The Bee Sting Related Wolff-Parkinson-White Syndrome
Shanmuga Ravi Santhosh M.1, Stalin Viswanathan2, Shanthi Kumar3
1. Intern, Department of Internal Medicine Pondicherry Institute of Medical Sciences, Pondicherry, India.
2. Assistant Professor, Department of Internal Medicine, Indira Gandhi Medical College, Pondicherry, India.
3. Assistant Professor, Department of Oral Pathology, Indira Gandhi Institute of Dental Sciences, Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Stalin Viswanathan, Assistant Professor, Department of Internal Medicine, Indira Gandhi Medical College Kathirkamam, Pondicherry -605009, India.
Phone: 9894787277
E-mail: stalinviswanathan@ymail.com
Hymenoptera stings are common reasons for emergency visits. The admissions for the hymenoptera stings occur for systemic or unusual reactions. We are reporting a man with multiple bee stings, who presented with dizziness and palpitations and was found to have ECG findings of the Wolff-Parkinson-White syndrome. He had no worsening of symptoms or new ECG changes during his hospitalization. The hymenoptera related cardiac effects have also been reviewed and summarized.
Hymenoptera stings, Coronary syndrome, Arrhythmia, Kounis syndrome
Introduction
Bees, hornets, wasps and ants are grouped under the order of hymenoptera. All these hymenopteran insects commonly cause local reactions. Unusual reactions which affect the cardiac, renal, pancreatic and the neurological systems have been rarely reported. We have described an electrocardiographic complication which arose from multiple bee stings, that has not been previously reported.
Case
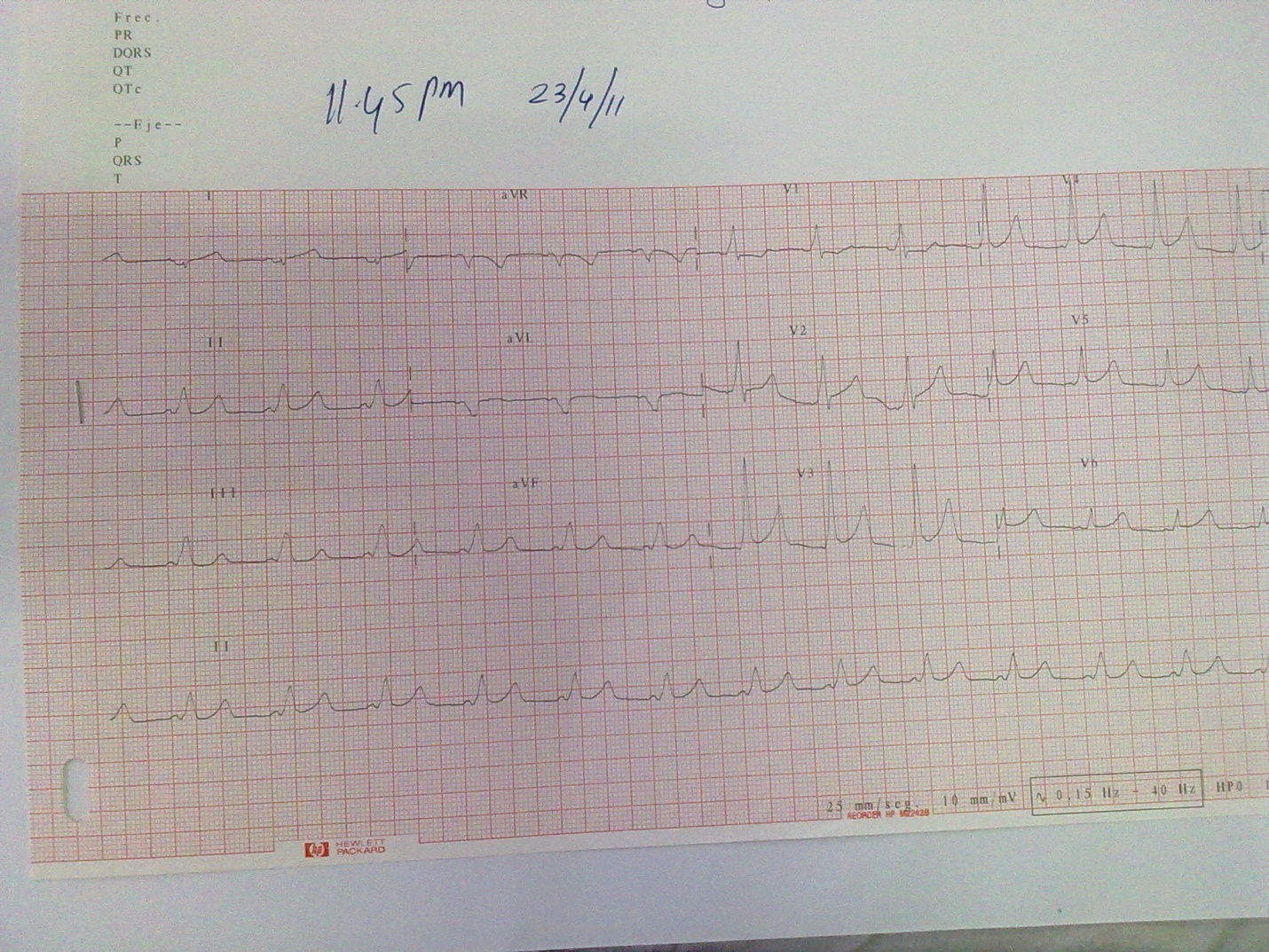
A 32-year old clerk who worked in a factory came with a history of multiple bee stings [~five] to his lips, right eye-lid and right ear lobe. There was no history of retained stingers. He was taken to the company's hospital with a history of palpitations and dizziness. He had only lip and ear lobe swellings, with an otherwise normal examination. He had been administered intravenous methyl prednisolone 125 mg and chlorpheniramine along with intramuscular diclofenac 50mg. He was referred to our institution in view of the electrocardiographic changes which were noted in that hospital. There were no other cardiorespiratory symptoms or signs. He had never smoked and was a teetotaler. He had no family history of heart disease. At admission, his pulse was 96/min, his blood pressure was 110/80mm Hg and his respiratory rate was 18/min, with a normal systemic examination. His upper lip and his right ear lobe had minimal swelling and redness. There were no other visible skin changes. His investigations revealed haemoglobin -13.4g/dL, total counts -9.0 × 109/L, with 92% neutrophilia, blood sugar -8.96mmol/L, urea- 8.93mmol/L, creatinine-80μmol/L, creatine kinase- [CK-MB] 16U/L, troponin I- negative and total IgE levels of 126U/L[<150]. His electrocardiogram revealed a short PR-interval and a delta wave which were suggestive of the Wolff-Parkinson-White syndrome (WPWS) [Table/Fig-1]. His echocardiography report was normal. The patient was observed in the hospital for 3 days and no new symptoms or new changes in the ECG were found. He was given injectable chlorpheniramine and hydrocortisone 100mg at the time of his admission. In view of his age, his non-smoking status and the absence of new symptoms, a coronary angiography was deferred after consultation with the cardiologist. The ECG findings subsided spontaneously on a follow up visit a week later.
ECG at admission revealing WPW syndrome
Discussion
The hymenoptera stings typically cause type IV hypersensitivity (IgG) mediated focal and large local skin reactions (>10cm), which our patient had. He also suffered a severe allergic reaction in the form of WPWS. The hymenoptera venom contains both allergenic [mainly phospholipase A2] and thrombogenic substances along with vasoactive mediators. These substances can cause either hypotension or hypertension. Hypertension and an increased myocardial oxygen demand can predispose to ischaemia just as hypotension can [1]. Mellitin, the major component of the bee venom induces catecholamine release [2]. Metalloproteinases like tryptases and leukotrienes, both of which mediate hypersensitivity reactions, have a multitude of cardiac effects that include the destabilization of plaques and coronary vasospasm. Intravenous injections of Africanized Bee Venom [ABV] into Wistar rats had caused elevations of cardiac noradrenaline and acute myocardial infarction lesions [3]. The ABV injection temporarily causes reduction in the heart rate and the mean arterial pressure, which is similar to the picture in the Bezold-Jarisch reflex. ABV consists of vasoconstrictors like adrenaline and noradrenaline and vasodilators like histamine. Histamine modulates inflammatory cells, activates platelets and can cause coronary vascoconstriction [4]. Hypertension and subsequent ischaemia [which are partly contributed by the direct myocardial toxicity] can lead to infarction and ECG changes. These effects on the heart may be reduced by atropine [5].
Coronary events are very rare in the hymenoptera stings. Bee sting fatalities are generally associated with the preexisting coronary lesions. Coronary events and electrocardiographic changes have been described in three hymenoptera families-namely the bees, wasps, and the hornets. Twenty four odd cases of Myocardial Infarction (MI) in hymenoptera stings have been reported [Table/Fig-2]. Wasp and bee stings have similarly caused 9 and 13 cases of MI respectively [Table/Fig-2]. Two acute coronary syndromes 1 with and 1 without an ST elevation MI] have been described following hornet stings [3]. Other electrocardiographic changes have been described in hymenoptera stings. These changes include ischaemia, atrial flutter and fibrillation, a right bundle branch block, ventricular fibrillation (VF), ventricular ectopics, and a wandering pacemaker [6–10]. The patient with VF briefly became comatose following hypoxia. Atrial arrhythmias occur in patients with preexisting atrial diseases like the left atrial enlargement.
Coronary syndromes and electrocardiographic changes in hymenoptera stings
| 1 | 2011 | Wasp | Myocardial infarction [MI] | Valla et al. |
| 2 | 2011 | Bees | Kounis syndrome | Karasu et al. |
| 3 | 2010 | Bees | ECG changes of MI- 2 children | Biteker et al. |
| 4 | 2009 | Bees | Acute coronary syndrome | Murat et al. |
| 5 | 2009 | Wasps | Stent thrombosis, MI | Greif et al. |
| 6 | 2009 | Hornets | MI | Cvetkovic-Matic D. et al. |
| 7 | 2009 | Bees | MI | Mytas et al. |
| 8 | 2009 | Bees | MI | Taqqar et al. |
| 9 | 2008 | Bees | Ventricular fibrillation | Quercia et al. |
| 10 | 2008 | Bees | MI, ST segment elevation, RBBB | Erbilen et al. |
| 11 | 2008 | Bees, wasp | 1 case each; MI, normal coronaries | Bitekar et al. |
| 12 | 2006 | Hornet | MI with Atrioventricular block | Korantzopoulos et al. |
| 13 | 2005 | Wasp | Acute MI | Bongo et al. |
| 14 | 2003 | Wasp | Silent MI | Lombardi et al. |
| 15 | 2003 | Wasp | Atrial flutter | Fisher et al. |
| 16 | 2002 | Wasp | Acute MI | Calveri et al. |
| 17 | 2001 | Bees | MI | Quercia et al. |
| 18 | 2001 | Bees | MI | Ceyhan et al. |
| 19 | 2000 | Bees | MI | Magadle et al. |
| 20 | 1997 | Bees | Atrial flutter and fibrillation | Law et al. |
| 21 | 1994 | Bees | posterior wall MI | Engrav et al. |
| 22 | 1994 | Wasp | Acute MI | Wagdi et al. |
| 23 | 1988 | Bees | Ischemic ECG changes | Nagaratnam et al. |
| 24 | 1988 | Wasp | Acute MI | Jones et al. |
| 25 | 1979 | Yellow jacket | Electrographic changes | Rowe et al. |
| 26 | 1997 | Bees | MI | Massing et al. |
| 27 | 1976 | Wasps | Acute MI | Levine et al. |
| 28 | 1974 | Wasps | Reversible electrographic changes | Brasher et al |
| 29 | 1972 | Hornet | Ventricular ectopics | Shilkin et al. |
| 30 | 1970 | Hornet | Ventricular ectopics | Durie et al. |
The electrocardiographic changes in hymenoptera envenom-ation have been postulated to be caused by the use of epinephrine, myocardial ischaemia which is caused by bronchoconstriction related hypoxia [5,7], an anaphylaxis related coronary vasospasm or a preexisting heart disease. The coronary syndrome which is related to allergic reactions [venom, drugs] is called the Kounis syndrome [4]. The patients with this syndrome generally have ECG changes of infarction and elevated cardiac enzymes. But our patient never had angina nor did he have elevated cardiac enzymes (troponin I and CK-MB). Intradermal venom skin tests and increased histamine/ tryptase levels are generally observed in these patients. We did not have the facilities for conducting such tests. Only tachyarrhythmias had been previously reported with bee stings [8,9].
In conclusion, bee stings can rarely cause electrocardiographic changes which may or may not be life threatening; sometimes they are associated with coronary events. An ECG may be required for all the victims of hymenoptera stings, even in the absence of systemic symptoms, during emergency visits. Due to the rare coronary events, their observation periods will have to be extended as well.
[1]. Greif M, Pohl T, Oversohl N, Reithmann C, Steinbeck G, Becker A, Acute stent thrombosis in a sirolimus eluting stent after a wasp sting which caused acute myocardial infarction: a case reportCases J 2009 2:7800 [Google Scholar]
[2]. Fitzgerald KT, Flood AA, Hymenoptera stingsClin Tech Small Anim Pract 2006 21:194-204. [Google Scholar]
[3]. Guimaraes JV, Costa RS, Machado BH, dos Reis MA, The cardiovascular profile after an intravenous injection of Africanized bee venom in awake ratsRev Inst Med Trop Sao Paulo 2004 46:55-58. [Google Scholar]
[4]. Kounis NG, The Kounis syndrome (allergic angina and allergic myo-cardial infarction): a natural paradigm?Int J Cardiol 2006 110:7-14. [Google Scholar]
[5]. Nagaratnam N, Husodo H, James WE, Electrocardiographic changes following bee-sting anaphylaxisJ R Soc Med 1988 81:420-21. [Google Scholar]
[6]. Korantzopoulos P, Kountouris E, Voukelatou M, Charaktsis I, Dimitroula V, Siogas K, Acute myocardial infarction after a European hornet sting-a case reportAngiology 2006 57:383-86. [Google Scholar]
[7]. Engrav MB, Zimmerman ME, The electrocardiographic changes which were associated with anaphylaxis in a patient with normal coronary arteriesWest J Med 1994 161:602-04. [Google Scholar]
[8]. Law DA, Beto RJ, Dulaney J, Jain AC, Lobban JH, Schmidt SB, The atrial flutter and fibrillation following bee stingsAm J Cardiol 1997 80:1255 [Google Scholar]
[9]. Quercia O, Emiliani F, Foschi FG, Stefanini GF, Ventricular fibrillation after a hymenoptera stingInt J Cardiol 2008 127:e5-7. [Google Scholar]
[10]. Erbilen E, Gulcan E, Albayrak S, Ozveren O, Acute myocardial infarction which was caused by a bee sting, which was manifested as an ST wave elevation after the hospital admissionSouth Med J 2008 101:448 [Google Scholar]