An Adult Recurrent Diaphragmatic Hernia with a Near Complete Defect: A Rare Scenario
N. Sathyanarayana1, Ranjith M. Rao2, Shivaprasada B.K. Rai3
1 Associate Professor, Department of Surgery, Kasturba Medical College, Light House Hill Road, Mangalore, Karnataka, India 575001.
2 Assistant Professor, Department of Surgery, Kasturba Medical College, Light House Hill Road, Mangalore, Karnataka, India 575001.
3 Professor, Department of Surgery, Kasturba Medical College, Light House Hill Road, Mangalore, Karnataka, India 575001.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ranjith Rao M. Assistant Professor, Department of Surgery, Kasturba Medical College, Light House Hill Road, Mangalore, Karnataka, India 575001
Phone: 91 9845434043
E-mail: drranjithrao@gmail.com
A diaphragmatic hernia is usually seen in childhood and it is rare in adults. We are reporting a case of a 73 years old male who presented with pain and distension of the abdomen, breathlessness and constipation. He was operated 10 years back for a diaphragmatic hernia, during which a splenectomy, omentectomy and a mesh repair were done. X-rays and CT scans of the chest and the abdomen showed a recurrent diaphragmatic hernia on the left side. Laparotomy and left sided thoracotomy was done. The contents being the small bowel and the colon, they were reduced. The left hemi-diaphragm was completely absent, except for an anterior thin rim of tissue. A short ischaemic jejunal segment was resected. A dual mesh was used to reconstruct the left hemi-diaphragm in a contaminated field and it was fixed to the intact rim and to the other available tissues around the defect. The post-operative chest X-rays showed the mesh to be in place. The patient had an uneventful recovery. No signs of recurrence were found during 2 years of followup. Adult diaphragmatic hernias, once they are diagnosed, are managed surgically to prevent complications. Difficult scenarios may be encountered, for which the surgical strategy should be individualized and the immediate postoperative complications should be dealt appropriately.
Diaphragmatic hernia, Bochdalek hernia, Traumatic, Hernia repair, Diaphragm, Adult
Introduction
A diaphragmatic hernia is a condition which is commonly diagnosed and treated in the neonatal period. This condition may rarely be undiagnosed at birth and it may present with symptoms in adulthood. The adult diaphragmatic hernias are usually asymptomatic and they are diagnosed incidentally when patients are being investigated for non-specific symptoms. Most of the complications are related to visceral incarceration and hence, an early surgical management becomes mandatory. The defect in the diaphragm is approximated with interrupted sutures if it is small and it is covered with a prosthetic mesh patch if it is large sized [1].The use of a mesh in a contaminated field has a considerable risk. A complete absence or a near complete defect in a diaphragmatic hernia is a rare presentation and operating in a recurrent situation with minimal information of the previous surgery makes the surgical treatment a challenging task. The fixation of a suitable mesh in a tension free manner to the available minimal surrounding structures, creates a rare but a complex scenario. The reduction of large hernias may lead to untoward sequelae in the immediate postoperative period, which has to be borne in mind.
Case Report
We are reporting a case of 73 years old male who presented to us in the surgical emergency ward with distension of the abdomen and colicky pain of 4 days duration and breathlessness and constipation of 3 days duration. On examination, he was found to have tachypnoea, normal haemodynamics and distension of the abdomen. There were no signs of peritonitis. The bowel sounds were sluggish. The left hemithorax was not expanding as compared to the right one and the breath sounds were diminished on the left side. He had an oblique scar on the left side of the chest, extending to the back whcih was healed with a primary intention.
He was operated elsewhere for a left sided diaphragmatic hernia, 10 years back, during which a splenectomy, omentectomy and a mesh repair of the defect were performed, which had ended in a normal recovery. No clinical or investigation details were available. There was no past history of any significant trauma or a road traffic accident.
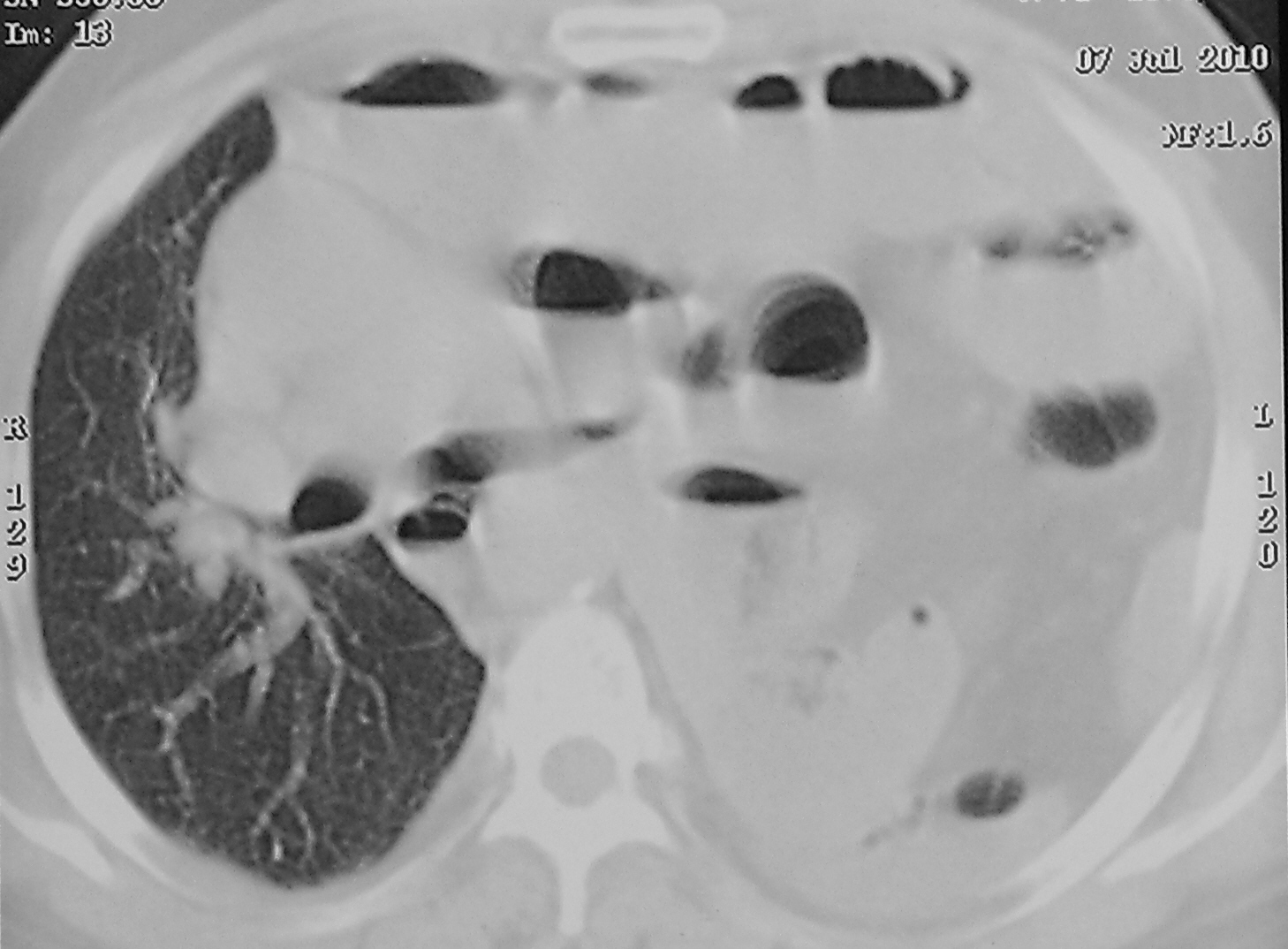
He was investigated with blood examinations and chest and abdomen X-rays, which showed bowel loops in the left hemithorax, with a visible defect in the left hemi-diaphragm [Table/Fig-1]. The abdomen showed features of small bowel obstruction. The CT scans of the chest and abdomen confirmed the diagnosis of a recurrent diaphragmatic hernia on the left side [Table/Fig-2]. A laparotomy with left sided thoracotomy was done and the hernia was explored by using a double-lumen endotracheal tube. The contents were the colon and the small bowel, with the latter having dense adhesions onto the pericardium, probably due to the migrated mesh which was used during the previous surgery. The material which was used was unknown. No intact prosthetic material was encountered in the field. After the reduction of the contents, a 20cms length of the ischaemic jejunal segment was resected. The defect in the left hemidiaphragm was very large, with the pericardium and the descending aorta being exposed medially, a thin rim of the diaphragmatic remnant on the anterior aspect and with no tissue on the lateral and the posterior wall. A Proceed® dual mesh which measured 20 x 20cms was used to reconstruct the diaphragm in a tension-free manner. The absorbable surface of the mesh was placed towards the peritoneum and it was medially fixed to the pericardium and the peri-adventitial tissue of the descending aorta, posteriorly and laterally to the intercostal muscles of the thoracic wall and anteriorly to the intact rim of the tissue. We fixed the mesh with 2-0 prolene interrupted horizontal mattress sutures. At the end of the procedure, the mesh took a natural convexity towards the thorax. The abdomen was closed first with a tube drain and the thoracotomy was closed later by deploying an intercostal drainage tube. The patient needed an elective post-operative ventilation for 5 days. The post operative X-rays showed the mesh to be in place, with a mild collapse of the lower lobe of the left lung. The patient had an uneventful recovery and he was discharged on the 14th post operative day. There were no signs of recurrence during these 2 years of the follow-up.
Chest X-Ray showing bowel loops in the left hemithorax with gross mediastinal shift to the right

CT Scan Chest at the level of mid-thorax showing dilated bowel loops & right sided mediastinal shift displacing heart
Discussion
Diaphragmatic hernia in adults is due to a delayed presentation of the congenital type or it may occur secondary to a trauma. Bochdalek hernia is the most common congenital diaphragmatic hernia which presents in newborns with respiratory distress [1]. It occurs due to the abnormal persistence of the pleuroperitoneal canal during the 8th–12th gestational weeks. The right canal usually closes early, leading to hernias which occur more commonly on the left side. There is a male preponderance of 2:1 among the newborns. Few cases may be seen in early childhood. The incidence of the delayed presentation in adults varies from 0.17-6% [2]. Trauma, both the blunt and the penetrating type, is a common cause. Blunt trauma causes 75% of the cases. More than half of the cases occur on the left side [3].
Most of the cases are asymptomatic and they are incidentally diagnosed while the patients are being investigated for other disorders. The symptoms, if they are present, are related to the gastrointestinal tract and they rarely involve the respiratory system. In the right-sided hernias, the contents are predominantly the liver, the kidney, and fat, whereas the left-sided hernias contain the enteric tract, the spleen, the liver, the pancreas, the kidney, or fat. The colon-containing hernias are rare and they usually occur through left-sided defects, as was seen in our case. Most of the complications are related to incarcerations of the small or the large bowel. Chest X-rays with bowel contrast studies and CT scans of the chest and the abdomen are the investigations which are needed to diagnose this condition with the latter being more specific [2].
The recurrence of a diaphragmatic hernia may be due to causes like the use of absorbable sutures for the primary closure of the defect during a previous surgery [4], the tension during a primary closure, improper fixation of the prosthetic material to the defect edges with a minimal overlap, the post-operative increase in the abdomen pressure due to a prolonged ileus, poor chest toileting and an intra-abdominal sepsis which leads to tension and disruption of the tissue and the sutures, which result in the mesh displacement or re-opening of the defect. A recurrence largely occurs due to a failure at the host-prosthesis interface, while the synthetic patch integrity is usually maintained [5].
A peritoneal sac may or may not be there (its incidence varies from 10 to 38%) [2], around the contents, but if it is absent, it leads to bowel adhesion onto the intrathoracic organs, which needs a tedious dissection, making reduction through a laparotomy difficult. Thoracotomy is the preferred route in a chronic traumatic or a long standing, diaphragmatic hernia, but both sides of the diaphragm need to be approached if a visceral incarceration is suspected [6]. The size of the defect in the diaphragm may vary, but rarely is the diaphragm totally absent. Small defects are primarily closed with interrupted non-absorbable sutures by using pledgets on some occasions. A larger defect is covered with a prosthetic mesh patch repair. The size of the mesh which is used to bridge the defect varies according to the defect size. Laparoscopic and thoracoscopic approaches have been used, even in recurrent hernias [7, 8]. Flaps with the use of muscle or fascia and biomaterial patch repairs have as well been performed. Flaps and prosthetic patch repairs play an important role when recurrent cases are being treated [5].
The complete or near complete defects pose a surgical challenge, as the entire tissue has to be replaced by a prosthetic mesh. A dualmesh which has both absorbable and non-absorbable surfaces provides a good alternative in dealing with such situations. Using a prosthetic mesh in a contaminated field creates a difficult situation, but it has been used both in the open and the laparoscopic routes, with successful outcomes [9]. In this case, apart from the usual surgical complications that the diaphragmatic hernia posed, the difficult task was to fix the mesh to the structures which were in the vicinity of the defect, to provide stability for the mesh to tolerate the immediate post-operative increased abdomen pressure. An awareness on the abdominal compartment syndrome during the early postoperative period is also essential in the cases where large hernias have been reduced [10]. A good lung ventilation, either mechanical, if it is indicated or through chest physiotherapy, may provide the necessary support to prevent a respiratory compromise. The right choice of the prosthetic material or the method of repair of the defect prevents the likelihood of a recurrence. The use of a unique surgical strategy, along with an aggressive postoperative management, led to a promising result in our case. The complications which arise out of diaphragmatic hernias can cause high mortality, necessitating an early diagnosis and an emergency surgical treatment for successful outcomes. The surgical team needs to individualize its strategies while it deals with rare scenarios that may present when it treats adult recurrent diaphragmatic hernias, keeping in mind the postoperative challenges that each case may offer.
[1]. Mathew MH, David WR, Paraoesophageal and complex diaphragmatic hernias. In: Charles J. Yeo, Shackelford’s Surgery of the Alimentary Tract 2007 6thPhiladelphiaSaunders Elsevier:549-62. [Google Scholar]
[2]. Mullins ME, Stein J, Saini SS, Mueller PR, The prevalence of the incidental Bochdalek’s hernia in a large adult populationAm J Roentgenol 2001 177:363-66. [Google Scholar]
[3]. Reber PU, Schmied B, Seiler CA, Baer HU, Patel AG, Buchler MW, The missed diaphragmatic injuries and their long-term sequelaeJ Trauma 1998 44:183-88. [Google Scholar]
[4]. Kitada M, Ozawa K, Satoh K, Hayashi S, Sasajima T, A recurrent diaphragmatic hernia, 3 years after an initial repair for a traumatic diaphragmatic rupture: a case reportAnn Thorac Cardiovasc Surg. 2010 16:273-75. [Google Scholar]
[5]. Bekdash B, Singh B, Lakhoo K, Recurrent late complications following congenital diaphragmatic hernia repairs with prosthetic patches: a case seriesJ Med Case Rep. 2009 May 26 3:7237 [Google Scholar]
[6]. Gregory JJ, Diaphragmatic injuries. In: John L. Cameron. Current Surgical Therapy 2011 10thPhiladelphiaSaunders Elsevier:930-37. [Google Scholar]
[7]. Tokumoto N, Tanabe K, Yamamoto H, Suzuki T, Miyata Y, Ohdan H, The thoracoscopic-assisted repair of a Bochdalek hernia in an adult: a case reportJ Med Case Rep. 2010 Nov 17 4:366 [Google Scholar]
[8]. Frantzides CT, Madan AK, O’Leary PJ, Losurdo J, The laparoscopic repair of a recurrent chronic traumatic diaphragmatic herniaAm Surg 2003 69:160-62. [Google Scholar]
[9]. Dente M, Bagarani M, The laparoscopic dual mesh repair of a diaphragmatic hernia of Bochdalek in a symptomatic elderly patientUpdates Surg. 2010 62(2):125-28. [Google Scholar]
[10]. Losanoff JE, Sauter ER, A congenital, posterolateral, diaphragmatic hernia in an adultHernia 2004 8:83-85. [Google Scholar]