Introduction
Osteosarcoma (OS), which is sometimes referred to as osteogenic sarcoma, is the most common primary bone tumour in adolescents and young adults. Mandibular and maxillary osteosarcomas account for 6% to 9% of all the osteosarcomas. Mandibular OS is often considered as a distinct entity because of its predilection to older patients (mean age: 34 to 36 years) [1]. The WHO has recognized several variants of OS that differ in location, clinical behaviour, and the degree of cytologic atypia. The most frequently occurring variant is the classical osteosarcoma which arises centrally within the bone [2]. It is a tumour that can occur in any bone but which most commonly occurs in the long bones of the extremities, near the metaphyseal growth plates. Osteosarcomas accounts for about 20% of all the sarcomas and about 4%-6% occur in the maxillofacial region. Sometimes, they are referred to as gnathic osteosarcomas [3,4]. The purpose behind writing of this case report was to highlight the diagnostic difficulties encountered in a patient of OS which affected the mandible and presented as a swelling in the lower right third molar region.
Case Report
A 29-year female reported with a diffuse swelling and pain in the right posterior mandibular molar region and numbness of the right side of the lower lip since two months. The pain was dull and intermittent. It was relieved after medications. The patient gave a history of extraction of the lower right third molar, one month before, for the same complaint, but there was no relief. The patient did not give a history of excessive abnormal bleeding after the extraction of the tooth. The past medical history was noncontributory.
On extraoral examination, a diffuse swelling which caused slight asymmetry of the face was observed. There was paresthaesia of the right side of the lower lip, which was clinically confirmed. The overlying skin appeared normal on inspection as well as on palpation. The right submandibular lymphnodes were palpable, mobile and slightly tender. The intraoral swelling could be appreciated on pressure and it was slightly tender.
The intra-oral examination revealed an ulcerative lesion (may be because of an unhealed extraction socket) which was covered by slough, in the lower right third molar region. The size of the lesion was 1x1cm, it had inflamed margins and it was covered with slough. The overlying mucosa was reddened on the buccal and the lingual sides. The buccal and the lingual cortical plates were found to be intact and bulbous on palpation. The mass was mildly tender and without any signs of active bleeding [Table/Fig-1].
Intraoral Photograph showing swelling with ulceration, reddish margins and slough in lower right third molar region

Based on the clinical findings, a provisional diagnosis of an inflammatory lesion was made.
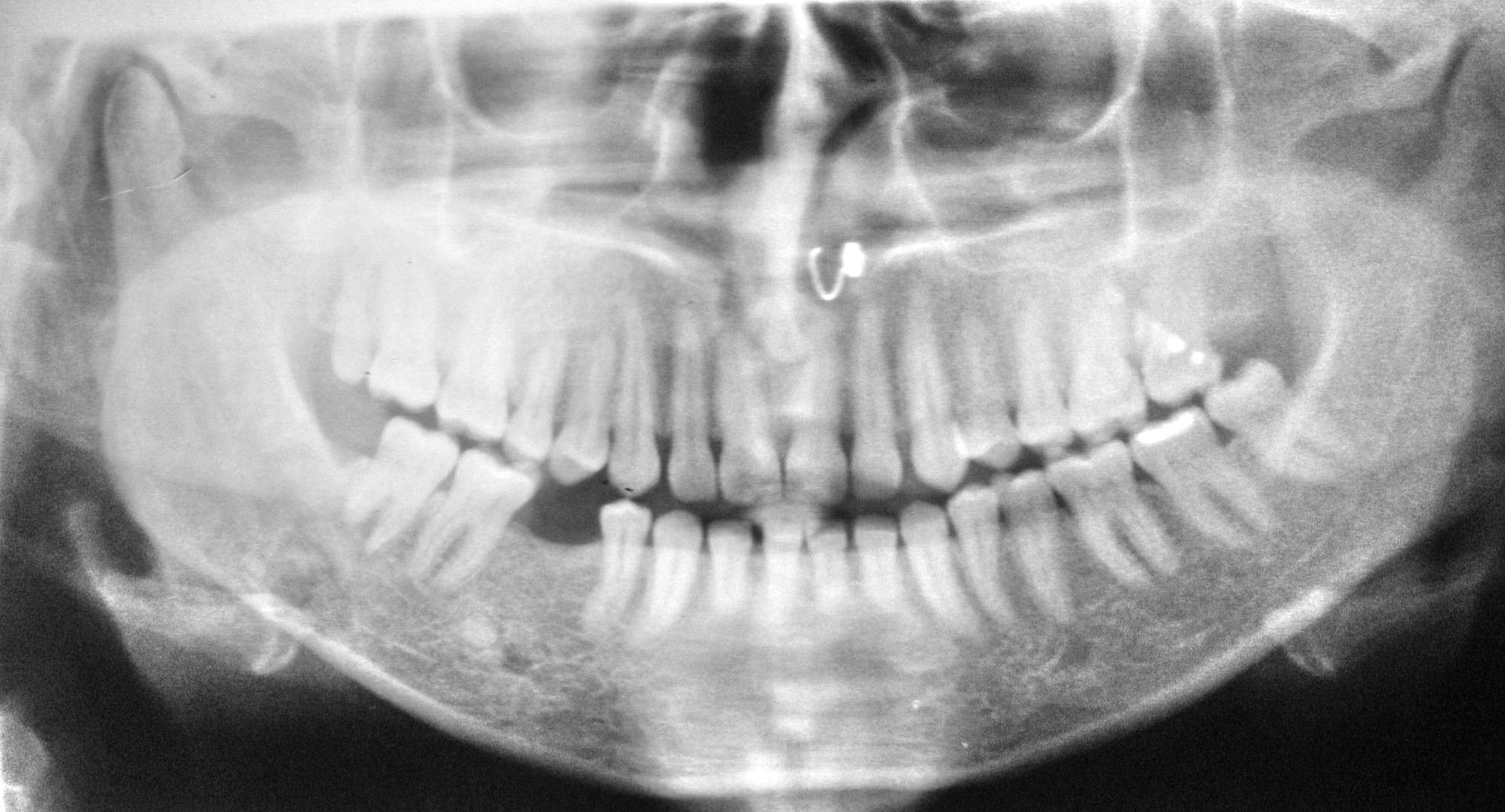
Primary radiographic investigations were carried out to rule out the presence of any root piece or the fracture of the cortical plates. The Intra-oral Periapical (IOPA) radiograph and the Orthopentamogram (OPG) showed an unhealed extraction socket with 48, with no evidence of root pieces or fractured fragments of bone.
There was evidence of a diffusely radiolucent and a radio-opaque lesion (mixed lesion) which extended from the distal root socket of the third molar region to the mesial root of the second molar and from 0.5cm above the inferior border of the mandible up to the apical 1/3rd of root. The lesion appeared to invade in to the surrounding bone (ragged borders). The second molar showed resorption of the distal root and loss of the lamina dura on the mesial root. There was no evidence of either caries with first and second molars or of periodontal space widening with the first molar. These findings, along with the paresthaesia of the lower lip, provoked us to give a serious thought to this clinical entity as osteomyelitis or other mixed lesions like metastatic carcinoma or even sarcoma [Table/Fig-2 and 3].
IOPA Radiograph showing recently extracted tooth socket along with resorption of roots of adjacent tooth

OPG showing diffuse radiolucent lesion in the periapical region of socket of right Mandibular third molar
After the patient’s written consent, a complete haemogram was obtained and an incisional biopsy was performed under local Anaesthesia.
Histopathology
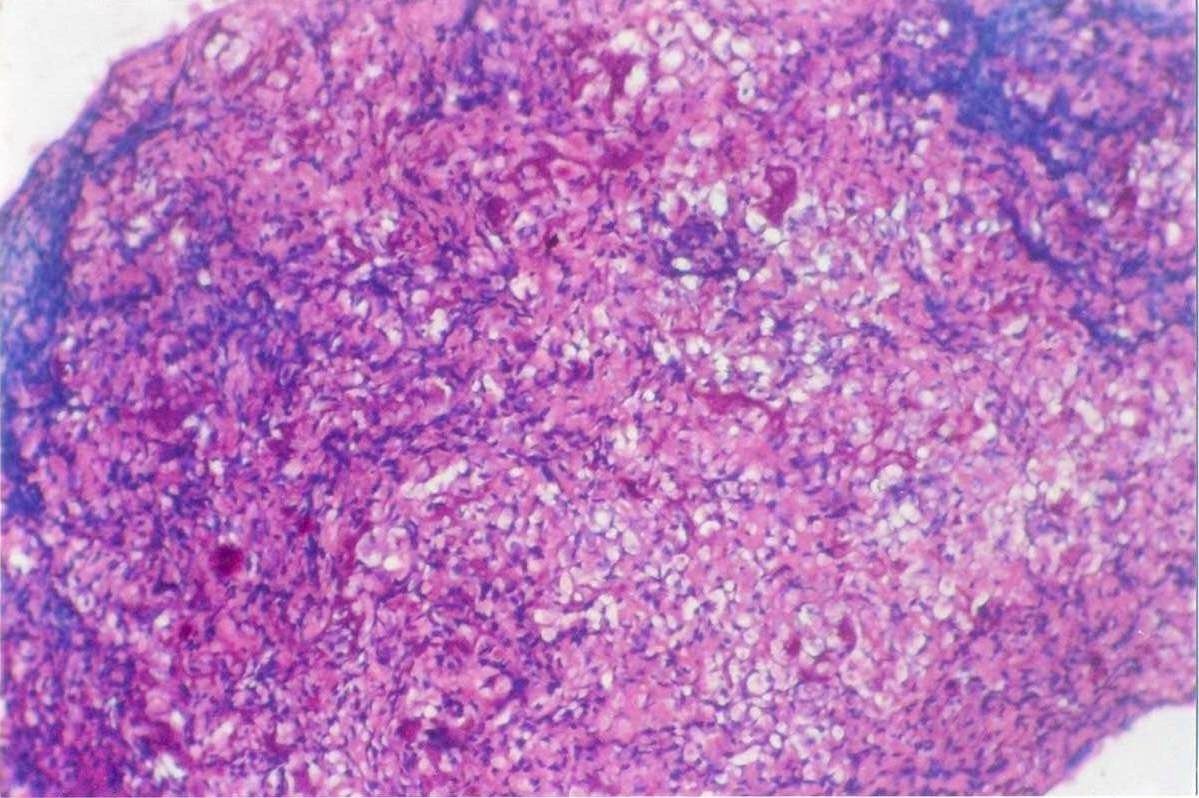
The histopathological examination revealed a parakeratinized, stratified squamous epithelium with signs of proliferation, along with fibrocellular connective tissue with abundance of blood vessels and chronic inflammatory cells. The deeper areas of the section showed tissues which were composed of large sized pleomorphic cells with hyperchromatic nuclei which were arranged in an irregular fashion. These cells were malignant osteoblasts. The tumour cells were found to be admixed with some spindle shaped cells and they were found to deposit atypical eosinophilic osteoid. Few giant cells were also noticed. These microscopic findings were suggestive of osteoblastic osteosarcoma, and a final diagnosis was made [Table/Fig-4].
Photomicrograph showing proliferation of sarcomatous components with malignant osteoid. (20X, H &E Stain)
After the confirmation of the diagnosis, the patient was referred to Tata Memorial Hospital, Mumbai, India. Other investigations were carried out, like chest radiographs and lung and body scans, which were negative for primary as well as metastatic lesions. The patient was treated by hemimandibulectomy of the affected side, which was supported by chemotherapy. The resected margins of the lesion were negative for tumour, but still the patient was given adjuvant chemotherapy to improve the prognosis.
Discussion
Osteosarcoma is a rare but highly malignant bone tumour. Excluding multiple myeloma, it is the most frequent primary malignant lesion of the bone in patients who are below 40 years of age. Osteosarcomas account for about 20% of all the sarcomas and about 4%-6% occur in the maxillofacial region. The OS of the jaws usually presents at a later age than the OSs which occur at other locations and it has a lower incidence of metastasis and a higher survival rate. But the local recurrence is common and it is often uncontrollable, leading to the death of the patient [4,5,6].
The exact cause of OS is unknown. However, a number of risk factors do exist. The role of the rapid bone growth appears to predispose the patients to develop OS. There are cases of OS of the jaws which are associated with other bone diseases, such as Paget’s disease, fibrous dysplasia, enchondromatosis and hereditary multiple exostosis and with previous radiation therapy to the jaw region. This may suggest an association between OS in general and excessive bone cellular activity. Because a substantial increase in the incidence of OS occurs in patients with retinoblastoma, it is now thought that the RB1 gene causes both the diseases [7].
The characteristic clinical presentation of OS of the long bones is bone pain. In the jaw lesions, pain is not a prominent feature and swelling and paresthaesia of the involved region is the commonest presenting complaint. The radiographic appearance varies, depending on the inter-relationship between the destruction of the pre-existent cortical or medullary bone, calcification or new bone production and periosteal new bone formation. Accordingly, the radiographic appearance may be purely osteolytic, mixed or osteogenic (sun-ray appearance). Widening of the periodontal ligament space or attenuation of the lamina dura around the OS are the common radiographic findings [5,8].
The most common variant of OS is the conventional type (i.e., osteoblastic, fibroblastic and chondroblastic) [2]. The patient who has been reported here was diagnosed as having osteoblastic osteosarcoma. The IOPA-radiograph and OPG revealed characteristic features like a stippled bone pattern and destruction of the cortical outlines though perpendicular speculations of the periosteal new bone was absent [9].
Osteosarcoma spreads microscopically through the narrow spaces. Another possible route is the mandibular canal and the structures which connect the intra-osseous components and soft tissues, such as the periodontal ligament, the mental nerve and the inferior alveolar nerve, which may facilitate the spread of an intra-osseous lesion in to the adjacent soft tissues. It may appear extra-osseously through a recently extracted tooth socket, as was observed in our case [7] or by perforating the cortical plates.
In the case which has been presented here, no metastasis was found in the conventional antero-posterior and the lateral chest radiographs. Also, the lung and body scan did not reveal any signs of metastasis. The patient is still on regular review at this center and she responded well to the treatment.
The literature indicates that osteosarcoma of the jaw differs from osteosarcoma of the long bones in its biological behaviour, even though they have the same histological appearance. Because of the differences in the tumour characteristics, the introduction of chemotherapy did not dramatically alter the prognosis of osteosarcoma of the jaw. Early diagnosis and radical surgery are the keys to high survival rates [6].
Guadagnolo et al. [9] described the outcome of the treatment in OS patients. Combined treatment in the form of radical surgery, followed by radiotherapy and/or chemotherapy, were found to result in a good prognosis. Similar findings were reported by LeCornu et al. [10], Chindia M L. [11] and Demicco et al. [12]. Angiero et al. stressed the importance of an early diagnosis for this malignant neoplasm, as both of their patients died in the early phase of the therapy [13].
Because of the complexity of the clinical features, the radiographic appearances and their rarity in the daily clinical practice, the preoperative diagnosis of osteosarcoma is often difficult. The final diagnosis can be made only after doing histopathologic investigations. This case was diagnosed only after a histopathological examination of the lesion.
Conclusion
A thorough clinical, radiographical and histopathological evaluation of any suspicious lesion helps in diagnosing its pathology at an early stage, especially if the lesion turns out to be malignant. Here, we would like to stress the importance of an early diagnosis of gnathic osteosarcoma and its management. The case which we have presented, showed a remarkable recovery after radical surgery and adjuvant chemotherapy. These help in increasing the life expectancy of the patients.
[1]. Murphey MD, Robbin MR, McRae GA, The many faces of osteosarcomaRadiographics 1997 17:1205-31. [Google Scholar]
[2]. Bennett JH, Thomas G, Evans AW, Speight PM, Osteosarcoma of the jaws: A 30-year retrospective reviewOral Surg Oral Med Oral Pathol Oral Radiol Endod 2000 90:323-33. [Google Scholar]
[3]. August M, Magennis P, Dewitt D, Osteogenic sarcoma of the jaws: factors which influence the prognosisInt. J. Oral Maxillofac Surg. 1997 26:198-204. [Google Scholar]
[4]. Nissanka EH, Amaratunge EAPD, Tilakaratne WM, Clinicopathologic analysis of osteosarcoma of the jaw bonesOral Diseases 2007 13(1):82-87. [Google Scholar]
[5]. Ogunlewe MO, Oluseyi FA, Wasin LA, Akinola LL, Olutayo J, Osteogenic sarcoma of the jaw bones: a single institutional experience over a 21 year periodOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 101:76-81. [Google Scholar]
[6]. Mardinger O, Givol N, Talmi YP, Taicher S, Osteosarcoma of the jaw- The Chaim Sheba Medical Center experienceOral Surg Oral Med Oral Pathol Oral Radiol Endod 2001 91:445-51. [Google Scholar]
[7]. Petrikowski GC, Pharoahi MJ, Lee L, Grace MGA, Radiographic differentiation of osteogenic sarcoma, osteomyelitis and fibrous dysplasia of the jawsOral Surg Oral Med Oral Pathol Oral Radiol Endod 1995 80:744-50. [Google Scholar]
[8]. Nakayama E, Sugiura K, Ishibashi H, Oobu K, Kobayashi I, Yoshiura K, The clinical and diagnostic imaging findings of osteosarcoma of the jawDentomaxillofacial Radiology 2005 34:182-88. [Google Scholar]
[9]. Guadagnolo BA, Zagars GK, Raymond AK, Benjamin RS, Sturgis EM, Osteosarcoma of the jaw/craniofacial region: outcomes after multimodality treatmentCancer 2009 Jul 15 115(14):3262-70. [Google Scholar]
[10]. LeCornu MG, Chuang SK, Kaban LB, August M, Osteosarcoma of the jaws: factors which influence the prognosisJ Oral and Maxillofacial Surg 2011 69(9):2368-75. [Google Scholar]
[11]. Chindia ML, Osteosarcoma of the jaw bonesOral oncology 2001 37(7):545-47. [Google Scholar]
[12]. Demicco EG, Deshpande V, Nielsen GP, Kattapuram SV, Rosenberg AE, Well-differentiated osteosarcoma of the jaw bones: A clinicopathologic study of 15 casesAmerican J Surgical Pathology 2010 34(11):1647-55. [Google Scholar]
[13]. Angiero F, Moltrasio F, Cattoretti G, Valente MG, Clinical and histopathological profiles of primary or secondary osteosarcoma of the jawsAnticancer Research 2011 31(12):4485-89. [Google Scholar]