Introduction
Giardia lamblia is a flagellated protozoan parasite of man. Only 2 stages i.e. the trophozoite and the cyst forms are observed in the life cycle of Giardia. The Giardia infection is acquired from drinking water or by eating food which is contaminated with cysts. The symptoms of the Giardia infection are foul smelling diarrhoea, flatulence, steatorrhoea, etc. Stool samples from the patients are examined for the detection of the motile trophozoites and cysts. As the trophozoites disintegrate rapidly, the stool sample should be observed within 15 minutes of its passage. Hence, we developed a staining method to stain the Giardia trophozoite permanently.
Materials and Methods
Smears of the stool samples were prepared and they were fixed with methanol. The staining was done by using a 1% methylene blue solution.
Results
All the 15 known Giardia lamblia trophozoite positive samples were also found to be positive by the Methylene blue staining. The Giardia lamblia cysts could not be stained by this method. 20 stool samples were used as negative controls.
Conclusion
We developed the methylene blue staining for demonstrating the trophozoite of Giardia, which is a very simple permanent staining method. The slides can be kept for a permanent record.
Giardia trophozoite, Methylene blue staining, Simple, One step method
Introduction
Among the intestinal flagellates, Giardia lamblia and Dientamoeba fragilis are pathogenic to man. G.lamblia/ G.intestinalis is a flagellated protozoan parasite of man. It was first observed in 1681 by Antony van Leuwenhoek in his own stool. In 1883, the genus, Giardia was named after Prof. A.M. Giard of Paris. In 1915, Stiles named it as Giardia lamblia [1]. In 2004, a waterborne outbreak which was caused by the contamination of a municipal water supply, occurred in Bergen(Norway), where 1300 laboratory confirmed cases were found and 2500 persons received medical treatment [2].
The Giardial infection is acquired from drinking water or by eating food which is contaminated with the cysts of Giardia. Giardia can survive in water for upto 3 months and thus the chances of acquiring Giardiasis increases many fold, as compared to the infection with other parasites. The incubation period for Giardiasis is about 12-20 days.
Giardia is also harboured by animals like cats, dogs, cattle, rodents and horses. The beaver, which is a rodent of north America, favours the Giardia transmission by building dams which are known as beaver dams. Wild-life lovers who frequently visit forests are at high risk of acquiring the Giardia infection on drinking water from streams or rivers. Hence, Giardiasis is also known as Beaver Fever or Backpacker’s Diarrhoea. Along with E.histolytica, G.lamblia has been identified as a sexually transmitted pathogen among those who practice the oral-anal sex [3].
The Giardia trophozoite does not appear consistently in the stools of all the patients. There are 3 patterns of excretion of Giardia:
High – When Giardia is present in nearly all the stool samples of the patient.
Low – When Giardia is present in approximately 40% of all the stool samples of the patient.
Mixed – When there is a 1-3 week period of a high excretion rate which alternates with a shorter period of a low excretion.
Stools should be examined for the Giardia trophozoites within 15 minutes of their passage, since this trophozoite disintegrates rapidly [4]. Hence, we developed a staining method for staining the Giardia trophozoite.
Materials and Methods
A total number of 15 Giardia trophozoite positive, 10 Giardia cyst positive and 20 Giardia negative stool samples were processed. All the stool samples were first screened by the ‘saline and iodine wet mount’ preparation. Then, 3 faecal smears were prepared from each stool sample.
In the methylene blue staining, all the faecal smears were fixed with methanol and they were stained with 1% methylene blue solution. They were kept for 2 minutes and were washed with tap water. After air drying, the smears were observed under an oil immersion lens. The Methylene blue powder was procured from HiMedia Pvt. Ltd. India (Code no. RM955).
Result
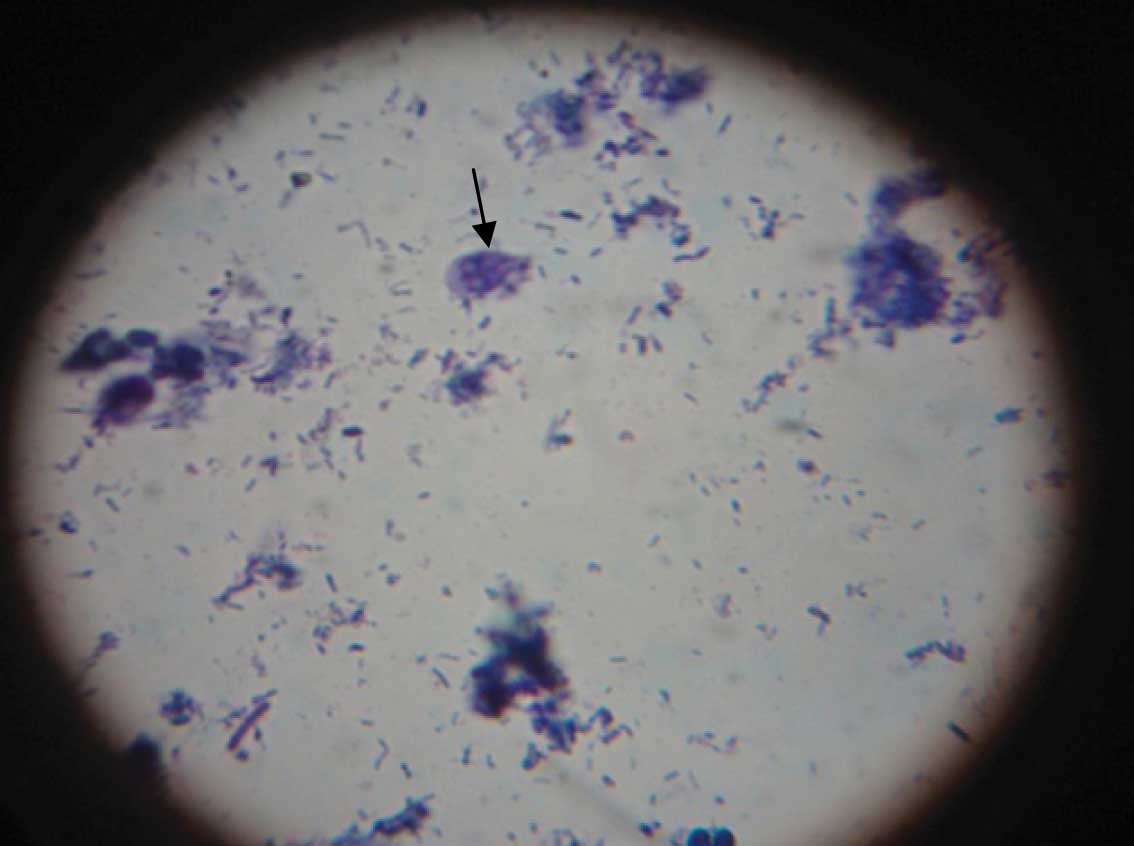
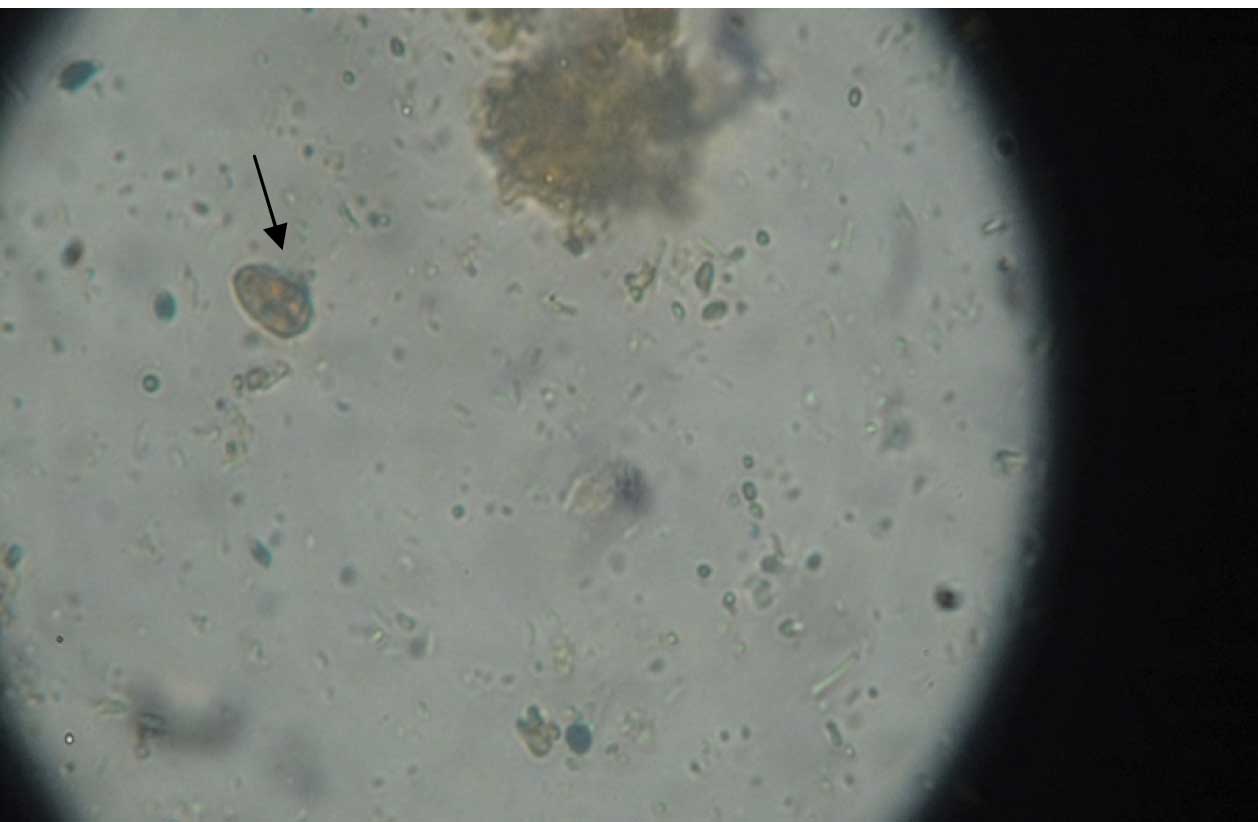
All the 15 Giardia trophozoite samples which were positive on the saline wet mount preparation were also positive on methylene blue staining [Table/Fig-1]. 20 stool samples which were negative for the Giardia trophozoite were also negative on methylene blue staining. But 10 stool samples which were positive for the Giardia cysts on the saline wet mount and the iodine preparation of the stools [Table/Fig-2], were also negative on methylene blue staining, as the Giardia cysts do not take up the methylene blue staining.
Methylene Blue staining showing Giardia trophozoite
Iodine wet mount showing Giardia cyst
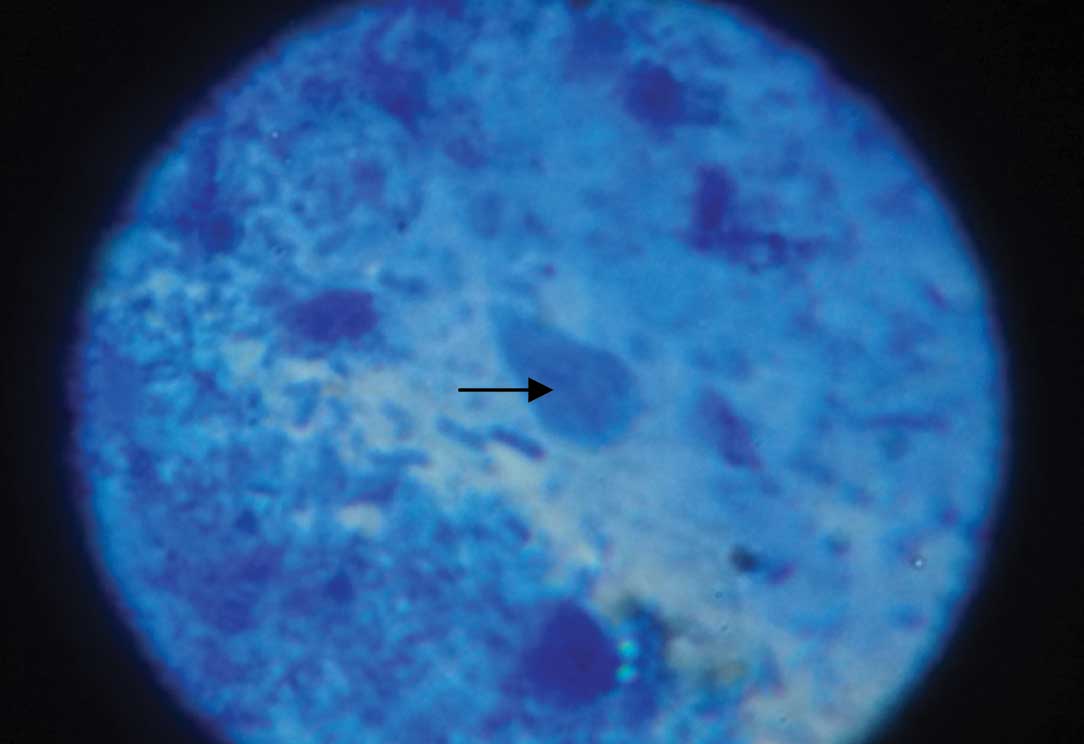
In one child, which was a case of acute lymphatic leukaemia (ALL) with watery diarrhoea, the transportation of the stool sample to the laboratory was delayed for 4 hours due to some unexplainable reason. In the saline wet mount preparation, some structures which resembled the Giardia trophozoite were seen, but no characteristic motility was observed. But the smear was prepared with specimen and stained with methylene blue, where the Giardia trophozoite could be seen very well [Table/Fig-3].
Methylene blue staining showing Giardia trophozoite in stool specimen of ALL case
Discussion
The life cycle of Giardia alternates between an actively motile trophozoite and an infective cyst. The Giardia lamblia trophozoites are pear shaped and they measure 10-20 μm in length and 5-15 μm in width. There are 4 pairs of flagella, 2 nuclei, 2 axonemes and 2 slightly curved bodies which are called median bodies. In the saline wet mount preparation, the Giardia trophozoites have a characteristic monkey face appearance or an old man appearance and the trophozoites are motile, showing the typical falling leaf motility.
The Giardia cysts are usually 11-14μm in length and 7-10μm in width and they are either round or oval in shape and contain 4 nuclei, axonemes and median bodies. A ‘halo effect’ outside the cyst wall may be observed because of the shrinkage which is caused by dehydrating agents, especially in the permanent staining [5].
The life cycle of Giardia lamblia in human is as follows:
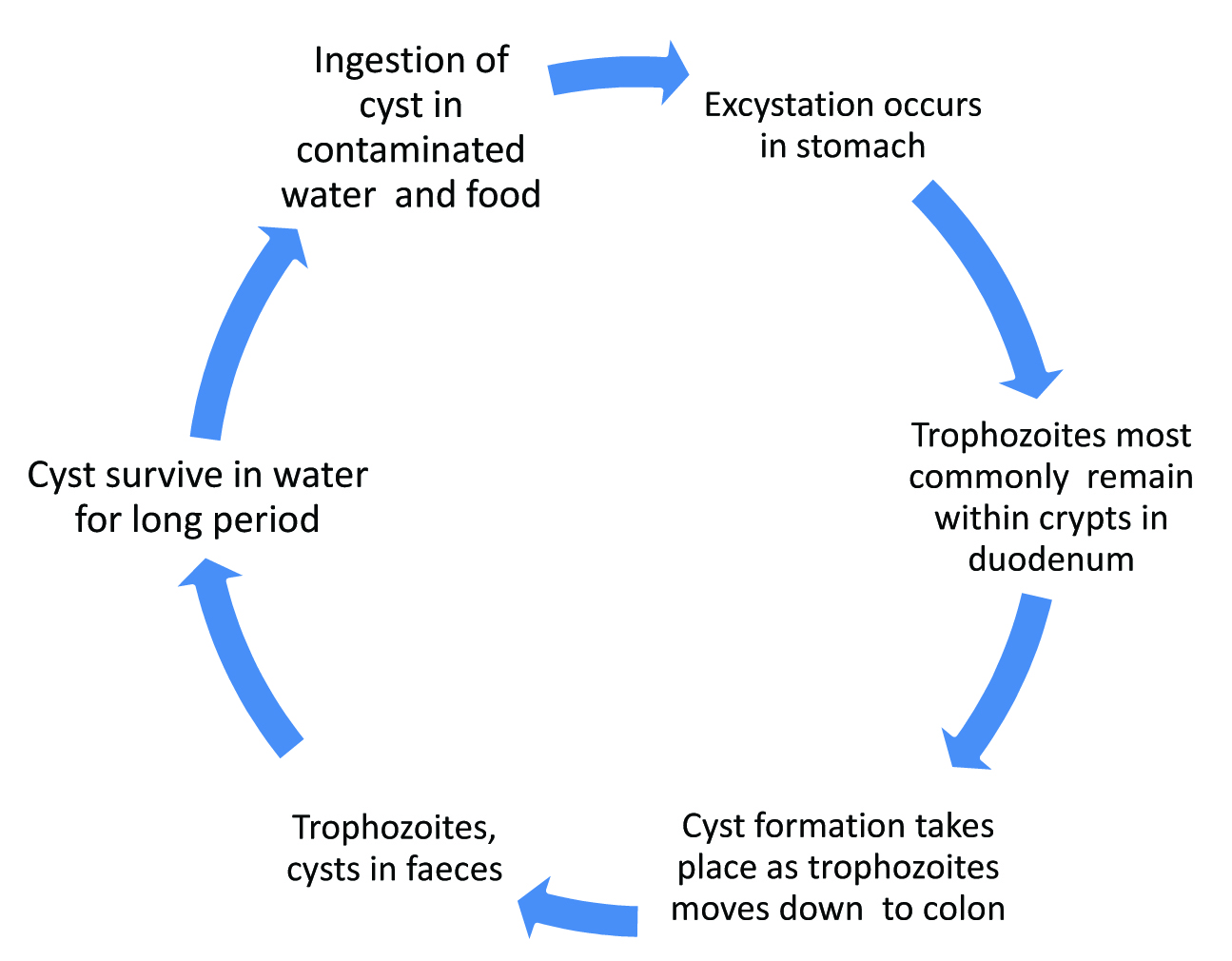
As the acute stage of the disease lasts for only a few days, the Giardiasis is not always recognized . The differential diagnoses are acute viral enteritis, bacterial food poisoning, intestinal amoebiasis or an infection with toxigenic Escherichia coli. After the cyst is ingested by man, excystation occurs in the stomach. Then the trophozoite reaches the upper part of the small intestine. Most commonly, the trophozoite remains in the crypts within the duodenum. The growth of the trophozoite in the duodenal area is stimulated by the presence of carbohydrates and bile. Adherence to the intestinal mucosa is achieved by the attachment of the ventral sucking disc, microtubule mediation, the contractile protein activity and possibly by a mannose binding lectin [6].
When the trophozoite moves through the colon, the cyst formation occurs, though the exact cause is not known. Children are more commonly affected than adults. The symptoms may be mild diarrhoea, flatulence, anorexia, abdominal cramps, foul smelling diarrhoea, steatorrhoea and the malabsorption syndrome. The biopsy of the jejunum shows the major finding of the shortening and blunting of the villi [7]. The other less common sites are the gall bladder and the bile ductal system. Stevens and Vermeire, in 1981, reported the detection of Giardia lamblia in bronchoalveolar lavage [8]. It has also been detected in the urinary tract [9].
The specimens that can be obtained to detect Giardia lamblia are:
Stool (most common)
Duodenal fluid (which is obtained by intubation)
Biopsy Specimen
Jejunal impression Smear and
the mucus which adheres to the distal end of the gelatin capsule in the String test.
The identification of the Giardia trophozoite or cyst is commonly done by
Wet Film – i) Saline wet mount preparation for the trophozoite and the cyst and ii) Iodine preparation to observe the cyst.
The staining methods which are used are the Iron-hematoxylin stain, the Trichrome stain and the Giemsa stain [5].
Direct Immunofluorescence – the Giardia cysts appear as oval, apple – green fluorescing forms which are 11-14 µm in diameter [10].
Electron Microscopy is not done routinely.
Giardial antigen in faeces is detected by -
Enzyme Linked Immunosorbant Assay (ELISA),
Countercurrent Immuno – Electrophoresis (CIE), and
the Immunochromatographic card test [5].
Molecular Methods: Polymerase Chain Reaction (PCR) [5].
Cultivation: A medium which comprises of a Chick embryo extract, Human serum, Hottinger’s digest, Hank’s solution and Yeast(Candida guillermondi) [11].
The main advantages of the methylene blue staining are: It is a single-step procedure and a permanent staining method. For the trophozoites which disintegrate rapidly, this method is beneficial, if we want to preserve the trophozoite structure for teaching purposes. This method is also economical and it takes less time. The methylene blue reagent is easily available in any clinical Microbiology laboratory. The method is quite useful for survey work. Only a stool smear needs to be prepared and fixed with methanol and on the next day, the smear can be stained and its reporting can be done.
The limitation of the methylene blue staining is that the Giardia cysts cannot be stained by this method. The other permanent staining methods like the Trichrome stain and the Iron-haematoxylene stain are costly and time consuming and they involve many steps, but both the Giardia trophozoites and cysts can be stained by these methods [5]. The Giardia cyst can retain its structure for many years, if the stool sample is stored in a 10% formalin solution.
Conclusion
Methylene blue staining is a simple staining method which can be used for detecting and preserving the Giardia trophozoite’s structure and the stained smears can be kept as a permanent record.
[1]. Hegner RW, The systematic relationship of Giardia lamblia Stiles, 1915 from man and Giardia agilis Kunstler, 1882 from the tadpole.American Journal of Epidemiology 1922 2(4):435( to search in 2011) [Google Scholar]
[2]. Nygard K, Schimmer B, Sobstad O, Walde A, Tveit I, Langeland N, A large community outbreak of waterborne Giardiasis – delayed detection in a non – endemic urban areaBMC Public Health 2006 6:141http://www.biomedcentral.com/1471-2458/6/141 [Google Scholar]
[3]. Mohan CR, Lehman DC, Manusetis G, Textbook of Diagnostic Microbiology 2007 3rd edNew Delhi IndiaElsevier [Google Scholar]
[4]. Lumsden WHR, Burns S, McMillan A Mackie, McCartney Practical Medical Microbiology 2006 14th ed.New Delhi IndiaChurchill Livingstone Elsevier [Google Scholar]
[5]. Garcia L S Topley, Wilson’s Microbiology and Microbial infections Parasitology, 2005 10th ed.Washington DC, USAHodder Arnold [Google Scholar]
[6]. Katelaris PH, Naeem A, Farthing MJG, Attachment of Giardia lamblia trophozoites to a cultured human intestinal cell lineGut 1995 37:512-18. [Google Scholar]
[7]. John DT, Petri WA, Markell Voge’s Medical Parasitology 2009 9th ed.Noida IndiaSaunders Elsevier [Google Scholar]
[8]. Stevens WJ, Vermeire PA, Giardia lamblia in bronchoalveolar lavage fluid.Thorax 1981 36:875 [Google Scholar]
[9]. Meyers JD, Kuharic HA, Holmes KK, Giardia lamblia infection in homosexual menBr. J. Vener. 1977 53:54-55. [Google Scholar]
[10]. Winn W, Allen S, Janda W, Koneman E, Procop G, Schreckenberger P, Koneman’s Color Atlas and Textbook of Diagnostic Microbiology 2006 6th ed.Philadelphia USALippincott’s Williams and Wilkins [Google Scholar]
[11]. Karapetyan A, In vitro cultivation of Giardia duodenalisThe J. of Parasito 1962 48(3):337-40. [Google Scholar]