Hepatic mesenchymal hamartoma (HMH) is a hamartomatous growth of the mesenchymal tissue in the liver, which is of an uncertain aetiology. It is a space-occupying lesion that can potentially compress the adjacent organs, resulting in various complications, which include death. Hepatic mesenchymal hamartoma is characterized by the variable proliferation of the myxomatous mesenchyme and the malformed bile ducts. The differential diagnosis includes other paediatric hepatic masses. The diagnosis is typically made during infancy, and a complete resection is invariably curative. Here, we are reporting a case of HMH in a one year old female child who presented with abdominal distension. A clinical diagnosis of malignancy was made, based on the symptoms and imaging studies and a final diagnosis was made only after a histopathological examination. The lesion was potentially benign, with very rare chances of recurrence. This case has been presented due to its rarity.
Introduction
Hepatic mesenchymal hamartoma (HMH) is a rare congenital developmental lesion of the liver, which is of an uncertain histogenesis. It makes up approximately 8% of all the paediatric tumours and is second in occurrence only to hepatoblastoma, when only the paediatric hepatic tumours are considered. Eighty percent are found within the first 2 years of life and the remainder are detected by 5 years of age [1,2].
Rare cases have been reported in adults [3]. The differential diagnosis includes other paediatric hepatic masses. The diagnosis is typically made during infancy, and a complete resection is invariably curative.
The pathogenesis of HMH is still being debated. A handful of series have shown an association with mesenchymal stem villous hyperplasia of the placenta. Mesenchymal stem villous hyperplasia is characterized by diffuse oedema of the stem villi, with the preservation of the terminal villi. Whether these two entities are somehow related, is still in question, but the hypothesis that they arise from a synchronous abnormal mesodermal development rather than a true developmental abnormality (as originally thought), is gaining acceptance.
Case report
A 1-year-old female child presented with abdominal distension and respiratory distress of 2 week's duration. There was no history of cough, cyanosis or jaundice. The past history was uneventful. On examination, the liver was found to be palpable by 6 cm below the right subcoastal margin in the mid-clavicular line and by 3 cm in the epigastric region. It was nontender, with a smooth surface and a firm consistency and rounded borders. No other mass was palpable. The rest of the systemic examination was normal. The haemoglobin was 7.5 g/dl and the total leukocyte count was 33,000 per cu mm, with 84% polymorphs in the differential count. The bleeding time, clotting time and the platelet count were normal. Serum bilirubin was 0.7 mg/dl, SGPT was 88 IU/L (normal 0-40 IU/L) and serum alkaline phosphatase was 486.1 IU/L (normal 200-770 IU/L. The ultrasound examination showed an enlarged liver with a rounded solid mass, which had a cystic component in the right lobe of the liver, which compressed the kidney. There was no cyst in the kidneys or in any other organ. The movements of the right dome of the diaphragm were markedly restricted. The child was referred for a CT scan. The CT scan showed a 10x9 cms large, complex, predominantly solid mass with cystic areas and internal septations in the right lobe of the liver. A clinical diagnosis of malignancy was made and the tumour was resected with partial angioembolisation. The resected specimen was sent for a histopathological examination.
The resected gross specimen measured 10x9x9cms and it included a portion of the liver and the tumour. The cut section of the mass appeared multinodular grey white, with fibrous and cystic areas. The largest cyst measured 1.5cms and it was filled with mucoid material [Table/Fig-1].
Gross of hepatic Mesenchymal hamartoma showing predominant solid pattern with focal cystic areas (arrow head)

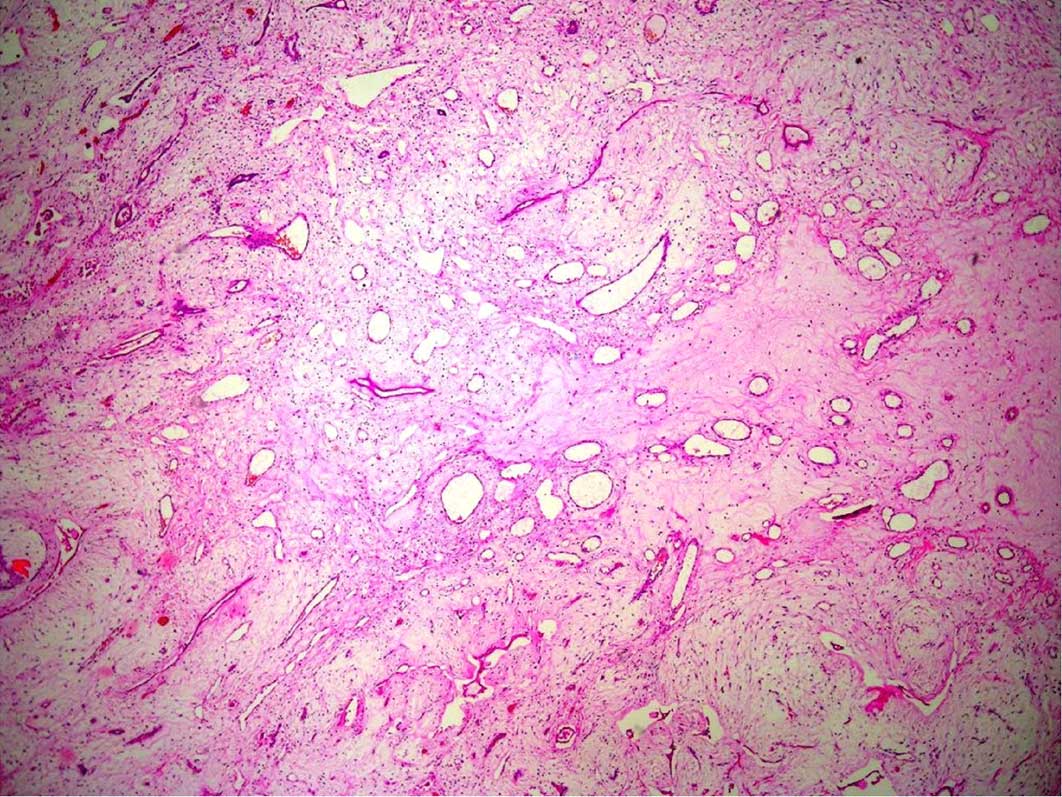
The histological examination showed proliferation of the myxomatous connective tissue which was composed of loose mesenchymal stellate cells with interspersed cystic spaces, some of which were lined by the bile duct epithelium. Branching bile ducts, which were similar to the malformed ductal plates were seen. The solid part of the tumour also showed an admixture of fibrous tissue and islands of bland hepatocytes [Table/Fig-2]. A pathological diagnosis of a mesenchymal hamartoma was made.
Photomicrography shows lobules of Mesenchymal tissue (arrow head) with adjacent cords of benign hepatocytes ( double arrow head (H & E stain, 40X)
Discussion
Less than two hundered cases have been reported in the literature [1]. This clinical entity was first described in 1959 and as a pathological lesion, it was first described in 1966 [2,3]. The other synonyms include lymphangiomas, bile duct hamartomas, mesenchymomas, psuedocystic mesenchymal tumours and cystic hamartomas. 75% of the cases of HMH involve the right lobe of the liver and the rest involve either the left lobe or both the lobes. In the current concept, HMH is viewed as a congenital process for which the histogenesis has not been well understood. Whether it represents a developmental anomaly, a reaction to a biliary obstruction, or even the result of a regional ischaemic process rather than a true neoplasm, has become a topic which is under discussion [4–6]. Nevertheless, several investigators have reported a balanced translocation between the long arms of chromosome 11 and chromosome 19. A breakpoint at chromosome 19q13.4, that had a documented karyotypic abnormality, has also been demonstrated. By using histologic, immunohistochemical, flow cytometric, and cytogenetic data, a case of embryonal sarcoma which arose from an Hepatic Mesenchymal Hamartoma (HMH), where the transformed component had the 19q13.4 breakpoint in addition to several other numerical and structural chromosomal abnormalities, was documented by some authors. Taking this together raises the possibility that perhaps a subset of the HMHs is truly neoplastic.
Mesenchymal hamartoma of the liver is a primary benign tumour that occurs exclusively during infancy and childhood, although a few cases have been reported in the older age groups [7]. Its origin is mostly from the right lobe of the liver [2]. Most of the cases remain asymptomatic, while the others are detected incidentally when they present with a right upper quadrant mass, respiratory distress, fever and a raised right hemidiaphragm [2,8]. This was the clinical scenario in the case which has been presented here. The liver function tests usually remain within normal limits, as they were in our case. The most helpful diagnostic tests are ultrasono-graphy and computerized tomography [4]. On CT scan, it presents as a complex mass which contains areas of low attenuation which are separated by solid septae and stroma, which get enhanced with intravenous contrast administration. However in our case , it was a predominantly solid lesion with cystic areas. A clinical diagnosis of malignancy was made.
Several tumours enter into the differential diagnoses of paediatric hepatic masses. The benign liver tumours in children may be divided into two major groups which may be neoplastic or non neoplastic in nature. The non neoplastic and the neoplastic lesions of epithelial derivation include simple cysts, polycystic liver disease, focal nodular hyperplasias, adenomas and hepatoblastomas [9,10]. Among the different histologic patterns of hepatoblastoma, mixed epithelial-mesenchymal hepatoblastoma is the one which is the most similar to HMH. This particular type of hepatoblastoma can be composed of relatively bland appearing hepatocytes (of the foetal type) with spindle/stellate mesenchyme. Using immunohistochemical stains alone for this differential diagnosis can potentially be misleading, because the foetal-type epithelial cells stain similar to the adult type hepatocytes (positive for cytokeratin [CK8, CK18] and hepatocyte [Hep Par 1]). In addition, the mesenchymal components of both HMH and hepatoblastoma are strongly positive for vimentin [1]. The benign mesenchymal tumours of liver are more common than their epithelial counterparts [2]. The vascular lesions of mesenchymal origin are infantile hemangioendothelioma and cavernous hemangioma. Microscopically, these tumours are quite vascular and they consist of variable sized vascular spaces which are lined by relatively immature, plump endothelial cells. The plump endothelium is positive for the factor VIII-related antigen, CD31, and for the CD34 immunohistochemical stains.
The heterotopic liver tissue may be classified either a accessory liver, when it is connected with a thin stalk to the main liver or as a true ectopic liver, when no such relationship can be established. Most often, ectopic livers are found on the serosal surface of the gallbladder. In general, the reported sizes of the ectopic livers range from a few millimeters up to several centimetres [11,12]. The mesenchymal and epithelial hamartomas have been reported to arise from ectopic liver tissues . Hepatoblastomas and hepatocellular carcinomas enter into the clinical and the radiological differential diagnoses.
Thus, a rapidly enlarging lesion with a predominant solid component can resemble the malignant abdominal lesions of infancy. In the present case, due to the large size, the rapidly growing tumour and the predominant solid appearance on CT scan and preoperatively, a clinical diagnosis of a liver malignancy was suggested and the resected tumour, along with a part of the normal liver, was sent for a histopathological examination. The final diagnosis of hepatic mesenchymal hamartoma was made only after a histopathological examination.
Pachydermoperiostosis is a rare familial genodermatosis, can present variably with features such as digital clubbing, swelling of the peri-articular tissue, osteoarthropathy, arthralgia and arthritis, congenital heart disease, a delayed closure of the fontanels, pachydermia and seborrhoea [12]. An association of this condition with an ectopic liver and hepatocellular carcinoma has been described [13].
In conclusion, mesenchymal hamartoma is considered to be a rare, benign, congenital paediatric tumour, the aetiology of which has yet to be completely elucidated. Due to its diverse clinical presentation, it can mimic a variety of benign and malignant neoplasms. Thus, a histopathological examination is mandatory, to differentiate this relatively benign condition from its clinical malignant mimics, and to avoid the unnecessary surgical and chemo-radiotherapeutic procedures which are associated with misdiagnosed malignant tumours.
[1]. Yen JB, Kong MS, Lin JN, Hepatic mesenchymal hamartomaJ Paediatr Child Health 2003 39:632-4. [Google Scholar]
[2]. Wada M, Ohashi E, Jin H, Mesenchymal hamartoma of the liver: the report of an adult case and review of the literatureIntern Med 1992 31:1370-5. [Google Scholar]
[3]. Jaswal TS, Singh S, Purwar P, Mesenchymal hamartoma of the liverIndian J Pathol Microbiol 2003 46:226-8. [Google Scholar]
[4]. Smith SL, Ramli NM, Somers JM, Cystic mesenchymal hamartoma which mimicked the hydatid diseaseClin Radiol 2001 56:599-601. [Google Scholar]
[5]. Papastrias G, Margaris H, Zografos GN, Korkolis D, Mesenchymal hamartoma of the liver in an adult: a review of the literatureInt J Clin Pract 2000 54:552-5. [Google Scholar]
[6]. Edmonson HA, Tumor of the liver and the intrahepatic ducts. Fascicle 25Armed Forces Institute of Pathology 1958 Washington, DC [Google Scholar]
[7]. Tsao KJ, Hirose S, Sydorak R, Fetal therapy for giant hepatic cystsJ Pediatr Surg 2002 E3:37 [Google Scholar]
[8]. Laberge J-M, Patenaude Y, Desilets V, A large hepatic mesenchymal hamartoma which led to a midtrimester fetal demiseFetal Diagn Ther 2005 20:141-5. [Google Scholar]
[9]. Carta M, Maresi E, Giuffre M, Congenital hepatic mesenchymal hamartoma which was associated with mesenchymal stem villous hyperplasia of the placenta: a case reportJ Pediatr Surg 2005 E37(9):40 [Google Scholar]
[10]. Kitano Y, Ruchelli E, Weiner S, Adzick NS, Hepatic mesenchymal hamartoma which was associated with mesenchymal stem villous hyperplasia of the placentaFetal Diagn Ther 2000 15:134-8. [Google Scholar]
[11]. Rakheja D, Margraf LR, Tomlinson GE, Schneider NR, Hepatic mesenchymal hamartoma with a translocation which involves the chromosome band 19q13.4: a recurrent abnormalityCancer Genet Cytogenet 2004 153:60-3. [Google Scholar]
[12]. Uppal S, Diggle CP, Carr IM, Mutations in 15-hydroxyprostaglandin dehydrogenase can cause primary hypertrophic osteoarthropathyNat Genet 2008 40:789-93. [Google Scholar]
[13]. Matthias D, Peter I, Peter M, Giant ectopic liver, hepatocellular carcinoma and pachydermia-a rare genetic syndrome?Diagnostic Pathology 2011 6(10):75 [Google Scholar]