The Immune Reconstitution Inflammatory Syndrome (IRIS) is an exaggerated pathological inflammatory reaction which occurs after the initiation of the antiretroviral therapy, due to the exuberant immune responses to the occult or the apparent opportunistic infections. The hallmark of the syndrome is the paradoxical worsening of an existing infection or a disease process or the appearance of a new infection or a disease process soon after the initiation of the antiretroviral therapy.
The most common forms of IRIS occur in association with tuberculosis and chronic viral and invasive fungal infections. Multiple IRIS in a patient is extremely rare. Our patient had multiple manifestations of IRIS, in the form of cryptococcal meningitis, toxoplasmosis and Cytomegalovirus (CMV) retinitis after the initiation of highly active antiretroviral therapy.
Immune reconstitution inflammatory syndrome (IRIS), HIV, Cryptococcal Meningitis, Toxoplasmosis, Cytomegalovirus (CMV) retinitis
Introduction
HIV-infected patients improve after starting Anti Retroviral Therapy (ART), because ART will reduce the HIV-RNA levels and boost the immune system. In some patients, another response is seen after starting with ART. In these patients, a clinical deterioration occurs despite increased CD4 counts and decreased plasma HIV viral load. Because a clinical deterioration occurs during the immune recovery, this phenomenon has been described as Immune Restoration Disease (IRD) or the Immune Reconstitution Inflammatory Syndrome (IRIS).
IRIS is defined as the occurrence or the worsening of the clinical and/or the laboratory parameters despite a favourable outcome in the Human Immunodeficiency Virus (HIV) surrogate markers (CD4 count) and the plasma viral load [1]. IRIS is an adverse consequence of the restoration of the pathogen-specific immune responses in HIV-infected patients during the initial months of the Highly Active Antiretroviral Treatment (HAART). Multiple IRIS in a patient is extremely rare.
Case
A 40 year old male patient who was diagnosed to have HIV 5 years back, came to our hospital on 5th March 2010. He was taking homeopathic treatment for HIV. On examination, he was found to have oral candidiasis. There was no evidence of any other opportunistic infections (the chest X ray, ultrasound of the abdomen and the fundus examination were normal). His CD4 count was 22cells/μl and so he was started on anti retroviral treatment with lamivudine, stavudine and nevirapine. He was started on co- trimoxazole prophylaxis (sulfamethoxazole 800mg/ trimethoprim 160mg once daily).
He was again admitted on 14th May 2010 with the complaints of severe headache, vomiting and low grade fever of 5 days duration. On examination, it was found that there was neck rigidity and a positive Kernig's test. The fundoscopy did not show any papillooedema. So, a lumbar puncture was done. The CSF analysis revealed protein- 123mg/dl, glucose -16mg/dl, cells- 55/cumm, 90%- lymphocytes and 10% -neutrophils. The India ink stain was positive for Cryptococcus neoformans and the CSF culture also grew Cryptococcus (heavy growth) after 4 days of incubation. The patient was treated with Mannitol 100 ml IV three times daily and conventional Amphotericin B (1mg/kg) for 2 weeks and he was discharged on oral Fluconazole.
The patient was again admitted on 25th June 2010 with the complaints of pain in the abdomen in the epigastric region. His serum amylase was 112 mg/dl. So, stavudine was withheld and the patient was given tenofovir, emtricitabine and nevirapine. Zidovudine could not be given because he had anaemia. Due financial constraints, after one month, the patient was once again restarted on stavudine and lamivudine.
On 2nd August 2010, the patient got admitted with the complaints of headache and decreased vision in both the eyes. A CSF analysis was done, which showed protein -158.2mg/dl, glucose- 29mg/ dl, 50cells/cumm, 78%- neutrophils, 19%-lymphocytes and 3% eosinophils. The India ink staining for CSF, the AFB staining and the culture were negative. The patient was started on Ceftriaxone 2g IV twice daily, along with Dexamethasone and Mannitol.
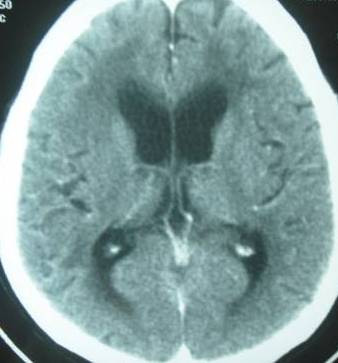
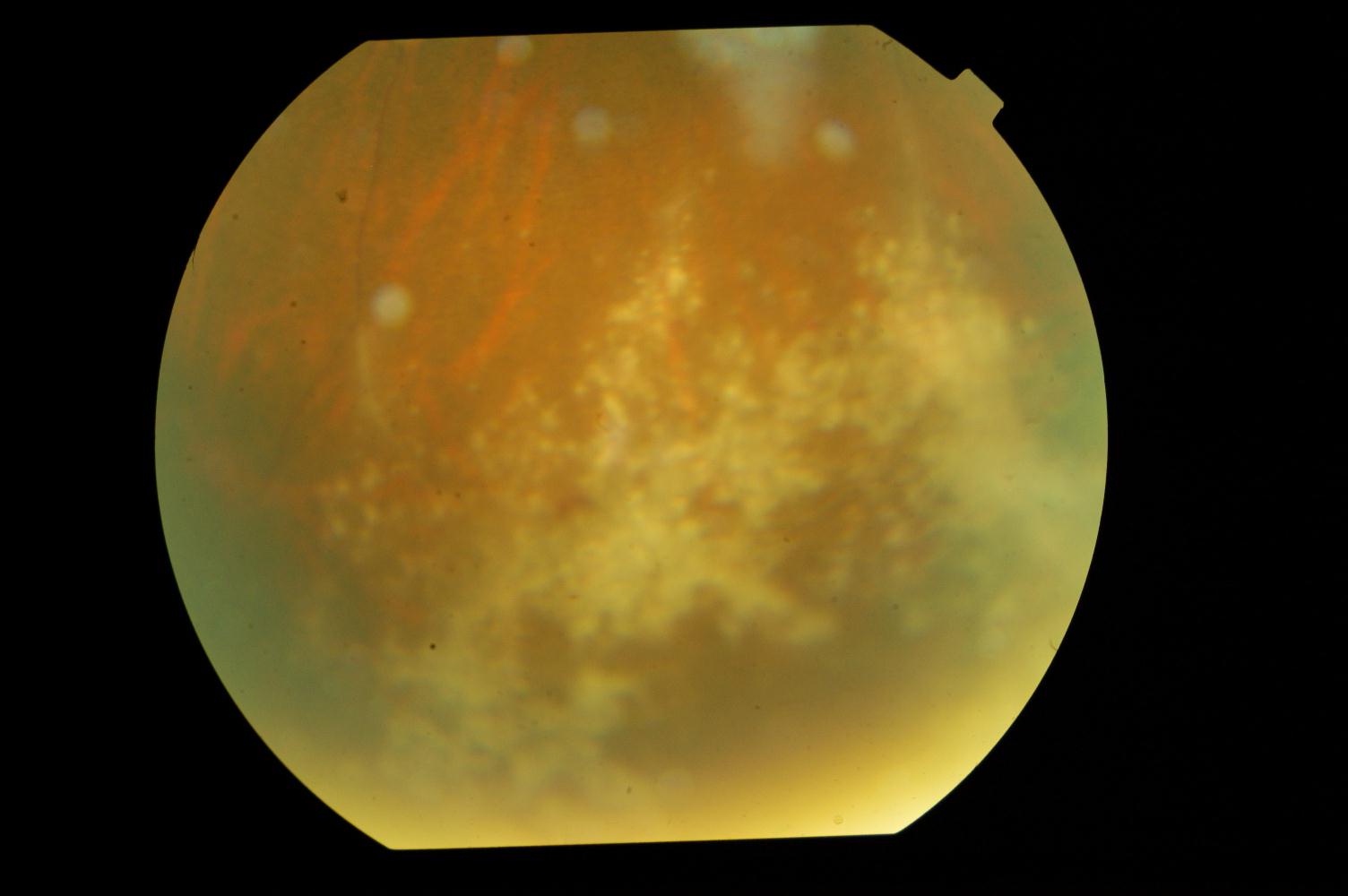
For the persisting headache, a CT scan of the head was done, which showed an obstructive hydrocephalus [Table/Fig-1]. His serum IgG for toxoplasma was positive, with a titre of 125.5IU/l. The patient was started on Trimethoprim160mg/Sulfomethoxazole 800mg 3 times daily and Sulfadoxine 500mg/ Pyrimethamine 25mg three times daily. An ophthalmology consultation was taken for the decreased vision, which showed the features of Cytomegalovirus retinitis in the peripheral retina [Table/Fig-2]. He was treated with the injection gancyclovir.
CT brain showing dilated ventricles
Fundus showing CMV retinitis
In view of the multiple opportunistic infections, a repeat CD4 count was done, which had improved to 107 and so we thought of a possibility of the immune reconstitution syndrome. We could not do a viral load study due to financial constraints. With the above treatment, the patient's headache subsided and he was discharged on 14th August 2010. The patient was on regular follow up for 6 months and then he was lost for follow up.
Discussion
French et al. have concluded that 25% of the HIV patients develop IRIS after the initiation of ART [2]. There are two types of IRIS: unmasking IRIS and paradoxical IRIS. Unmasking IRIS occurs when an Opportunistic Infection (OI) present pre-ART and re mains undiagnosed and subsequent immune recovery following ART initiation trig gers the presentation of OI with the development of unusual inflammatory features. In paradoxical IRIS, the infection, though it was previously treated, it worsens clinically after initiation of ART. Our patient had unmasking IRIS.
The risk factors for the development of IRIS are: the male sex, lower CD4+ cell count at ART initiation, a higher HIV RNA at ART initiation, an antiretroviral naive at the time of the OI diagnosis and a shorter interval between the OI therapy initiation and the ART initiation [3]. A low baseline CD4+ T cell count, below 50 cells/μl [4] is a major risk factor for IRIS. However, IRIS is known to occur even at higher CD4+ T-cell counts. In our patient, the base line CD4 count was low and after few months of therapy, a significant rise in the CD4 count was documented. Hence, his clinical deterioration was attributed to IRIS.
The opportunistic infections which are most commonly associated with IRIS are tuberculosis, cryptococcal meningitis, Cytomegalovirus CMV) retinitis, Herpes zoster, Herpes Simplex and Progressive Multifocal Leukoencephalopathy (PML) [5].
In many situations, IRIS manifests as a single infection, but our patient had various infections, starting from cryptococcal meningitis, toxoplasmosis and then CMV retinitis, which is a very rare occurrence. On review of the literature, we found only very few cases of multiple IRIS and no reports on the occurrence multiple IRIS from India. Asselman et al. [6] have described patient who presented with multiple IRIS. Their patient developed tuberculosis, then cryptococcosis, and later, Varicella Zoster Virus (VZV) IRIS.
Another significant finding was the occurrence of toxoplasmosis as IRIS in our case, which is rare [7]. Pfeffer et al. [8] have also described a case of toxoplasma IRIS. Hydrocephalus without a mass lesion is an unusual presentation of toxoplasmosis [9].
The diagnosis of IRIS is difficult because it has to be differentiated from the treatment failure. In treatment failure, there is a decrease in the CD4 count and an increase in the viral load, along with a clinical deterioration. In IRIS, a clinical deterioration occurs in the setting of increased CD4 counts and decreased plasma HIV viral loads.
Conclusion
A majority of the HIV-infected patients in our country present to the clinicians with advanced immunodeficiency (low CD4+ cell count) and Opportunistic Infections (OI).They need a rapid initiation of ART to minimize the overall mortality . Such patients are high risk candidates for IRIS. Our case highlighted the same. IRIS is a diagnosis of exclusion and a high index of suspicion is needed to identify it. IRIS has to be differentiated from treatment failure.
[1]. French MA, Price P, Stone SF, Immune restoration disease after antiretroviral therapyAIDS 2004 18:1615-27. [Google Scholar]
[2]. French MA, Lenzo N, John M, Mallal SA, McKinnon EJ, James IR, Immune restoration disease after the treatment of immunodeficient HIV-infected patients with highly active antiretroviral therapyHIV Med 2000 1:107-15. [Google Scholar]
[3]. Murdoch DM, Venter WD, van Rie A, Feldman C, Immune reconstitution inflammatory syndrome (IRIS): A review of common infectious manifestations and treatment optionsAIDS Res Ther. 2007 4:9 [Google Scholar]
[4]. Muller M, Wandel S, Colebunders R, Attia S, Furrer H, Egger M, Immune reconstitution inflammatory syndrome in patients starting antiretroviral therapy for HIV infection: a systematic review and metaanalysisLancet Infect. Dis. 2010 10:251-61. [Google Scholar]
[5]. Lawn SD, Meintjes G, Pathogenesis and prevention of immune reconstitution disease during antiretroviral therapyExpert Rev Anti Infect Ther. 2011 9:415-30. [Google Scholar]
[6]. Asselman V, Meintjes G, A patient with multiple IRISSouthern African Journal of HIV Medicine 2007 8:57 [Google Scholar]
[7]. Martin-Blondel G, Alvarez M, Delobel P, Uro-Coste E, Cuzin L, Cuvinciuc V, Toxoplasmic encephalitis IRIS in HIV-infected patients: a case series and review of the literatureJ Neurol Neurosurg Psychiatry 2011 82:691-93. [Google Scholar]
[8]. Pfeffer G, Prout A, Hooge J, Maguire J, Biopsy-proven immune reconstitution syndrome in a patient with AIDS and cerebral toxoplasmosisNeurology 2009 73:321-22. [Google Scholar]
[9]. Nolla-Salas J, Ricart C, D'Olhaberriague L, Galí F, Lamarca J, Hydrocephalus: an unusual CT presentation of cerebral toxoplasmosis in a patient with acquired immunodeficiency syndromeEur Neurol 1987 27:130-32. [Google Scholar]