Introduction
Periodontitis is a chronic inflammatory disease which is initiated by an infection of the oral microorganisms and it involves the humoral cellular characteristics of the host response. The periodontal disease is found to develop due to a series of interactions among the periodontotrophic herpes viruses, the periodontopathic bacteria and the host immune reactions [1]. HCMV is a herpes virus which has the ability to establish a lifelong infection in a host and its reactivation in the periodontal sites constitutes an important pathogenic event in periodontitis. A growing body of data sup-ports the concept that HCMV contributes to severe forms of periodontitis [2].
HCMV has been detected in saliva and GCF. The PCR based detection has proved to be a sensitive and a specific tool for the identification and the quantification of HCMV . In a study, a strong relationship between the presence of HCMV in the crevicular samples and the measurements of probing depth and the clinical attachment levels was observed [3,4,5].
Cervical cancer is a malignant cancer of the uterine cervix. Human papillomaviruses (HPVs) are important, but not sufficient in causing cervical cancer [6]. The search for the cofactors which are involved in the multistep oncogenic pathway has received much interest and HCMV was considered as a potential candidate. Recent evidence has indicated the frequent presence of the genomes and the antigens of HCMV in cancer of the cervix. Studies which have used highly sensitive PCRs have reported the presence of HCMV in cervical cancer [7].
Inflammatory conditions have been found to reactivate the latent HCMV and to cause oncomodulation. HCMV has been derived from cervical cancer biopsy specimens and cell cultures. The presence of a significantly higher level of antibodies to HCMV was observed in studies which were done on patients with carcinoma of the cervix. However, the available data on the presence of HCMV in cervical cancer are inconclusive [8].
Periodontal disease has been linked to many systemic diseases such as cardiovascular disease, pulmonary disease, low birth weight and more recently, cancer. The scientific rationale behind this proposed association is inflammation [9]. It is thought that a local infection such as that which occurs in periodontal disease may contribute to the establishment of a systemic inflammatory condition in genetically susceptible individuals, which is known as the ‘hyper inflammatory phenotype’, which potentially involves the increased production of inflammatory mediators and a breakdown of pathways which are responsible for an immune resolution [10,11].
Human Cytomegalovirus (HCMV) is one of the infectious organisms for which the available evidence for its involvement in inflammatory diseases is the strongest. Since inflammation plays a central role in the pathogenesis of HCMV, the current research is focussed on determining the role of HCMV in inflammatory diseases such as vascular diseases, autoimmune diseases and cancer [12].
Although there are several studies on the association of periodontal disease and various cancers, to date, to our knowledge, there are no reports on studies which were done on the association of periodontal disease and carcinoma of the cervix. Since HCMV was found to be one common denominator in periodontal disease and carcinoma of the cervix and since both the diseases presented as chronic inflammatory conditions, ours was a pilot study which was carried out to observe the role of HCMV in chronic periodontitis and in carcinoma of the cervix and to explore the hypothesis of a link between the two.
Material and Methods
Study Population
The study population consisted of the subjects who were being screened for carcinoma of the uterine cervix at the Bharat Hospital and Institute of Oncology, Mysore. Sixteen female subjects who were aged 35 to 65 years, who were diagnosed with carcinoma of the cervix were selected for the study. The non-availability of previous literature, the expenses which were involved and the availability of untreated cervical cancer patients limited the sample size to 16.
The sample subjects who were included in the study had no other systemic illnesses, they had not received any periodontal therapy or systemic antibiotics at least six months prior to their sampling and recording, and they had not received any treatment for carcinoma of the cervix. The patients who were medically compromised, those who were under a therapeutic regimen for carcinoma of the cervix and smokers were excluded from the study.
The investigation was performed in accordance to the requirements of the “Declaration of Helsinki” as was adopted by the 18th World Medical assembly in 1964 and revised in Edinburgh (2000).
The study protocol which was followed for the present study was approved by the Institutional Review Board (IRB) and the the JSS Dental college and Hospital, an affiliated institution of the JSS university, Mysore. An informed consent was obtained from all the subjects prior to the study after explaining the study procedures in detail to them.
The Clinical Evaluation and the Sampling Procedure
Sixteen subjects who were diagnosed as positive for carcinoma of the cervix were selected for the study. The patients who were selected were grouped as Stage I, II or III, based on the severity of the cancer. All the sixteen patients underwent a clinical evaluation for the periodontal conditions, based on the clinical parameters such as the plaque index (PI), gingival index (GI), probing depth (PD), and the clinical attachment Level (CAL). All the parameters were measured by using a Williams probe which was calibrated in millimetres. The measurements were taken at 4 sites per tooth on the entire dentition. Saliva, gingival crevicular fluid (GCF) and cervical biopsy samples were collected from all the patients for the HMCV detection.
Gingival Crevicular Fluid (GCF), Saliva and Cervical Biopsy Collection
The GCF was collected by using a micropipette. Briefly, prior to the GCF sample collection, the supragingival plaque was removed by using a sterile cotton pellet and the sites were isolated with cotton rolls. The GCF samples were collected from 4 of the deepest sites (5-7 mm) of the dentition in the patients with periodontitis. In the subjects without periodontitis, the samples were collected from 4 shallow sites (2-3mm) of the dentition. A sterile, 5 micron, micro capillary pipette was inserted into the sulcus and the GCF was collected and transferred into separate sterile plastic vials. Then the saliva samples were collected. The patients were asked to spit into sterile disposable cups and 2 ml of their saliva was transferred into the sterile vials. The cervical biopsies were obtained by using a speculum. The samples which were collected were tested for the presence of HCMV by the Polymerase Chain Reaction (PCR) technology.
DNA Extraction and the PCR Procedures
The Deoxyribose Nucleic Acid (DNA) from saliva, GCF or the cervical biopsy samples was extracted. Briefly, the samples were lysed in Tris-ethylene diamine tetra acetic acid (EDTA) buffer, 40 µl of 20% Sodium Dodecyl Sulphate (SDS) and 100µg of Proteinase –K by incubating at 55ºC for one hour, with occasional mixing. Equal volumes of Phenol-Chloroform-Isoamyl alcohol (PCI mix in 25:24:1 ratio) were added and the samples were centrifuged at 12,000 x g for 5 minutes. The upper aqueous phase was collected without disturbing the protein layer which was present at the interphase layer. The aqueous phase was subjected to PCR treatment for two more times. Then, 30µl of 3M sodium acetate and equal volumes of absolute ethanol were added and the samples were incubated at -20°C overnight. The samples were centrifuged for 10 minutes at 12000 x g and the supernatant was discarded without disturbing the pellet. The pellet was washed with 70% ethanol and allowed to dry briefly at 37°C. Finally, 50µl of sterile distilled water was added and it was incubated at 60°C briefly for the easy suspension of the DNA.
PCR was carried out in an Eppendorf Master Gradient thermal cycler. Specific primers were constructed for the amplification of the HCMV viral DNA. The PCR conditions were optimized for the efficient amplification of the 134 base pair HCMV specific fragment. The following conditions were found to be optimal for detecting HCMV from the clinical samples. The reaction was set up in a final volume of 20µl: 2µl PCR buffer (10x concentration), 1.6µl Magnesium chloride (25 mM stock), 1.0µl dNTPs (2mM stock), 10-50 ng DNA, 0.2µl (1 Unit) Taq polymerase, and sterile distilled water to make up the volume to 20 µl. The initial denaturation was at 94°C for 4 minutes, followed by 30 cycles of denaturation at 94°C for 1 min, annealing at 55°C for 30 seconds, and extension at 72°C for 60 seconds.
Gel Electrophoresis
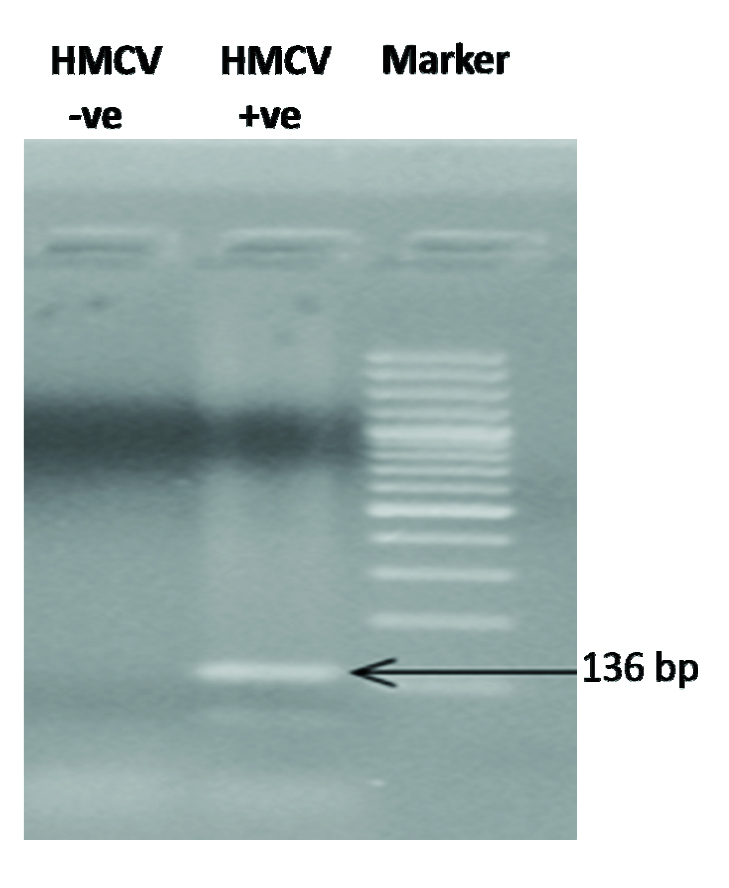
The PCR amplification products were separated by electrophoresis on a 1% agarose gel and the 136bp band which was specific for HCMV was visualised under ultraviolet light and it was analyzed qualitatively [Table/Fig-1].
Statistical Analysis
The descriptive statistics were calculated as mean ± standard error (SE) for the continuous variables and as frequencies (percentages) for the categorical variables. The comparison of the groups was performed by using the Chi Square (χ2) test or the t tests, as was appropriate. The frequency (percentage) of the patients who were positive or negative for HCMV in the cervical biopsies, saliva, and GCF samples were calculated and compared by χ2 analysis. The mean values of the clinical parameters such as the plaque index (PI), gingival index (GI), probing depth (PD), and the clinical attachment level (CAL) were compared between the HCMV positive and the HCMV negative patients (in saliva, GCF or cervical biopsies) by using the t-test. The difference at p≤0.05 was considered as statistically significant.
Results
The results of the study indicated an association of HCMV and chronic periodontitis, and an association of HCMV and carcinoma of the cervix. But an association of chronic periodontitis and cervical cancer could not be elucidated.
The GCF, saliva, and the cervical biopsies which were harvested from the sixteen carcinoma cervix patients with chronic periodontitis were analyzed for the HCMV DNA by using the nested PCR technology and the presence of the HCMV specific PCR product (136 bp) was determined by gel electrophoresis, which indicated as to which patients were positive for HCMV [Table/Fig-1], [Table/Fig-2].
Human Cytomegalovirus (HMCV) DNA in saliva, gingival crevicular fluid or cervical biopsy specimens were amplified using HMCV specific primers by polymerase chain reaction (PCR) techonology. The PCR products were separated by electrophoaresis on 1% agarose gel, stained with ethidium bromide, and visualized under UV source for 136bp HMCV specific PCR Product; a representative HCMV positive and negative sample are shown in the figure.
Carcinoma cervix patients positive for HCMV in cervical biopsy, saliva and gingival crevicular fluid.
| Stage of cancer | Number of patients percentage | HCMV in Cervix | HCMV in Saliva | HCMV in GCF |
|---|
| – | + | – | + | – | + |
|---|
| I | Number | 3 | 0 | 2 | 1 | 2 | 1 |
| Percentage | 18.75 | 0 | 12.25 | 16.7 | 66.7 | 33.3 |
| II | Number | 1 | 8 | 6 | 3 | 2 | 7 |
| Percentage | 6.25 | 50 | 60 | 50 | 22.2 | 77.8 |
| III | Number | 1 | 3 | 2 | 2 | 0 | 4 |
| Percentage | 6.25 | 18.75 | 20 | 33.3 | 0 | 100 |
| Total | Patients | 5 | 11 | 10 | 6 | 4 | 12 |
| Percentage | 31.25 | 68.75 | 62.5 | 37.25 | 25 | 75 |
Statistical comparisons (stages I, II, and III together):
HMCV in cervix +ve Vs –ve (P= 0.015); HMCV in saliva +ve Vs –ve (P= 0.837); HMCV in saliva +ve Vs –ve (P= 0.12); P≤0.05 was considered significant
Of the 16 patients who were diagnosed to be in different stages of carcinoma of the cervix, eleven (68.75%) were found to be positive for HCMV in the cervical biopsies, Six (37.5%) were positive for HCMV in saliva and twelve (75%) out of the 16 patients were positive for HCMV in GCF [Table/Fig-2].
The clinical parameter (PI, GI, PD, CAL) scores are shown in [Table/Fig-3]. The plaque index (P= 0.027), gingival index (0.187), probing depth (P=0.049) and the clinical attachment level (P=0.039) were significantly higher in the sites which were GCF positive for HCMV as compared to those in the sites which were GCF negative for HCMV [Table/Fig-3],[Table/Fig-4].
Mean values of clinical parameters and their comparisons between patients with HCMV (+ve) and HCMV (-v e) Gingival Crevicular Fluid in one or more sites.
p-value: PI=0.027, GI= 0.187, PD =0.049, 0.039
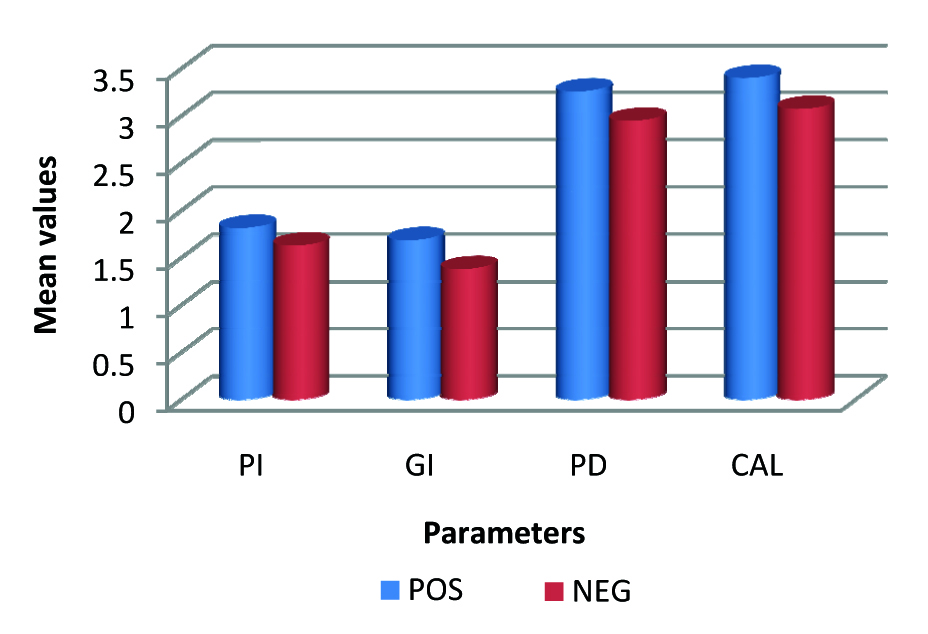
Mean values of clinical parameters and their comparisons between patients with HCMV (+ve) and HCMV (-ve) Gingival Crevicular Fluid in one or more sites.
| Parameters | Sites HCMV +/- | N | Mean | t | P Value |
|---|
| PI | – | 29 | 1.38 | -2.265 | 0.027 |
| + | 35 | 1.68 |
| GI | – | 29 | 1.62 | -1.335 | 0.187 |
| + | 35 | 1.81 |
| PD | – | 29 | 2.94 | -2.004 | 0.049 |
| + | 35 | 3.25 |
| CAL | – | 29 | 3.07 | -2.110 | 0.039 |
| + | 35 | 3.40 |
PI-Plaque Index; GI-Gingival Index; PD-Probing Depth; CAL-Clinical attachment Level; N-Number of Patients . + = positive, - = negative.
P≤0.05 was considered statistically significant.
Out of the total 16 carcinoma cervix patients who were studied, only 4 (25%) patients were positive for HMCV in both saliva and the cervical biopsies [Table/Fig-5]. There was no significant difference between the patients who tested HCMV positive and negative in saliva (p=0.889) or in the cervical biopsies, as was determined by χ2 analysis. Also, there was no significant correlation with the clinical parameters.
HCMV detected in saliva samples versus HCMV detected in Cervical biopsy samples.
| Saliva HCMV +/- | Count | Cervix- | HCMV +/- |
|---|
| Percentage | + | - |
|---|
| + | 6 | 4 | 2 |
| 37.5 | 66.7 | 33.3 |
| – | 10 | 7 | 3 |
| 62.5 | 70 | 30 |
p value: 0.889; HCMV detected in saliva and Cervical biopsy in 4 out of 16 patients = 25%.
Out of the 16 patients, 9 tested positive for HCMV in both GCF and the cervical biopsies. HCMV was not detected in any site in 4 patients [Table/Fig-6]. There was no significant difference between the patients who tested HCMV positive and negative in GCF (p=0.97) or in the cervical biopsies, as was determined by χ2 analysis.
HCMV detected in GCF samples versus HCMV detected in Cervical biopsy samples.
| GCF HCMV +/- | Count | Cervix +/– | HCMV +/– |
|---|
| Percentage |
|---|
| + | 12 | 9 | 3 |
| 66.7% | 66.7 | 33.3 |
| – | 4 | 0 | 4 |
| 33.3% | 0 | 100 |
p-value : 0.97; HCMV detected in GCF and Cervical biopsy in 9 out of 16 patients= 56%.
Discussion
Periodontitis and carcinoma of the cervix are both chronic inflammatory conditions with multifactorial aetiologies. Further, both the disease entities have been found to harbour the human cytomegalovirus. Whether the virus plays a role as a cofactor in the disease progression or whether it is just a by-stander to other causative factors, still remains an enigma.
HCMV and periodontal disease
The human cytomegalovirus is the most immunodominant antigen which is encountered by the immune system. The virus remains latent in an infected host and its reactivation occurs by immune activation. The immune activation occurs mostly in the inflammed tissues i.e. the tissues which are targeted by the immune system [12]. The periodontal disease sites are the areas of chronic low grade inflammation. HCMV has been detected in the subgingival areas and these have been found to exert a periodontopathic potential [13]. Significant associations among HCMV, P. gingivalis and progressive periodontitis have been demonstrated, which have implied that HCMV and P. gingivalis may serve as co factors in the periodontal breakdown [14]. HCMV has been detected in saliva and in the periodontal pockets by using the polymerase chain reaction (PCR) more frequently in the periodontitis lesions than in the periodontally healthy sites [2,3]. Hence in this study, the PCR technology was used.
Sayguan et al. provided a compelling evidence on periodontitis as a source for salivary HCMV and suggested that the periodontal therapy could potentially decrease the salivary counts and the transmission of HCMV [5]. However, in the present study, only 37.7% patients tested positive for HCMV in saliva and the comparisons of the clinical parameters between the patients who were positive for HCMV in saliva and the patients who were negative for HCMV in saliva were not significant (P≥0.05).
In the present study, out of the 16 carcinoma cervix patients with chronic periodontitis, HCMV was detected in the GCF of 12 (75%) patients and in the saliva of 6 (37.5%) patients. The presence of the virus in the GCF of the sampled sites was associated with significantly higher measurements of the probing depth and the clinical attachment loss in comparison to the patients with HCMV negative GCF. This is in accordance with a study which confirmed the frequent presence of HCMV in the crevicular samples of chronic periodontitis lesions and which suggested a strong relationship between the presence of HCMV in the subgingival areas and the measurements of probing depth and probing attachment loss, as the virus was detected more often in the deep pockets than in the shallow areas [4]. Overall, these findings were suggestive of a possible association between the presence of HCMV and chronic periodontitis.
Similarly, a growing body of data has supported the concept that HCMV contributes to periodontal disease [4]. It was hypothesised that the HCMV infection of the periodontium could alter the immune control of the resident microorganisms and that this could be important in the multistage pathogenesis of periodon-titis which involved viral activation, the periodontopathogenic bacteria and the host immune response. HCMV was found to exist as a co infection in association with the periodontopathogenic bacteria, thus decreasing the host resistance against the subgingival colonization and the multiplication of the periodontal pathogens [2].
Any data which had implicated HCMV to cause periodontitis which was independent of the periodontopathic bacteria was unavailable [12]. Our study, which was coherent with the available literature, suggested that HCMV acted either as a co factor in periodontal disease or that it triggered its relapse. Further studies and the use of real time PCR for quantifying the virus are required. Comparison of the levels of the cytokines and the chemokines in the HCMV detected and the undetected sites needs further research.
HCMV and Carcinoma of the Cervix
HCMV has been studied as a cancer associated virus and it has been isolated from various cancers which include cervical cancer. In various studies, HCMV had been isolated from cervical cancer biopsy specimens by the PCR technique and culture [8]. Its role in carcinoma of the cervix since human papilloma virus is found to be important but not sufficient to cause cervical cancer. [7] In the present study, the PCR method was employed and HCMV was detected in the cervical biopsy specimens in 11 (68.75%) out of the 16 patients. This was in accordance with the findings of the studies which were conducted by Huang, Fletcher et al., who detected the HCMV DNA in the cervical cancer specimens. Further, histological and seroepidemiologic studies have provided evidence of an association between HCMV and cervical cancer [8].
Due to the ubiquitous distribution of HCMV and its high seroconversion rates, an aetiological association between the HCMV infection and human cancer has been difficult to establish. Some investigators have found significantly higher levels of antibodies to HCMV in the patients with HCMV than in the controls, while others have found no such correlation. Although HCMV has been detected in cervical cancer biopsy specimens, seroepidemiologic studies which have linked the HCMV infection to cervical cancer have yielded conflicting results.
The detection of the DNAs of several other viruses, especially the Human Papilloma Virus-2 (HPV-2) along with HCMV in cervical cancer biopsies, points towards the possibility of synergistic interactions among these viruses in the infected cell, thus leading to the development of cervical cancer [8]. In our study, HCMV was detected in the cervical biopsies of 11 patients. But the determination of the serum antibody levels to HCMV in these patients was not attempted. Also, confounders like obesity, nutrition, stress, socioeconomic status and immunity made this assessment more complex. These factors were not standardized in our study. Hence, with the available data, the role of HCMV in carcinoma of the cervix could indicate its role as a by-stander rather than a co factor for oncogenesis in cervical cancer.
Periodontitis and Cancer
Michaud has extensively researched the association of period-ontal disease and cancer risk and he has conclusively suggested plausible biological mechanisms, such as systemic inflammation and/or the increased concentrations of carcinogenic compounds as a result of the presence of bacteria in the oral cavity of those with periodontal diseases to be involved in the development of cancer [10]. The hypothesis which has linked periodontal disease and cancer is based on the fact that periodontitis results in a low grade systemic inflammation with increased levels of circulating inflam-matory markers i.e. cytokines, leukocytes, prostanoids and acute phase proteins [11,15]. Hence, the assessment of an association between periodontitis and cancer may require the assessment of the systemic inflammatory markers. These parameters could not be assessed in the present study due to economic constraints.
Conclusion
The results of the present study were suggestive of a possible association between the HCMV occurrence in chronic periodontitis and carcinoma of the cervix. The presence of HCMV in the GCF of the sampled sites and its correlation with the measurements of probing depth and the clinical attachment level were suggestive of the role of HCMV as a possible co-factor in periodontitis. The detection of HCMV in the cervical biopsies was suggestive of its presence as a by stander to other causative factors. The present study, with its available data, failed to indicate a possible association between cervical cancer and periodontitis. As the literature is sparse in this regards, further studies that assess in more detail the potential mechanisms for the association of carcinoma of the cervix and periodontal disease are warranted, to enable the development of rational treatment strategies.
Limitations of the Study
Need for a larger sample size and a longer duration of the study
The gingival biopsies can be compared with the cervical biopsies for the presence of the virus
Systemic inflammatory markers- cytokines and antibody titres could be included
The use of real time PCR for the quantification of the virus would be more useful
The confounding factors were not standardized
Future Perspective
The results of the present exploratory study prompt further research to establish the role of HCMV in periodontitis, and to determine a definitive causal relationship between periodontitis and cervical cancer. Understanding the significance of HCMV in these diseases may have important therapeutic implications. Quantification of an association between chronic periodontitis and cervical cancer would have substantial implications for the public health in terms of their prevention and early diagnosis. Further, the potential of the periodontal therapy to decrease the salivary counts of HCMV may help in diminishing its transmission. The positive outcome of the periodontal treatment would probably benefit the circulatory system and decrease the risk of systemic complications and cancer.
Clinical Relevance
Periodontal disease, with its broad prevalence globally, remains the single most common cause of tooth loss. Worldwide, cervical cancer is the fifth most common cancer in women. Periodontitis and carcinoma of the cervix are both chronic inflammatory conditions with multifactorial aetiologies. Further, both the disease entities have been found to harbour the human cytomegalovirus. Chronic inflammation and co-infection with HCMV can be significant contributory factors. Whether the virus plays a role as a cofactor in the disease progression or whether it is just a by-stander to other causative factors, still remains an enigma.
If an association between the occurrence of the virus in periodontal lesions and carcinoma of the cervix is explored, it would have substantial implications for the public health in terms of prevention and early diagnosis. This will provide an impetus to further research on a larger population and will enable the development of rational treatment strategies.
Statistical comparisons (stages I, II, and III together):HMCV in cervix +ve Vs –ve (P= 0.015); HMCV in saliva +ve Vs –ve (P= 0.837); HMCV in saliva +ve Vs –ve (P= 0.12); P≤0.05 was considered significant
PI-Plaque Index; GI-Gingival Index; PD-Probing Depth; CAL-Clinical attachment Level; N-Number of Patients . + = positive, - = negative.
P≤0.05 was considered statistically significant.
p value: 0.889; HCMV detected in saliva and Cervical biopsy in 4 out of 16 patients = 25%.
p-value : 0.97; HCMV detected in GCF and Cervical biopsy in 9 out of 16 patients= 56%.