This is a case report of the presentation and the management of an apicomarginal defect which was associated with a root end fracture in an endodontically treated tooth. In spite of a successful Root Canal Treatment (RCT), if the fractured root end is left intact, considering inadverdent ankylosis or resorption, it may progress to the development of a bony dehiscence.
Introduction
An apicomarginal defect can be defined as a complete loss of the buccal alveolus which extends from what was once the crestal bone, to the apex of the tooth [1]. The use of surgical techniques to successfully repair periapical bony defects has been welldocumented. The use of a technique to repair the apicomarginal defects, however, has not been well-established.
A number of factors affect the results of an endodontic surgery. It is well known that a marginal bone loss impairs the prognosis. When there is an osseous defect which extends from the periapical region to the alveolar crest to the tooth i.e., a combined endodontic-periodontic lesion, an endodontic surgery which is done in this region may fail. The failure may be caused by an apicomarginal communication which provides avenues for a microbial invasion of the apex [2-3].
Skoglund and Persson [2] suggested that such defects require a combined endodontic-periodontic treatment; however, they reported a success rate of only 37% where this defect existed. Hirsch and colleagues [3] reported a success rate of only 27% with complete loss of the buccal plate. The presence of apicomarginal defects obviously decreases the chances of a success; many practioners therefore recommend extraction.
This case report represents the correct diagnosis and the successful management of an apicomariginal defect which was associated with the fractured root end of a maxillary central incisor tooth.
Case Report
A 32-years-old female patient reported to the Out Patients Department (OPD) of JSS Dental College and Hospital with the chief complaint of a persistent, chronic and dull aching pain with periodic exacerbation and remission and tenderness on biting in the maxillary left central incisor, of 15 years duration. She reported gingival bleeding and pus drainage with a variable intensity, which was there since some time.
Her history revealed she had a trauma to her upper left central incisors at the age of 17-years, while climbing a stair case in a trade fair stall. As a result of the trauma, the maxillary left central incisor subluxated in the socket, with an accompanying soft tissue injury. Subsequently, the patient reported to the nearby dental clinic where it was diagnosed as a subluxated tooth with the fracture of the apical one third of the root end. The tooth was tender and it was severely mobile when it was presented to the nearby dentist. As a treatment protocol, the attending dentist splinted the tooth by using a resin reinforced wire splint and performed Root Canal Treatment (RCT) after 15 days of the event. The splint was stable for 3 months and finally, it got fractured during brushing. The patient didn’t return to the dentist for the correction/re-splinting of the splint.
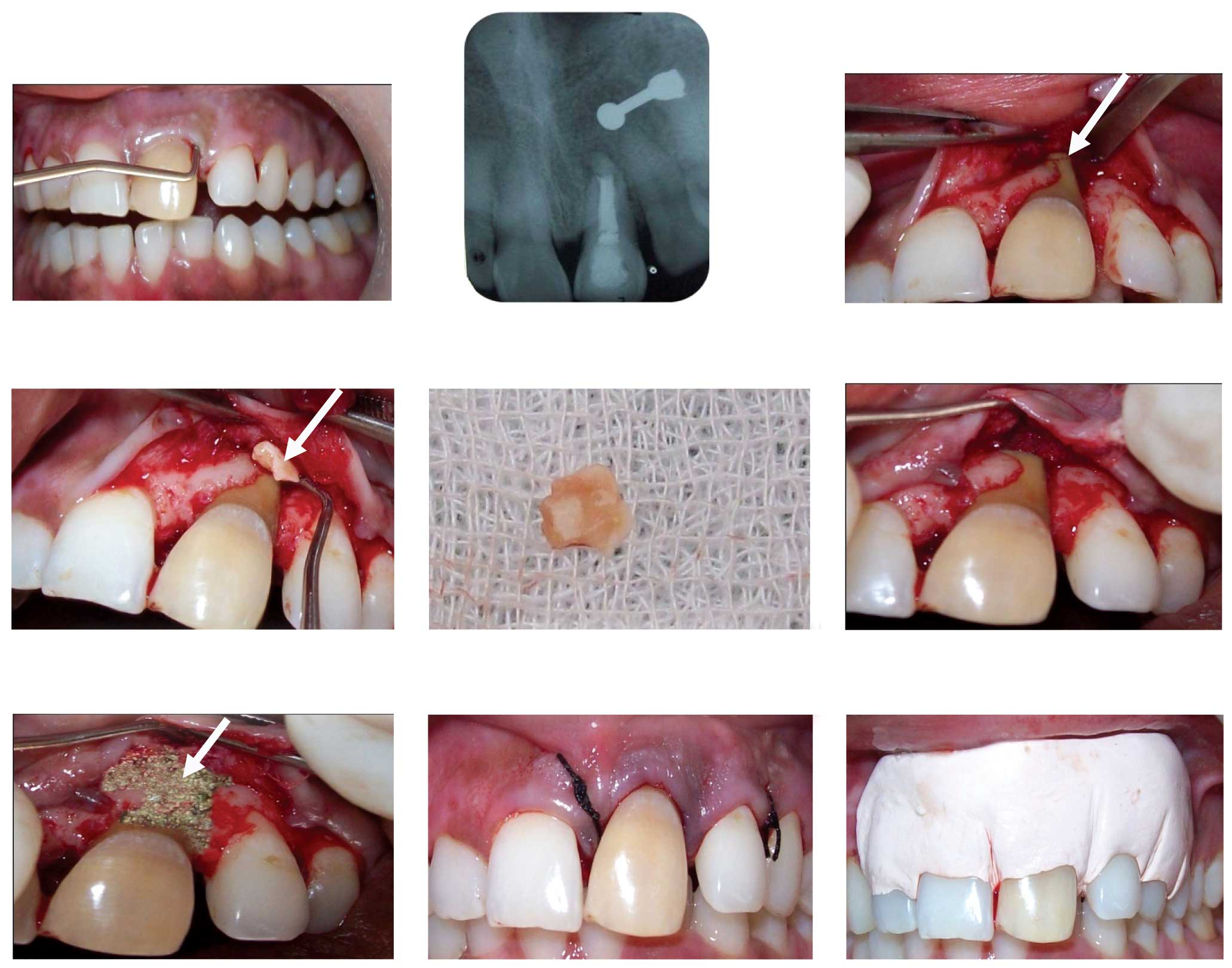
After 15 years, when she presented to our clinic, the intra-oral examination of the involved tooth revealed that it was discoloured and tender on percussion. There was a 12mm pocket which was present on the distobuccal/buccal aspect of the tooth and a 6mm pocket on the mesiobuccal aspect of the tooth, with a draining sinus in the muco-buccal fold of #21 [Table/Fig-1]. The tooth was Grade I mobile, with no evidence of a gingival recession. There was a mild pathologic migration of the tooth, consequently resulting in mesial tilting and in migration, leading to a 2 mm diastema between #21 and #22. There was no occlusal trauma from the lower anterior teeth. Overall, the oral hygiene of the patient was good. A Radiographic Analysis (IOPAR) showed a successful RCT with a fractured root end #21, with mild bone loss in the interdental area of the involved tooth [Table/Fig-2]. Subsequently, after observing a radiographic evidence of minimal bone loss in the interdental region and a deep pocket which was present in the mesiobuccal/buccal region, on probing the tooth clinically, we diagnosed the case as chronic localized periodontitis with a apicomarginal defect which was associated with a root end fracture with respect to 21.
IOPAR of The Involved Tooth

The Treatment Protocol and Follow-up
The Phase I therapy: The phase I therapy involved full mouth scaling and root planning of the involved tooth. The patient was advised to use 0.2% chlorhexidine twice a day for one week and she was under antibiotic coverage: Amoxicillin and Metronidazole [Cap AMOX 500 mg TID and Tab FLAGYL 400 mg TID] for 7 days. The patient was reviewed after 5 days and on examination, it was found that no draining sinus was present.
The Phase II therapy: The patient was appointed for surgery. The patient was anaesthetized by using a maxillary and an anterior superior alveolar nerve block and a nasopalatine nerve block by using 2% lidocaine with 80,000 adrenaline. A papilla preservation flap was reflected with respect to #2 and a conventional flap was reflected with respect to #11 and #22.
The flap reflection revealed abundant granulation tissue and there was a complete bony buccal dehiscence which extended to the root end of #21; the other areas of the tooth had a normal bony anatomy [Table/Fig-3]. The fractured root segment was visualized and the fragment was mobilized with a bone chisel and a periosteal elevator [Table/Fig-4]. The root fragment was then retrieved with the help of a curette and beaked forceps [Table/Fig-5]. A thorough debridement was done and the root end gutta percha was burnished by using a ball burnisher [Table/Fig-6]. There was no need for a retrograde filling of amalgam, as the gutta percha filling was satisfactory. The bone defect was filled with “Periobone G®” [Table/Fig-7].

Mobilizing Fractured Root Segment


Complete Buccal Dehiscence

Placement of Bone Graft (Periobone G)

Interrupted sutures were placed by using 3-0 silk and a periodontal pack was placed [Table/Fig-8 and 9]. The patient was advised to continue with the remaining course of antibiotics for the next 2 days, along with the analgesics [Tab HIFENAC-P BID] for the next 3 days. The suture removal was done after 7 days. Further, in the follow-up recall appointments, she presented with a complete remission of the lesion and an uneventful healing of the sinus tract [Table/Fig-10 and 11].


Post Operative 3 Weeks (Palatal)

Post Operative 3 Weeks (Labial)

Discussion
Mid-root fractures occur most frequently in the upper anterior teeth due to their position in the arch. These fractures are generally transverse to oblique and they may be single or multiple and complete or incomplete. In the present case report, there was an apical end fracture which was rare for the maxillary anterior teeth, which led to the formation an apicomarginal defect.
The initial treatment consists of repositioning of the displaced coronal segments, followed by the stabilizing of the tooth, to allow healing of the periodontal ligament which supports the coronal segment [4]. The amount of dislocation and the degree of mobility of the coronal segment affect the prognosis [5]. Achieving a stable fracture reduction is inversely proportional to the severity of the dislocation, the mobility, and the pulpal injury [5]. An endodontic intervention is required for the non- healing fractures. The following are the treatment options which had been carried out, with varied levels of success:
Root canal therapy of both the segments [6] which were done in the cases where both the fractured segments were not separated.
Root canal treatment of the coronal segment only, if this segment showed no mobility [7].
The use of an intra-radicular splint [8].
Root extrusion is a solution for the teeth with root fractures at or near the alveolar crest [9].
The placement of an endodontic implant with or without periapical surgery [10].
Extraction and subsequent replacement with prosthesis [Implant] [6].
The current recommendation for a mid-root fracture is root canal treatment of the coronal segment, only if this segment shows no mobility [7], particularly with the view that the apical segment may contain vital, healthy pulp tissue. If the root end fractured segment is left behind, it can heal by 4:
Healing with calcified tissue. Radiographically, the fracture line is discernible, but the fragments are in close contact.
Healing with interproximal connective tissue. Radiographically, the fragments appear separated by a narrow radiolucent line, and the fractured edges appear rounded.
Healing with interproximal bone and connective tissue. Radiographically, the fragments are separated by a distinct bony bridge.
Interproximal inflammatory tissue without healing. Radiographically, a widening of the fracture line and/or a developing radiolucency which corresponds to the fracture line becomes apparent
Endodontists believe in leaving back the fractured root fragment in place rather than going for its surgical removal. They expect the healing of this segment to happen eventfully. Unfortunately, not always is the healing uneventful. In the present case, the local dentist left the behind root end fracture, assuming that there would be an eventful healing. But the present case showed the persistent presence of a draining abscess since the past 15 years, which had led to the occurrence of a complete buccal dehiscence. Usually, the endodontist in practice considers the apical 1/3 fracture under good prognosis and leaves the fragment intact, but this is not acceptable from the periodontal point of view and from the long term success of the endodontic treatment. Therefore, this confirms the importance of the removal of the fractured root end and burnishing of the root end filling.
A number of factors have been known to influence the alveolar bone height after an periapical surgery [1]. A dentist must be aware of these factors, which will help them in diagnosing the condition accurately and in planning the treatment of such lesions accurately.
A study [11] was done to compare the healing responses of Platelet-Rich Plasma (PRP). PRP+, a collagen sponge and a collagen membrane, was used as a Guided Tissue Regeneration (GTR) material for the treatment of apicomarginal defects, on 30 patients. GTR which is applied to the apicomarginal defects by using PRP or a PRP+ collagen sponge, can lead to similar enhancements of the clinical outcome of periradicular surgeries in terms of the periapical healing, gain of the periodontal support and the probing depth reduction.
Conclusion
In spite of a successful RCT, if the fractured root end is left intact, considering an inadvertent ankylosis or resorption, it may progress to the development of a bony dehiscence, as the exudates can drain, either through a sinus or they can result in a periodontal pocket formation, ultimately leading to resorption of the buccal plate.
[1]. Daniel G Pompa, A guided tissue repair of the complete buccal dehiscences which were associated with periapical defects: A clinical retrospective studyJ Am Dent Assoc 1997 128:989-97. [Google Scholar]
[2]. Skoglund A, Persson G Malmo, A follow up study on apicetomized teeth with a total loss of the buccal plateOral Surg Oral Med Oral Pathol 1985 59:78-81. [Google Scholar]
[3]. Hirsch JM, Ahlstorm ULF, Henrickson PK, Periapical surgeryInt J Oral Surg 1978 8:73-185. [Google Scholar]
[4]. Andreasen FM, Andreasen JO, Root Fractures. Textbook and Color Atlas of Traumatic Injuries to the Teeth 1993 3rdCopenhagenMunksgaard [Google Scholar]
[5]. Zachrisson BU Jacobsen, I The long-term prognosis of 66 permanent anterior teeth with root fracturesScand J Dent Res 1975 83(6):345-54. [Google Scholar]
[6]. Ingle IJ, Bakland LK, Endodontics 2002 5thLondonBC Decker Inc [Google Scholar]
[7]. Flores MT, Andersson L, Andreasen JO, Bakland LK, Malmgren B, Barnett F, Guidelines for the management of traumatic dental injuries. I. Fractures and luxations of the permanent teethInternational Association of Dental Traumatol. 2007 23:66-71. [Google Scholar]
[8]. Weine FS, Altman A, Healey HJ, The treatment of fractures of the middle third of the rootASDC J Dent Child 1971 38:215-19. [Google Scholar]
[9]. Malmgren O, Malmgren B, Frykholm A, Rapid orthodontic extrusion of the crown root and the cervical root of fractured teethEndod Dent Traumatol 1991 7:49-54. [Google Scholar]
[10]. Linkow LI, The theories and the technique of oral implantology-2 1970 Saint LouisMosby Co [Google Scholar]
[11]. Goyal B, Tewari S, Duhan J, Sehgal PK, Comparative evaluation of the platelet-rich plasma and the guided tissue regeneration membrane in the healing of apicomarginal defects: a clinical studyJ Endod. 2011 Jun 37(6):773-80. [Google Scholar]