A Malignant Transformation in a Pre-Existing Benign Scrotal Naevus
Ranjan Agrawal1, Mukta Kumar2
1 Associate Professor, Department of Pathology, Rohilkhand Medical College Hospital, Bareilly, India.
2Department of Pathology, Rohilkhand Medical College Hospital, Bareilly, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ranjan Agrawal Associate Professor, Department of Pathology Rohilkhand Medical College Hospital Pilibhit Bypass Road, Bareilly - 243006 (India).
Phone: 9412291009;
E-mail: drranjan68@gmail.com
Malignant melanoma of the scrotum is the rarest of the primary genitourinary melanomas, with only 19 cases having been reported previously. The authors have described a rare case of a primary scrotal neoplasm. The necessity of a prompt diagnosis has been emphasized. We are presenting an additional case of this often aggressive malignancy. The pertinent literature has been reviewed and the current management strategies have been discussed.
Primary ovarian pregnancy
Introduction
Both the benign and the malignant tumours of the scrotum are rare. The scrotal malignancies are of special importance not only due to their historical importance, but also since they are rare in incidence. Malignant melanoma of the scrotum is the rarest of the primary genito-urinary melanomas [1-3]. A case of a primary malignant melanoma of the scrotum with an unusual presentation has been described.
Case Report
A 45-years old Hindu male presented to the surgical outdoor clinic with a lump in the right scrotum. He mentioned that it had started as a small black mole, 30 years back. Now recently, there had been an increase in its size, with an ulceration on its surface, with its colour becoming bluish-black. At times, he experienced a mild stretching pain. A tender swelling had developed in his right groin as well. His chest X-ray and ultrasound of his abdomen were insignificant. A wide excision of the mass with right inguinal lymphadenectomy was carried out.
Grossly, the specimen was globular and blackish in colour, with a stalk attached at one end. It measured 5 x 4 x 1.5cm in dimension. The outer surface was irregular and it was ulcerated at one place. The cut-surface was variegated, with multiple areas of haemorrhage. Two lymph nodes were dissected out in the inguinal tissue; the cut-surface of both showed extensive areas of necrosis.
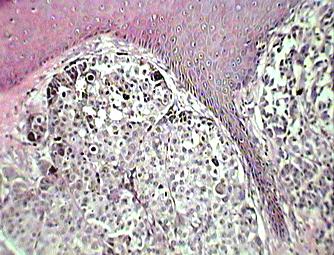
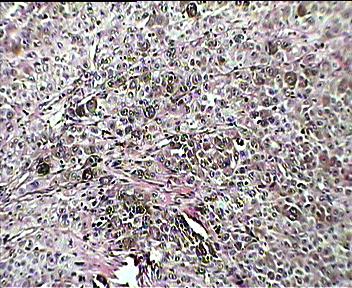
Microscopic sections from the pedunculated growth showed a stratified squamous epithelium with rete pegs and an outer thickened keratin layer. At one place, the epidermis was ulcerated. Beneath the epidermis, nests and sheets of neoplastic cells were present. The individual cells were medium to large sized with a high nuclear: cytoplasmic ratio. The cytoplasm was moderate in amount. Most of the cells showed a dark brown to black pigment in the cytoplasm [Table/Fig-1]. At places, a pigment incontinence was noted. Areas of necrosis and haemorrhage were present. The sections from both the lymph nodes showed replacement of the lymphoid tissue with nests of similar neoplastic cells, with pigmentation [Table/Fig-2]. The tumour cells stained positive for S100. A diagnosis of malignant melanoma of the scrotum with metastasis to the right inguinal lymph nodes was made.
Nests of melanoma cells with pigment incontinence (H&E x40)
Inguinal lymph node showing almost complete replacement by melanoma cells (H&E x 40)
According to the clinicopathologic staging system of the American Joint Committee on Cancer (AJCC), the tumour belonged to Stage III i.e with lymph node involvement and as per the level of invasion, it was of the AJCC level V, with invasion of the subcutaneous fat. A metastatic evaluation with a CT scan and a bone scan did not reveal any pulmonary, hepatic or osseous foci. The patient was reported to have expired one month after being discharged from the hospital.
Discussion
A malignancy of the scrotum is of special interest, despite its relative infrequency, because of its surprising virulence and also by virtue of its historical importance. This was the first known occupational cancer and it showed the need for research by involving the potential environmental carcinogens. Primary malignant melanoma of the scrotum is among the rarest of the lesions. Between 1949 and 2009, only 19 cases had been reported in the world literature [3,4]. However, none of the previous reports had mentioned such a history of a malignant transformation in a previously existing benign lesion. The present case was interesting, since the lesion (probably a Naevus) was present since the past 30 years and as it was neglected. This lesion was later followed by a sudden increase in its size, colour and texture, along with pain. These features are known to accompany a transformation from a benign to a malignant stage.
Due to the paucity of cases, there is lack of information about the natural history, aetiology and the standard management of scrotal melanomas. Fair skinned persons are more prone to develop malignant melanomas. A large majority of melanomas are associated with sunlight exposure and hence they are more common in the head and neck region and the lower extremities. They especially affect the females. This major risk factor for the development of malignant melanoma did not apply to our patient since the affected site was not sun-exposed. The commonest presentation of melanoma of the scrotum which had been reported earlier was a pigmented macule or a papule [5]. At times, the lesion presents as a pigmented exophytic mass with ulceration, satellite lesions and palpable inguinal lymphadenopathy, as was seen in our patient [6-7].
The histologic diagnosis and the tumour staging of primary scrotal melanoma is done in a manner which is similar to those of other primary cutaneous and epithelial melanomas. Some authors suggest that primary scrotal melanoma may have a more favourable prognosis than the other genitourinary malignancies [5]. We feel that this may be true for those tumours which present as small pigmented macules or papules, but those which present as large, exophytic, ulcerative masses have a poor prognosis, as in our patient, who died from the disease within 1 month of the diagnosis [7-8].
The prognosis of melanoma in general depends on – the clinical features, the spread to the regional lymph nodes and the distant metastasis; the anatomical location and the histological features. The melanomas on the extremities have been reported to have a better prognosis. Histologically, the prognosis depends on the Breslow's vertical thickness and the Clark's anatomical level of local invasion, the presence or absence of an ulceration, the satellite lesions, the margins, the mitotic index and the Tumour-Infiltrating Lymphocytes (TIL), regression, the angiolymphatic invasion and neurotropism. In a recent study, the presence of brisk TIL in a lymph node metastasis was found to be associated with a higher survival rate than in the patients whose metastasis lacked TIL [9].
Since, only few cases of melanoma of the scrotum have been reported so far, the exact treatment modality of this entity has not been well-defined. A radical surgery can be carried out but it has its own limitations, in that, by the time the disease is diagnosed, it would have already spread further. The genetic profiling of melanomas has revealed that KIT gene mutations are present in some cases, particularly in the tumours which arise in the mucosal and the acral sites. Imatinib, which is used to treat various neoplasms which are regulated by kinase mutations, has recently been reported to be effective in cases of KIT-mutant metastatic melanomas. A previous study had recommended the screening for the KIT gene mutations in primary scrotal and genitourinary melanomas since the presence of this mutation may open up new options for the therapy [8].
[1]. In: Ackerman's Surgical Pathology: 8th ed, Juan Rosai eds. 1996 USAMosby-Year Book, Inc:150-64. [Google Scholar]
[2]. Davis NS, Kim CA, Dever DP, Primary malignant melanoma of the scrotum: a case report and literature reviewJ Urol 1991 145(5):1056-57. [Google Scholar]
[3]. Berkmen F, Tandogdu R, Ardjcoglu A, Primary scrotal malignant melanoma. A report of 2 cases and review of the literatureJ Exp Clin Cancer Res 1998 17(1):91-93. [Google Scholar]
[4]. Konstadoulakis MM, Ricaniadis N, Karakousis CP, Malignant melanoma of the scrotum: a report of 2 casesJ Urol 1994 15(1):161-62. [Google Scholar]
[5]. Sánchez-Ortiz R, Huang SF, Tamboli P, Prieto VG, Hester G, Pettaway CA, Melanomas of the penis, scrotum and the male urethra: a 40-year single institution experienceJ Urol 2005 173:1958-65. [Google Scholar]
[6]. Vasudeva P, Agrawal D, Goel A, Malignant melanoma of the scrotumUrology 2008 71(6):1053-54. [Google Scholar]
[7]. Damala K, Tsanou E, Pappa L, A rare case of primary malignant melanoma of the scrotum which was diagnosed by fine-needle aspirationDiagn Cytopathol 2004 31(6):413-16. [Google Scholar]
[8]. Beadling C, Jacobson-Dunlop E, Hodi FS, The KIT gene mutations and the copy number in the melanoma subtypesClin Cancer Res 2008 14(21):6821-28. [Google Scholar]
[9]. In: Lever's Histopathology of skin. 8th ed, David Elder eds,199Lippincott-Raven Publishers:654-78. [Google Scholar]