Blue Rubber-Bleb Nevus Syndrome which was Associated with an Atrial Septal Defect: A Case Report
Shrikiran Aroor1, Chaitanya Varma2, Suneel C Mundkur3
1 Professor, Department of Paediatrics.
2 Assistant Professor, Department of Paediatrics.
3 Additional Professor, Department of Paediatrics, Kasturba Medical College, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Chaitanya Varma Assistant Professor, Department of Paediatrics, KMC Manipal, Karnataka, India.
Phone: 9964143170
E-mail: pvc_varma@yahoo.com
The Blue Rubber Bleb Nevus Syndrome (BRBNS) is a rare cause of persisting gastrointestinal bleeding. We are presenting a case which was associated with an atrial septal defect.
Blue rubber bleb nevus syndrome, Bean syndrome, Bleeding, Hemangiomas
Introduction
The Blue Rubber Bleb Nevus Syndrome (BRBNS) is a rare disease which is characterized by skin lesions and intestinal venous malformations that lead to gastrointestinal bleeding and chronic anaemia. The characteristic cutaneous lesions consist of deep-blue, easily compressible, soft, rubbery blebs. Most of the cases are sporadic, but a dominant autosomal transmission has also been reported. Very few Indian cases have been described in the literature. We are presenting the case of a 7 year old boy with BRBNS with an associated Atrial Septal Defect (ASD).
Case Report
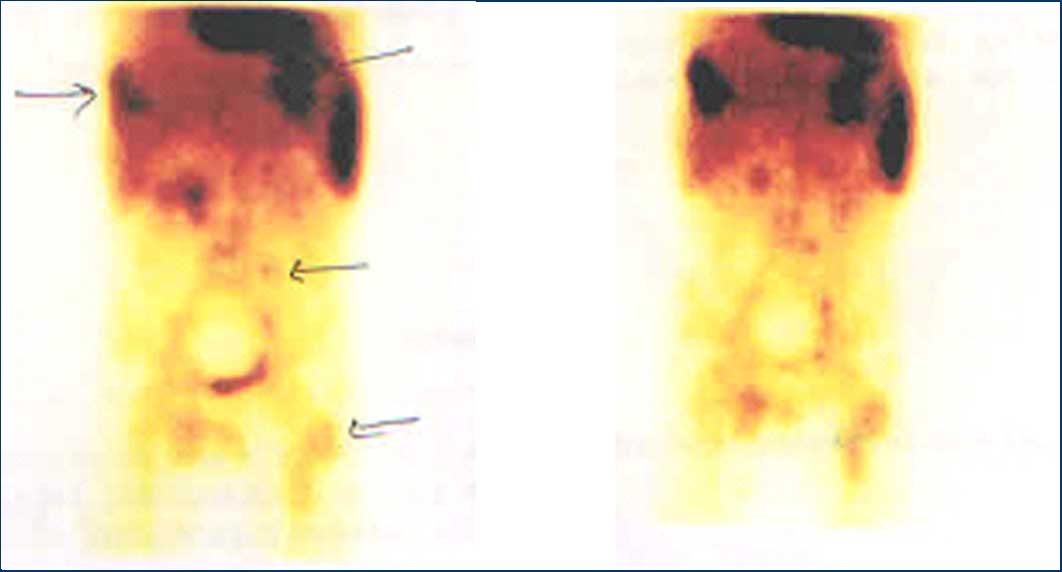
A 7 year old male child who was born out of a non consanguineous marriage, presented with a history of facial pallor, tiredness, easy fatiguability, breathlessness on exertion and passing fresh blood in stools. The child had a height of 116cms and a weight of 16kgs, which were both below the 3rd centile for age and sex. His examination revealed severe pallor, hepatomegaly, a shifted apex in the 6th intercoastal space in the anterior axillary line, visible epigastric and suprasternal pulsations with a loud first heart sound, a widely split second heart sound and a grade 4/6 ejection systolic murmur, which suggested an Atrial Septal Defect (ASD) and congestive cardiac failure. Multiple blue coloured hemangiomas were present over the jaw, chest wall, back, fingers and toes, which were easily compressible [Table/Fig-1]. The lab investigations showed a haemoglobin level of 1.4gm/dl and a peripheral smear with the features of severe iron deficiency anaemia. Echocardiography revealed a 10mm sinus venous ASD. Ultrasonography of the abdomen revealed multiple hemangiomas with a slow venous flow along the anterior chest wall. Scintigraphy studies showed the pooling of the tracer over the thoracic wall, the left thigh, the left mandible and the right lower limb. An abnormal tracer concentration was also seen near the bifurcation of the abdominal aorta and the small intestine [Table/Fig-2]. Computer tomography revealed multiple diffuse hemangiomas in the small bowel wall. The child was started on antifailure measures and he was transfused with packed cells. The child underwent an ASD surgical correction 3 months later. He was admitted twice over a period of the next six months for similar complaints and was transfused with packed red cells. Paediatric surgeons ruled out embolization or resection of the bowel wall because of the diffuse spread of the hemangiomas. The boy was started on propranolol as an antiangiogenic measure. The child has been asymptomatic and under regular follow up for the past 6 months.
Haemangiomas on the fingers, great toe and chest wall

Scitigraphy images showing tracer concentration
Discussion
William Bennet Bean first described BRBNS with cutaneous and gastrointestinal malformations in 1958 and hence it is also called as the 'Bean syndrome'[1]. The incidence of this syndrome is very low and only around 200 cases have been described in the medical literature. Bean described three types of cutaneous lesions: (1) blue, rubbery, blood-filled sacs with a smooth or wrinkled surface, that are easily compressible and promptly refilled when the pressure is released; (2) large, disfiguring, cavernous lesions that may compress the vital structures; and (3) blue irregular macules. They are discrete, multifocal and are mainly present over the trunk, soles and the palms, but they may be seen anywhere in the skin. The skin lesions rarely bleed, unlike the gastrointestinal lesions which can be present anywhere from the oral cavity to the anus and they usually exhibit bleeding at an early age, that continues throughout their life. A massive sudden haemorrhage rarely occurs, but the patients are chronically anaemic. Abdominal pain, intussusception, volvulus, infarction or internal haemorrhages are also present [2]. Mafucci's syndrome and the Rendu-Osler-Weber syndrome are other conditions where the skin lesions are associated with Gastrointestinal (GI) bleeding.
The characteristic skin lesions and a stool guaiac test which is done to detect anaemia and gastrointestinal bleeding, help in the initial evaluation of BRBNS. The bleeding sites may be evaluated with barium studies, angiography, tomography, magnetic resonance imaging and endoscopy [3]. Endoscopy and skin biopsy could not be done because the parents were unwilling for invasive procedures.
The reports on cardiac defects being associated with BRBNS are very few. Zhong et al. reported a Ventricular Septal Defect (VSD) and a raised pulmonary pressure in a child with BRBNS [4]. An extensive literature search did not reveal any association of ASD with this syndrome and this could well be the first case with such an association, which has been reported.
A conservative management with iron supplementation and blood transfusion is the first line of management of the gastrointestinal bleeding. Anti-angiogenic treatments and endoscopic sclerotherapy and coagulation have been reported as the non surgical interventions [2,5]. Surgical resection of the lesions is rarely successful due to the extensive and diffuse nature of the lesions in the GI tract. Laser therapy is usually used for cosmetic reasons to remove the cutaneous lesions [6].
Conclusion
BRBNS is a rare condition which is characterized by venous malformations in the skin and the GI tract. We are presenting such a case with an association with ASD. The treating physician should rule out gastrointestinal and intracranial malformations when this syndrome is suspected. The patient should be counselled about the chronicity of this condition, the necessity of symptomatic and conservative treatment and the need for regular follow-up.
[1]. Bean WB, Blue rubber bleb nevi of the skin and the gastrointestinal tract. In:Vascular Spiders and Related Lesions of the Skin. Springfield, IL: Charles C. Thomas 1958 :178-85. [Google Scholar]
[2]. Dobru D, Seuchea N, Dorin M, Blue rubber bleb nevus syndrome: a case report and literature reviewRom J Gastroenterol. 2004 Sep 13(3):237-40. [Google Scholar]
[3]. Ping QZ, Fang XZ, Qi HX, Jian LX, Blue rubber bleb nevus syndrome with maxillofacial hemangiomasJournal of Oral and Maxillofacial Surgery 2001 (4):351-55. [Google Scholar]
[4]. Kassarjian A, Fishman SJ, Fox VL, Burrows PE, Imaging characteristics in the blue rubber bleb nevus syndromeAJR Am J Roentgenol 2003 181:1041-48. [Google Scholar]
[5]. Rodrigues D, Bourroul ML, Ferrer AP, Monteiro Neto H, Gonçalves ME, Cardoso SR, The blue rubber bleb nevus syndromeRev Hosp Clin Fac Med Sao Paulo 2000 55:29-34. [Google Scholar]
[6]. Suma GN, Ravi Prakash SM, Rao D, Goel S, Blue rubber bleb nevus syndrome: Prominent oral findingsIndian J Dermatol Venereol Leprol 2010 76:168-71. [Google Scholar]