Congenital Lobar Emphysema (CLE) is one of the rare cystic malformations of the lung. This malformation is generally confused with pneumothorax of the lung and most often, the placement of an intercostal drainage tube is entertained in an emergency situation, but the non- improvement of the distress and non-expansion of the lung are eye openers for a treating paediatrician. We are describing a case of a 26 days old baby who presented with respiratory distress in the Emergency Department. On the basis of the chest X-ray (CXR), we suspected it to be a case of pneumothorax and an intercostal drainage tube was inserted. But as he did not improve, CT of the chest was done and the baby was diagnosed to have congenital lobar emphysema. In spite of the advanced diagnostic techniques, the diagnosis of CLE may present a diagnostic challenge and a high index of suspicion is needed if the diagnosis has to be made promptly.
Congenital Lobar Emphysema (CLE), Inter-costal chest Drainage (ICD), X-Ray
Introduction
Congenital lobar emphysema is a rare malformation of the lung development with an incidence of 1 in 70,000 to 1 in 90,000 live births. Most of the cases are identified during the neonatal period, but the diagnosis may be delayed for as long as 5 to 6 months in 5% of the patients [1]. The overdistension may be caused by a localized, partial obstruction [2]. A congenital deficiency of the bronchial cartilage, an external compression by the aberrant vessels [3], a congenital Cytomagalovirus infection [4], bronchial mucosal flaps and kinking have been well described.
We are presenting a case of a neonate who was initially diagnosed as pneumothorax and an ICD was put, but later on, it was proved to be a case of CLE. As this is a serious life threatening condition, a prompt diagnosis is important for making an appropriate management plan.
Case Report
A 26-days male boy presented to the Paediatrics Emergency Department with cough and respiratory distress since 2 weeks of age. He was referred to us because of the non improvement of his symptoms even after receiving intravenous antibiotics and other supportive measures. There was no history of cyanosis, seizures or fever. His antenatal period was insignificant. An antenatal ultrasonography (USG) was done at 18 weeks of gestation, which was normal. The patient was born after 5 years of a non consanguineous marriage. No risk factors for sepsis were present. The baby was exclusively breastfed.
On examination, the baby was found to be of term and appropriate for his gestational age. At the time of his admission, his heart rate, blood pressure, temperature and capillary refill time were found to be normal for his age. Spo2 was 84% on oxygen and his weight was 3.5 kg. The patient was tachypnoeic, with a respiratory rate of 76 per minute, with intercostals and a subcostal indrawing. The trachea and the apex beat were shifted to the right side with a hyper-resonant percussion note and with a decreased breath sound on the left side of his chest. The crepts were audible on the right side of the chest.
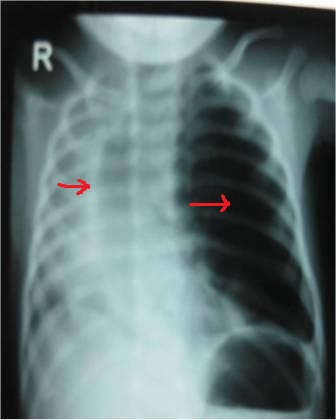
His chest X-Ray (CXR) revealed an increased hyperlucency of the left lung fields and shifting of the mediastinum to the right side [Table/Fig-1]. The blood gas analysis revealed a pH of 7.36, PO2 of 73.4 mm Hg, PCO2 of 40.2 mm Hg, SpO2 of 90.1% and HCO3 of 18.9 mmol. Echocardiography and ultrasonography of the skull were essentially normal (to rule out any other congenital anomaly).
Chest X-Ray showing increased hyperlucency of left lung fields and shifting of mediastinum to right side
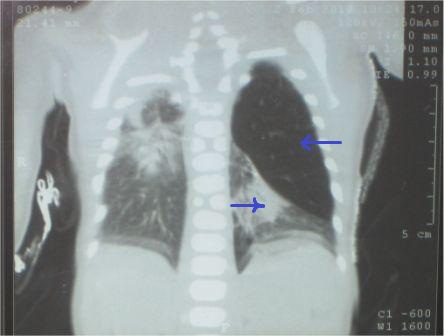
The treating paediatrician put the patient under a warmer and a humidified O2 inhalation was given. Based on the bedside CXR (as there was hyperlucency), a provisional diagnosis of pneumothorax was made and an intercostal drainage tube (ICD) was inserted, but the patient's condition did not improve. The patient remained dyspnoeic, with a SpO2 of 84%. A repeat X-ray which was done after the ICD insertion revealed non expansion of the lung and there was no release of the pneumothorax even after the ICD repositioning. On the basis of a repeat CXR and the non improvement even after the ICD insertion, the diagnosis was revised to CLE. CT of the thorax was done, which revealed a hyperinflated left upper lobe and collapse of the left lower lobe and the right lung [Table/Fig-2]. A final diagnosis of CLE of the left upper lobe was made. A surgical excision of the emphysematous lobe was performed, after which the patient recovered completely. A post operative CXR revealed expansion of the previously atelectatic lobe. A biopsy of the excised lobe revealed distension of the alveolar acini with the absence of cartilage.
CECT Chest showing hyperinflated left upper lobe and collapse of left lower lobe and right lung
Discussion
CLE is a rare malformation of the lung development which is characterized by an over inflation of a pulmonary lobe. A congenital deficiency of the bronchial cartilage and compression of the aberrant vessels have been described commonly [3]. Many a theory has been postulated but most recently, the theory of Polyalveolosis i.e an increased number of alveoli within each acinus, has been described [5]. It has been reported that this disease is more common in male children, being usually unilateral and affecting the left upper lobe more often (43%), followed by the right middle lobe (32%), although a bilateral involvement is not unknown [6]. The affected lobe is essentially non-functional because of overdistention and air trapping. Furthermore, there is compression atelectasis of the ipsilateral normal lung, which leads to a respir- atory compromise. With further distension, the mediastinum is shifted to the contralateral side, resulting in a bilateral, impaired lung function. A radiolucent lobe and a mediastinal shift are often revealed by a radiograghic examination [1]. This condition is generally confused with pneumothorax of the lung and most often, the placement of an intercostals chest tube is entertained in an emergency situation. But non-improvement of the distress and non expansion of the lung are eye openers for a treating paediatrician.
A series of 3 cases which presented with respiratory distress were mistakenly diagnosed as pneumothorax and an ICD was inserted in all the 3 cases, but later on, all turned out to be CLE [7]. As in our case, the ICD insertion does not help; rather, it may further increase the respiratory distress. In another series of 10 cases of CLE, a correct diagnosis was made only in 4 out of the 10 cases on chest radiograph before referral, even though the diagnosis could be arrived at in all the 10 cases on the basis of the initial radiographs [8].
The basic investigation in congenital lobar emphysema is a chest radiograph, from which a diagnosis can be made and it is readily accessible. A careful examination of the X-ray film with transillumination shows the presence of bronchovascular markings in CLE, whereas these markings are absent in the cases of pneumothorax [5]. The effects of the secondary compression of the over expanded lobe such as a tracheal or a mediastinal shift away from the affected lobe, atelectasis of the adjacent lobes or herniation of the expanded lobe across the midlines, are the other pointers [9]. Moreover, the pleural lines are visible in pneumothorax and not in CLE. However, the initial CXR may not show this “typical appearance”. The child may present with a region of increased density on the CXR rather than a hyperlucency and it can be misdiagnosed as pneumonia. This atypical presentation has been reported earlier [10,11,12]. But if the secondary compressive signs are present, a diagnosis of CLE should be considered.
Other diagnostic maneouvers for CLE which have been utilized, include CT scan, bronchography, bronchoscpy, angiography, magnetic resonance imaging, scintigraphy and even exploratory thoracotomy.
CT scan is an important diagnostic procedure because it not only shows the abnormally narrowed bronchus, the hyperinflated left upper lobe and the collapsed lower lobe, but it also shows that although the right lung is compressed, it consists of 3 lobes, thereby excluding a hypoplastic right lung as the cause of the appearances. The CT scan also exclude a vascular abnormality and other conditions that might be confused with CLE, such as pneumothorax, pneumatocoele, a diaphragmatic hernia or a cystic adenomatoid malformation [13].
V/Q scintigraphy is helpful in differentiating CLE from a foreign body and a compensatory hyperinflation which is secondary to atelectasis of other regions of the lung, but it is not available even at most of the advanced centres [11]. Bronchoscopy may be of value in ruling out the presence of an intraluminal foreign body that causes obstructive emphysema or atelectasis with compensatory emphysema [11]. But these procedures are not available in most of the hospitals in the developing countries.
Conclusion
In spite of the development of advanced diagnostic techniques, CLE is still a diagnostic dilemma for paediatrician. So, a high index of suspicion is needed to diagnose CLE in neonates who present with a progressive respiratory distress. A differential diagnosis of CLE should always be considered before inserting an ICD in a suspected case of pneumothorax, especially in a neonate.
[1]. Boas S, Winnie GB, Emphysema and Overinflation. In:Kliegman RM, Behrman RE, Jenson HB, Stanton BF. Nelson textbook of pediatrics 18th edition Elsevier publishers 2007 :1779-80. [Google Scholar]
[2]. Doull IJ, Connett GJ, Wamer JO, Bronchoscopic appearances of congenital lobar emphysemaPediatric Pulmonology 1996 21(3):195-97. [Google Scholar]
[3]. Absher DR, Kriss VM, Cotrill CM, Lobar emphysema due to anomalous aortic origin of the left pulmonary arteryCardiol-Young. 1999 9(3):327-30. [Google Scholar]
[4]. Carrol ED, Campbell ME, Shaw BN, Pilling DW, Congenital lobar emphysema in congenital cytomegalovirus infectionPediatr-Radiol. 1996 89(12):900-02. [Google Scholar]
[5]. Guidici R, Leao LE, Moura LA, Wey SB, Ferreira RG, Crotti PL, Polyalveolosis: pathogenesis of congenital lobar emphysema?Rev Assoc Med Bras 1998 44:99-105. [Google Scholar]
[6]. Ozcelik U, Gocmen A, Kiper N, Dogru D, Dilber E, Yalcin EG, Congenital lobar emphysema: evaluation and long-term follow-up of thirty cases at a single centerPediatr Pulmonol 2003 35(5):384-91. [Google Scholar]
[7]. Tempe DK, Virmani S, Javetkar S, Banarjee A, Puri SK, Datt V, congenital lobar emphysema: pitfalls and managementAnnals of Cardiac Anesthesia 2010 13:53-58. [Google Scholar]
[8]. Bappal B, Ghani SA, Chaudhary R, Sajvani MJ, Congenital lobar emphysema: a review of 10 casesIndian-J-Pediatr. 1996 63(6):801-08. [Google Scholar]
[9]. Caffey J, Congenital lobar emphysema. In: Caffey J.Pediatric X-ray Diagnosis. 6th ed. Chicago: Year Book Medical Publishers 1972 :1464 [Google Scholar]
[10]. Franken EA, Buehl I, Infantile lobar emphysema: report of two cases with unusual roentgenographic manifestationsAm J Roentgenol 1966 98:354-57. [Google Scholar]
[11]. Loewy L, O'brodowich H, Coates G, Ventilation scintigraphy with submicrinic radioaersol as adjunct in the diagnosis of congenital lobar emphysemaJ Nucl Med 1987 28:1213-17. [Google Scholar]
[12]. Fagan CJ, Swischuk LE, The opaque lung in lobar emphysemaAm J Roentgenol 1972 114:300-04. [Google Scholar]
[13]. Joazlina ZY, Wastie ML, Bruyne JAD, Congenital lobar emphysema: a diagnostic challengeJHK Coll radiology 2005 8:105-08. [Google Scholar]