Introduction
Carcinoma of the breast is one of the commonest malignancies in woman. It would thus seem worthwhile to characterize and to subdivide this type of cancer with the appropriate markers to predict its prognosis and therapeutic approach. Keratins have a number of distinct advantages as the marker proteins [1]. The expression of the intermediate filaments, particularly cytokeratins (Ck), components of the cytoskeleton of the cell, reflects the epithelial cell type, the state of the tissue growth and the tissue differentiation in addition to the functional status of the tissue.
However, a huge effort had been put forth in the last decade to establish new prognostic factors that are based on the functional criteria rather than on the morphologic features of this disease. Towards this end, determining the oestrogen and the progesterone receptor statuses, the expressions of Cathepsin D and Her-2/neu and the roles of several other oncogenes have been used to predict the prognosis [2,3].
The luminal cells in the resting mammary gland mainly express Ck7, Ck8, Ck18 and Ck19 but not Ck20; in contrast to this, the basal/myoepithelial cells express Ck5/6, Ck14 and Ck17 [4]. In invasive breast carcinoma, a vast majority of the cases show positivity for Ck7/8, 18 and 19, thus indicating a differentiated glandular phenotype, a finding which is associated with the ER positivity, an older patient age and a good prognosis. In contrast, the basal marker expression was found to be significantly related to a poor prognosis, ER negativity and a younger patient age [5]. The oestrogen receptor assays predict the clinical responses correctly in two thirds of the patients with ER positive tumours, whereas virtually, all the ER negative tumours fail to respond to the endocrinal therapy. Similarly, the ER positive tumours have a longer disease free survival as compared to the oestrogen receptor negative tumours [6].
Her-2/neu is a transmemberane glycoprotein which is involved in the cell growth control and its overexpression carries a poor prognosis. The present study was aimed at the immunohistochemical application of Ck 8/18, Ck 5/6, ER, and Her-2/neu on invasive ductal carcinoma for a further classification.
Materials and Methods
The study group comprised of 39 cases of breast carcinoma, whose samples were received in the Department of Pathology, GMC, Amritsar, India for the analysis of the expression of cytokeratin 8/18, Ck5/6, ER , and Her-2/neu by immunohistochemistry on four micron thick paraffin embedded tissue sections. The immunostaining was performed by the standard peroxidase – anti-peroxidase method by using a prediluted liquid mouse monoclonal antibody which was specific for the human Ck 8/18 intermediate filament protein, clone: Rtu-5D3 (novocastra), an ER prediluted monoclonal mouse ER antibody Rtu- ER-6F11 (novocastra), the Her-2/neu monoclonal mouse anti Her-2/neu clone CB11(novocastra) and the Ck5/6 primary antibody : monoclonal mouse antihuman Ck 5/6 clone D5/16B4 (DAKO code:7237).
Observations and Results
Histologically, 37 cases were diagnosed to have invasive ductal carcinoma and no special type with one case each of mucinous and IDC with a squamous differentiation. The ages of these patients varied between 20-80 years, with 71.5% cases in the third to the fifth decades of life. The tumour size ranged from less than 2cm to 15cm in the greatest dimensions and 27 cases were of grade III, ten being of grade II and only two cases being of grade I. Lymph nodes were recovered in 26 cases, of which ten cases showed a reactive pathology and the rest showed metastatic deposits. No definite correlation of the metastases was seen with the histological grades.
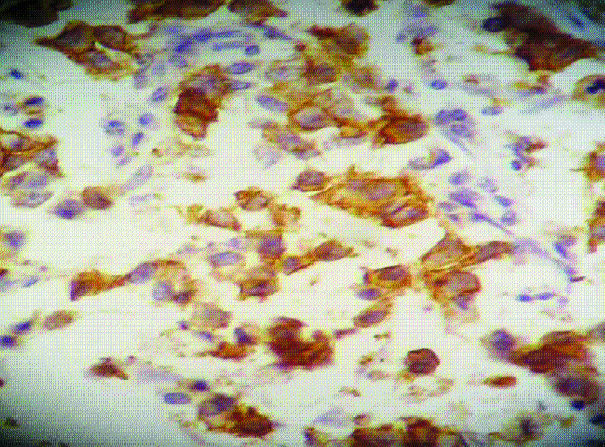
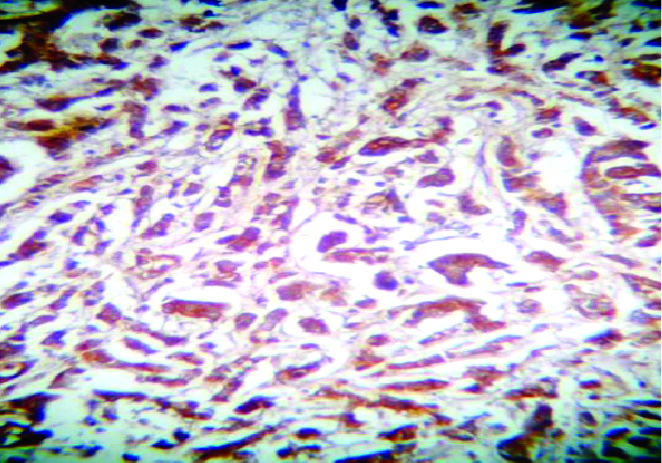
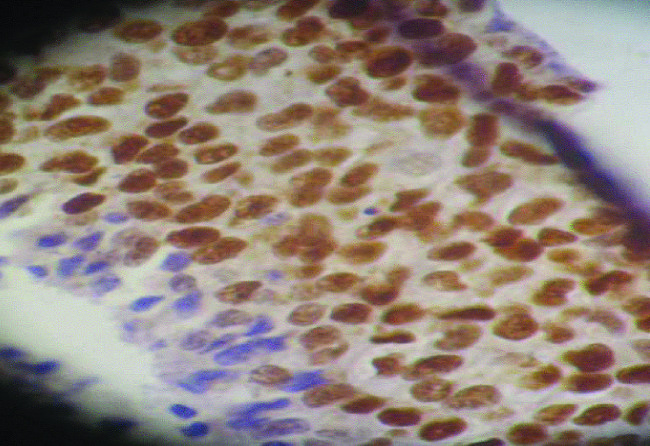
Immunohistochemical Staining for Ck 8/18, Ck5/6, ER and her-2/neu of the 39 cases, 33 cases were positive for Ck8/18, 7 were positive for ER and Ck 8/18, and 8 were positive for HER-2/neu and Ck 8/18, which showed a luminal type of pathology, while 6 cases were negative for all the 3 markers. One case was positive for all the 3 markers, which was of grade III. It was observed that the Her-2/neu and the Ck8/18 positivities increased with the grade, with the maximum positivities being seen in grade III [Tables/Fig-1, 2, 3, 4].
Immunohistochemical Expression of Immunological Markers
The value in the bracket shows percentage.
| Grade | Ck8/18 | ER | Her-2/neu | Ck5/6 |
|---|
| + | – | + | – | + | – | + | – |
| I | 2 | 0 | 1 | 1 | 0 | 2 | 0 | 0 |
| II | 9 | 1 | 3 | 7 | 1 | 9 | 1 | 0 |
| III | 22 | 5 | 3 | 24 | 7 | 20 | 6 | 21 |
| Total | 33 (85) | 6 (15) | 7 (18) | 32 (82) | 8 (20) | 31 (80) | 7 (25) | 21 (75) |
Immunohistochemical staining with Her-2/ neu in a case of infiltrating ductal carcinoma
Immunohistochemical staining with cytokeratin 8/18 in a case of infiltrating ductal carcinoma
Immunohistochemical staining with Estrogen receptor in a case of infiltrating ductal carcinoma
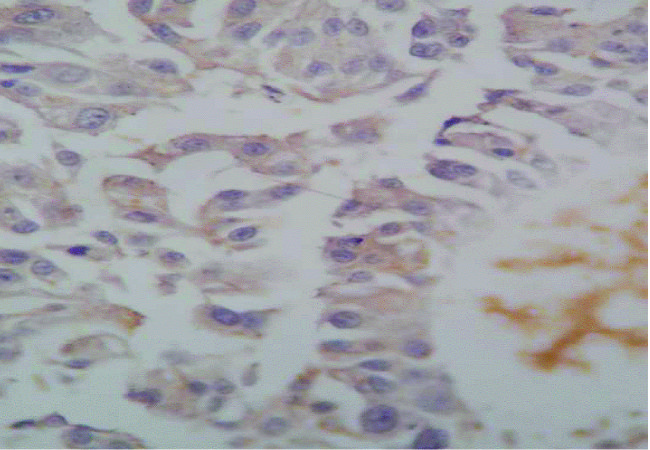
Twenty eight cases were subjected to the evaluation of Ck5/6, especially 6 cases which were negative for Ck8/18, ER and HER-2/neu and it was observed that a total of 4 cases were positive for Ck5/6 and Ck8/18, which were found to be of combined type, whereas 3 cases which were negative for the 3 markers were found to be positive for Ck5/6. They were found to be of basal type, whereas the remaining 3 cases which were negative for all the markers were considered to be of the null type [Table/Fig-5].
(X400): Immunohistochemical staining with cytokeratin 5/6 in a case of infiltrating ductal carcinoma
Discussion
In the human mammary gland, 2 cell types are distinguished immunohistochemically; the basal (and/or myoepithelial) cells can be stained with the antibodies against keratin 5/6, whereas the luminal epithelial cells can be stained with the antibodies against keratin 8/18 [7]. The luminal cells may be positive or negative for ER, PR and Her-2/neu.
The ER-positive/luminal tumours can be grouped into two 2 sub-types, luminal A and luminal B. The luminal A tumours demon-strate the highest expression of the ER and the ER related genes and they show the best prognosis. The luminal B tumours have profiles which are enriched for the ‘luminal genes’, but they show a low to moderate expression of the genes which pertain to the ER cluster. As compared to the luminal A tumours, they may have a higher proliferation rate, they may express genes that seem to be shared with the basal-like and the Her-2 subtypes and they are associated with a less favourable outcome [8,9]. The high Ki67/ER factor scores were strongly associated with the higher grade and the luminal B type of tumours, but they were also detected in a set of grade1and luminal A cases , thus potentially indicating the high risk patients in these categories [10].
In the present study, the incidence of the Ck 8/18 positivity was seen in 85% cases, whereas the study which was done by Rejthar et al showed a 100% positivity, ( z = 2.62, p < 0.05 ) [11]. In the literature observations which were made by different authors, it was found to range from 83%-100% [1,5,11,12]. As a majority of tumours arise from the luminal epithelial cells, it was observed that as the grade increased, the positivity for Ck8/18 also increased, with 56% cases of the grade III tumours expressing Ck8/18. The tumour of any grade, if it is positive for Ck8/18, carries a good prognosis, as compared to the tumours which are negative for Ck8/18. An elevated keratin 18 expression indicates a favourable prognosis in the patients with breast cancer and it has a higher impact on the prognosis than all other factors, which include the lymph node status and the tumour size. The highly metastatic cell lines are associated with a loss of the Ck8/18 expression [3,5]. DM-Abd et al described that a vast majority of the cases showed positivity for Ck7/8,18 and 19, thus indicating a differentiated glandular phenotype, a finding which was associated with a good prognosis and longer overall survival, as compared to those with a low or no expression of these luminal markers. Ck8 is associated with a better overall survival and it is an independent prognostic indicator of the relapse free survival. The Ck18 expression is an inde-pendent prognostic factor for predicting the overall survival [5].
In the present study, 18% cases were positive for ER and Ck 8/18, whereas Domenico Coppola reported 56% of the cases to be positive (z = 6.18, p < 0.05) [13]. This showed that there was marked difference in India and other countries, which may be due to the racial differences, the low prevalence of the oral contraceptives and the hormone replacement therapy. In the Indian studies, the oestrogen receptor positivity in the breast tumours was reported to vary from 24% , 31.6% to 32.6%[14,15].
The present study showed 20% cases to be positive for Her-2/neu and Ck8/18. Kumar V et al., showed a Her-2/neu oncogene over expression in 46.37% Indian patients, (Z=4.12,P<0.05) [16]. The Her-2/neu oncogene overexpression was higher (46.37%) among the Indian patients as compared to the 20 to 30% overexpression which was seen in most of the western literatures [2,16]. The Her-2/neu positivity represents an aggressive form of breast cancer which needs treatment with adjuvant therapy and which is resistant to the hormonal therapy. If the Her-2/neu overexpressing primary tumours are treated in combination with cytotoxic chemotherapy, this can increase the time of the recurrence and the overall response rate in metastatic breast cancer, while the patients with positive ER can benefit from the hormonal therapy. Although most of the cDNA expression studies have not characterized the luminal B group of tumours based on the expression of Her-2/neu protein itself, but on the expression of the genes which are characteristic of the Her-2 positive tumours and a high proliferation rate, many authors have used Her2 protein expression to differentiate between the luminal-A and -B subtypes of the tumours [8].
Another report in the literature demonstrated that the IHC Her-2/neu equivoical cases were a heterogenous group and that they needed FISH for a further categorization [17]. The interrelationship of ER and HER2/neu has come to have an important role in the management of breast carcinoma.
Eighty five percent cases were positive for Ck8/18, 18% were positive for ER and Ck8/18 and 20% were positive for Her-2/neu and Ck8/18, which showed that they were of the luminal type. Twenty eight cases were subjected to the evaluation of Ck 5/6, which included 6 cases which were negative for Ck 8/18, ER and Her-2/neu. A total of 25% cases were found to be positive for Ck 5/6, of which 10.71% cases were positive for Ck 5/6 and 14.28% were positive for Ck 5/6 and Ck 8/18, which showed that they were of the basal and the combined types respectively and 10.71% cases were negative for all the four markers, which were considered to be of the null type. DM-Abd et al., also reported that some of the cases did not express any of the markers (null type -0.4% and basal- type 0.8%). The expressions of the basal markers, Ck5/6, Ck14 and SMA have been reported in invasive breast carcinomas, which were found in 4% to 16% of the cases [18]. Similar findings were observed by others and the tumours which were classified to be of the basal phenotype (the combined luminal plus the basal and the pure basal) were seen in the poor prognostic groups [5].
One case of Grade III was positive for Ck8/18, ER and HER2/neu. Gene expression analysis has identified several breast cancer subtypes which differ markedly in their prognosis and in the repertoire of the therapeutic targets that they express. The subtype definitions were as follows: luminal A (ER+ and/or Progesterone receptor (PR) +, Her-2/neu-), luminal B (ER+ and/or PR+, HER2+), basal like (ER-,PR-,Her2-, Ck5/6+,and/or Her1+), Her-2+/ER-(ER-,PR-,and Her2+), and unclassified (negative for all the 5 markers). The disease specific survival was significantly lower among the breast cancer cases with the basal like and the Her2+/ER- tumours and it was more favourable among the cases with the luminal A tumours [9].
Several studies have shown that approximately one-third of the lymph node-negative breast cancer patients who were classified as lying within a ‘good prognostic group’ developed recurrence, whereas a similar proportion of node positive patients remained free from the development of distant metastases. On the other hand, a significant proportion of the patients who are allocated to the poor prognosis group will never develop a distant recurrence. Therefore, there is an increasing need for additional prognostic factors to improve the patients’ risk stratification and the targeting of the treatment for those who will truly benefit, thereby avoiding an iatrogenic morbidity in those who will not.
Conclusions
From this study, it has been concluded that all the cases which are ER negative should be subjected to Her-2/neu, Ck 8/18 and Ck 5/6 expression studies as the tumours which express Her-2/neu and Ck 5/6 or none of the markers carry a poor prognosis and different therapeutic approaches.
[1]. Tsubura A, Okada H, Senzaki H, The keratin expression in the normal breast and in breast carcinomaHistopathology 1991 18:517-22. [Google Scholar]
[2]. Slamon DJ, Clark GM, Wong SG, The human breast cancer correlation of relapse and survival with amplification of the Her-2/neu oncogeneScience(Washington DC) 1987 235:177-235. [Google Scholar]
[3]. Schaller G, Fuchs IIKA, Pritze W, The elevated keratin 18 protein expression indicates a favourable prognosis in patients with breast cancerClin Cancer Res 1996 2:1879-85. [Google Scholar]
[4]. Moll R, Krepler R, Franke WW, The complex cytokeratin polypeptide patterns which are observed in certain human carcinomasDifferentiation 1983 23:256-69. [Google Scholar]
[5]. Abd EI-Rehim DM, Pinder SE, Paish CE, Expressions of the luminal and the basal cytokeratins in human breast carcinomaJournal of Pathology 2004 203(2):661-71. [Google Scholar]
[6]. Susan EH, Graham AC, Walter CW, Towards an integrated model for the breast cancer etiology: The lifelong interplay of genes, lifestyles and hormonesBreast Cancer Res 2004 6(5):213-8. [Google Scholar]
[7]. Perou CM, Sorlie T, Eisen MB, The molecular portraits of human breast tumoursNature 2000 406:747-52. [Google Scholar]
[8]. Rakha EA, EI-Sayed ME, Reis-Filho JS, The expression profiling technology: its contribution to our understanding of breast cancerHistopathology 2008 52:67-81. [Google Scholar]
[9]. Carey LA, Perou CM, Livasy CA, Race, the breast cancer Subtypes, and the survival in Carolina. A Breast Cancer StudyJAMA 2006 295:2492-502. [Google Scholar]
[10]. Laurianavicius A, Laurinaviciene A, Ostapenko V, Dasevicius D, Jarmalaite S, Lazutka J, The immunohistochemistry profile of breast ductal carcinoma: the factor analysis of the digital image analysis dataDiagnostic Pathology 2012 March16:7-27. [Google Scholar]
[11]. Rejthar A, Nenutil R, The intermediate filaments and the prognostically oriented morphological classification in ductal breast carcinomaNeoplasma 1997 44:370-3. [Google Scholar]
[12]. Heatley M, Maxwell P, Whiteside C, Toner P, The cytokeratin intermediate filament expression in benign and malignant breast diseaseJ Clin Pathol 1995 48:26-32. [Google Scholar]
[13]. Coppola D, Catalano E, Santo V, Nicosia The significance of the p53 and the Bcl 2 protein expressions in human breast ductal carcinomaCancer Control 1999 6(2):181-7. [Google Scholar]
[14]. Dutta V, Chopra GS, Sahai K, The hormone receptors, Her-2/Neu and the chromosomal aberrations in breast cancerMJAFI 2008 64:11-5. [Google Scholar]
[15]. Desai SB, Moonim MT, Gill AK, The hormone receptor status of the breast cancer patients in IndiaBreast 2000 9(5):267-70. [Google Scholar]
[16]. Kumar V, Tewari M, Singh U, Shukla HS, Significance of the HER2/neu protein overexpression in Indian breast cancer patientsIndian Journal of Surgery 2007 69(3):122-8. [Google Scholar]
[17]. Murthy SS., Sandhya DG, Ahmed F, Assessment of the HER2/Neu status by fluorescence in situ hybridization in the immuno-histochemistry-equivocal cases of invasive ductal carcinoma and aberrant signal patterns: A study at a tertiary cancer centerIndian Journal of Pathology and Microbiology 2011 July-September54(3):532-8. [Google Scholar]
[18]. Nagle RB, Bocker W, Davis JR, The characterization of breast carcinomas by two monoclonal antibodies which distinguish the myoepithelial from the luminal epithelial cellsThe Journal of Histochemistry and Cytochemistry 1986 34(7):869-81. [Google Scholar]