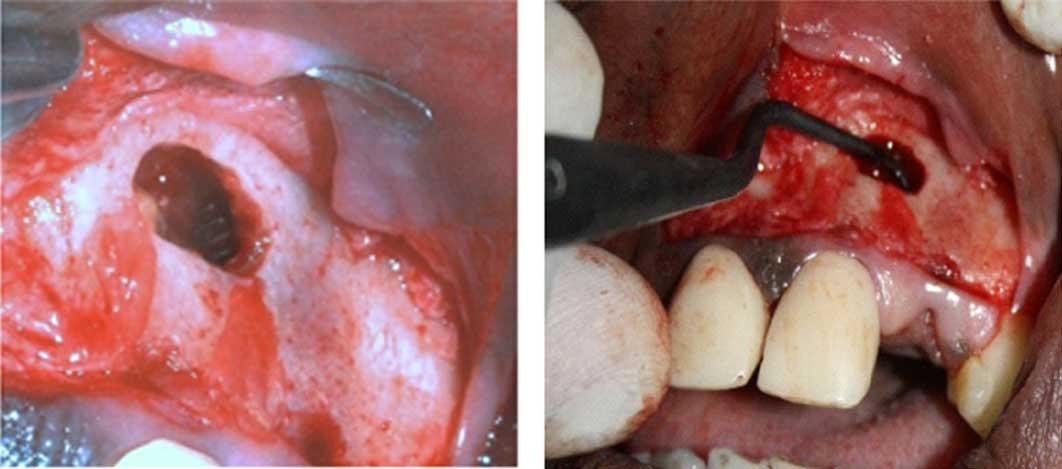
Under local anaesthesia, the patient preparation was done. A horizontal incision was placed through the attached gingiva, about 2 mm from the gingival margin and extending from the tooth #11 to the tooth #23. The full thickness flap was raised to access the periapical region in relation to tooth #21 and the implant in relation to #22. By using a round surgical bur, the periapical site was opened through the bone to access the periapical region of tooth #21. A complete debridement and detoxification [Table/Fig-8] was done around the affected site of the implant by using a Universal implant Deplaquer (Straumann USA). The over extension of the gutta percha was trimmed to prevent further irritation, which had led to the periapical pathology. By using a xenograft, the surgical site was packed and closed with Platelet Rich Fibrin (PRF), which acted as a bandage for the surgical site [Table/Fig-9]. By using a 3-0 silk suture, the site was approximated and the retreatment of 11 and 21 was done endodontically. A post operative review [Table/Fig-10] was continuously done and finally, the implant was loaded at 4 months. Post management 1 year follow up was reviewed [Table/Fig-11].
Debridement/Detoxification of Implant Surface

Periapical Surgery 3 Month Retreatment Review

Final Prosthesis (1-Year Review)

Discussion
Most of the case reports suggest that the residual bacteria in a radiographically healed socket or in an adjacent periapical lesion are the main causes of RPI. It has been further suggested that the endodontic bacteria can be reactivated during an implant osteotomy, leading to an implant infection [2,5]. Various techniques have been used, such as debridement only, a combination of debridement with the grafting material, detoxification of the infected implant surfaces or apicoectomy. The treatment goals of RPI include the elimination of the infection, resolution of the lesion, and ultimately, the implant survival. Re-osseointegration requires implant surface detoxification and the application of chemotherapeutic agents such as tetracycline, chlorhexidinegluconate, and citric acid [6]. Implant apicoectomy has been thoroughly covered in many case reports [7,8], although Ayangco and Sheridan [9] suggested that the scratching of the implant surface in such a location might not be crucial. Ataullah et al.,[10] suggested that the surface debridement should be carried out with extreme care, to prevent damage to the surface of the fixture. In this case report, the retrograde spread of the infection from the adjacent tooth led to the infection in the dental implant site. The management of this case required accessing of the site through the alveolar bone, a peri-apical surgery. Although this was an invasive procedure, the outcome of the surgery helped in preventing the implant from failing and it helped in achieving the required function and aesthetics, which were of concern to the patient.
[1]. Quirynen M, Gijbels F, Jacobs R, An infected jawbone site which compromised a successful osseointegrationPeriodontol 2000 2003 33:129-44. [Google Scholar]
[2]. McAllister BS, Masters D, Meffert RM, The treatment of the implants which demonstrated periapical radiolucenciesPract Periodontics Aesthet Dent 1992 4:37-41. [Google Scholar]
[3]. Zhou W, Han C, Li D, Li Y, Song Y, Zhao Y, The endodontic treatment of teeth induces retrograde peri-implantitisClin Oral Implants Res 2009 20:1326-32. [Google Scholar]
[4]. Sussman HI, The periapical implant pathologyJ Oral Implantol 1998 24:133-38. [Google Scholar]
[5]. Piattelli A, Scarano A, Balleri P, Favero GA, The clinical and the histologic evaluation of an active “implant periapical lesion”: A case reportInt J Oral Maxillofac Implants 1998 13:713-16. [Google Scholar]
[6]. Meffert RM, How to treat the ailing and the failing implantsImplant Dent 1992 1:25-33. [Google Scholar]
[7]. Shaffer MD, Juruaz DA, Haggerty PC, The effect of periradicular endodontic pathosis on the apical region of the adjacent implantsOral Surg Oral Med Oral Pathol Oral Radiol Endod 1998 86:578-81. [Google Scholar]
[8]. Dahlin C, Nikfarid H, Alse’n B, Kashani H, Apical peri-Implantitis: the possible predisposing factors, case reports, and the surgical treatment suggestionsClin Implant Dent Relat Res 2009 11:222-27. [Google Scholar]
[9]. Ayangco L, Sheridan PJ, The development and the treatment of retrograde peri-implantitis which involved a site with a history of failed endodontic and apicoectomy procedures: A series of reportsInt J Oral Maxillofac Implants 2001 16:412-17. [Google Scholar]
[10]. Ataullah K, Chee LF, Peng LL, Lung HH, The management of retrograde peri-implantitis: A clinical case reportJ Oral Implantol 2006 32:308-12. [Google Scholar]