Tuberculosis is a major cause of morbidity and mortality in the developing countries, accounting for two billion infected cases and 1.7 million deaths which were attributed to it in 2006, as per the WHO. Cancer was the leading cause of death, next only to coronary artery disease, with 11.3 million new cases and 7.9 million deaths in 2007. The combination of these two deadly diseases poses significant diagnostic and therapeutic challenges to the clinicians and the pathologists. The relationship of tuberculosis and malignancy can be viewed in two ways: tuberculosis can be a risk factor for cancer or tuberculosis and malignancy can coexist in the same biopsy or in the same patient. An early and an accurate diagnosis is a must for planning the appropriate management. We are describing a very rare case of coexistent extra adrenal pheochromocytoma and extrapulmonary tuberculosis in a single patient, which was diagnosed by fine needle aspiration cytology, with a brief review of the literature.
Introduction
Pheochromocytoma is a rare tumour which arises from the chromaffin tissue in the adrenal medulla. Extra-adrenal pheochromocytomas (EAPs) account for 10% of the cases, which present as thoracic or retroperitoneal masses in paravertebral locations [1,2]. It is extremely desirable for a clinician to make an accurate preoperative diagnosis, to prevent any untoward reaction or a fatality at surgery. Pharmacological tests can be used in the cases when they occur in the adrenal gland with a classic history of a paroxysmal attack of hypertension and headache [3]. Though it has been traditionally contraindicated, fine needle aspiration cytology (FNAC) has been used safely in cases of EAP for a preoperative diagnosis, especially in the unsuspected cases [4,5].
Very rarely, pheochromocytoma occurs concurrently with tuberculosis. A clinical overlap between these two entities may mislead the clinician, resulting in a delayed diagnosis [4]. Tuberculosis (TB) may retard the response to the treatment of pheochromocytoma. Likewise, the institution of chemotherapy may lead to the worsening of the underlying TB. The awareness on the coexistence of these two conditions is highly significant, since the treatment of both needs to be rationalized.
Case Report
A 55 year female presented with a mass per abdomen of three months duration, with a history of fever, tiredness and palpitation. She was detected to have hypertension six months back and was on antihypertensive drugs since then. On general examination, her pulse was found to be 102 beats/minute and her blood pressure was 200/100 mm of Hg. She had marked pallor and a palpable, single, 2 × 2 cm posterior cervical lymph node. A mass which was present in the right lumbar region was palpable. The laboratory investigations revealed that the haemoglobin was 3 gm/dl and that the ESR was 30 mm at end of one hour. The serum electrolytes and the kidney and the liver function tests were normal. Ultrasonography showed a heterogeneous mass lesion in the right lumbar region.
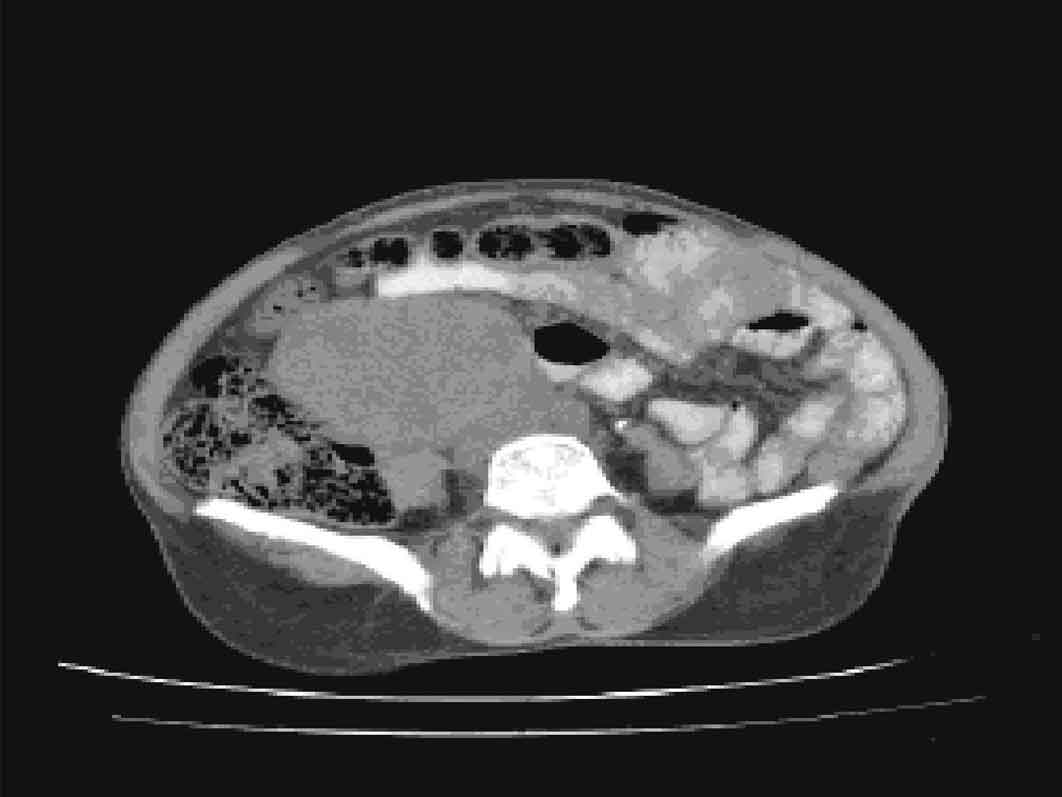
A computed tomography (CT) scan showed a well-defined hyper dense mass lesion which measured 4 × 4 cm in the right lumbar region, above the bifurcation of the aorta [Table/Fig-1].
Axial C.T image with oral contrast showing well defined mass lesion with areas of necrosis causing mild compression of inferior venacava.
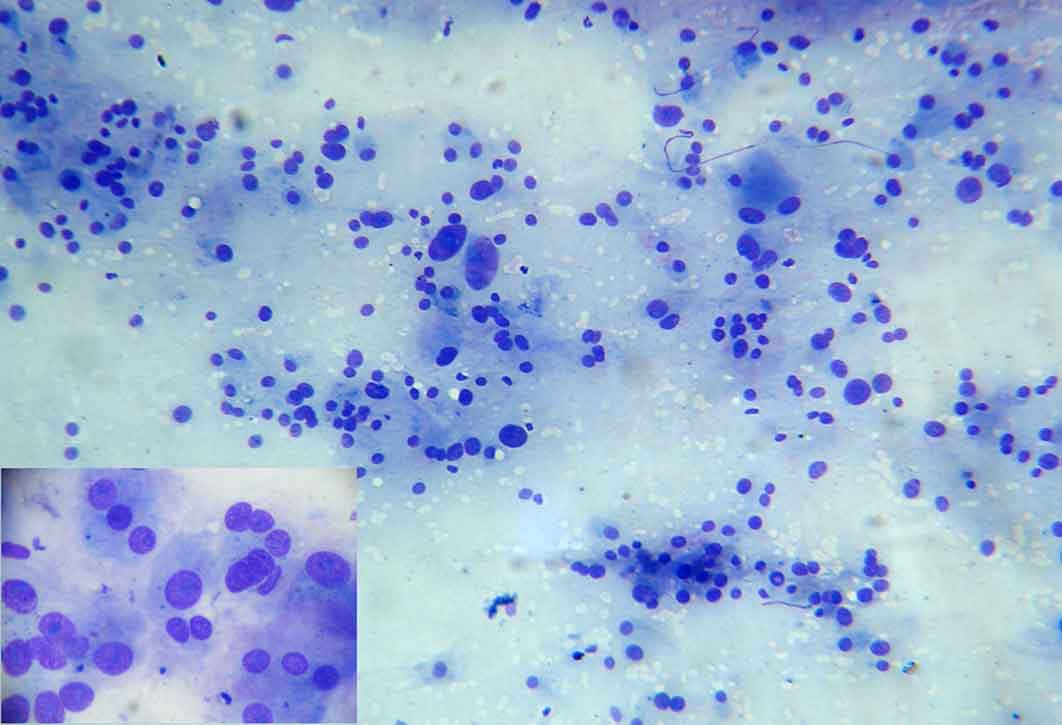
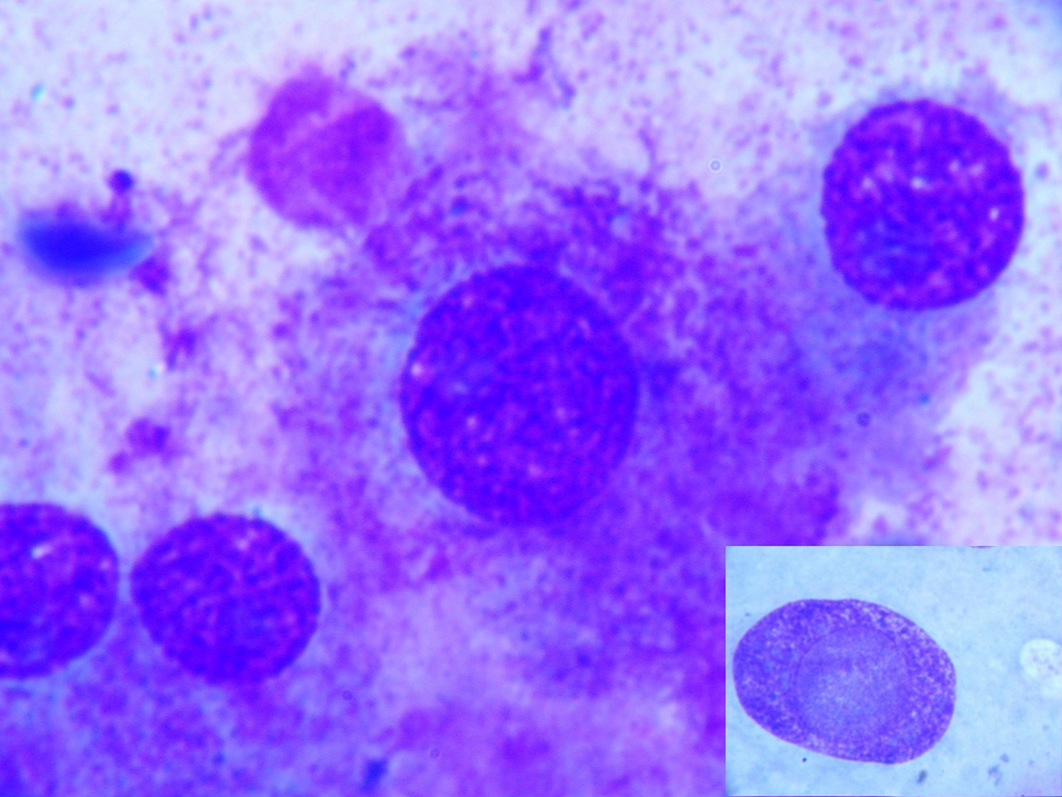
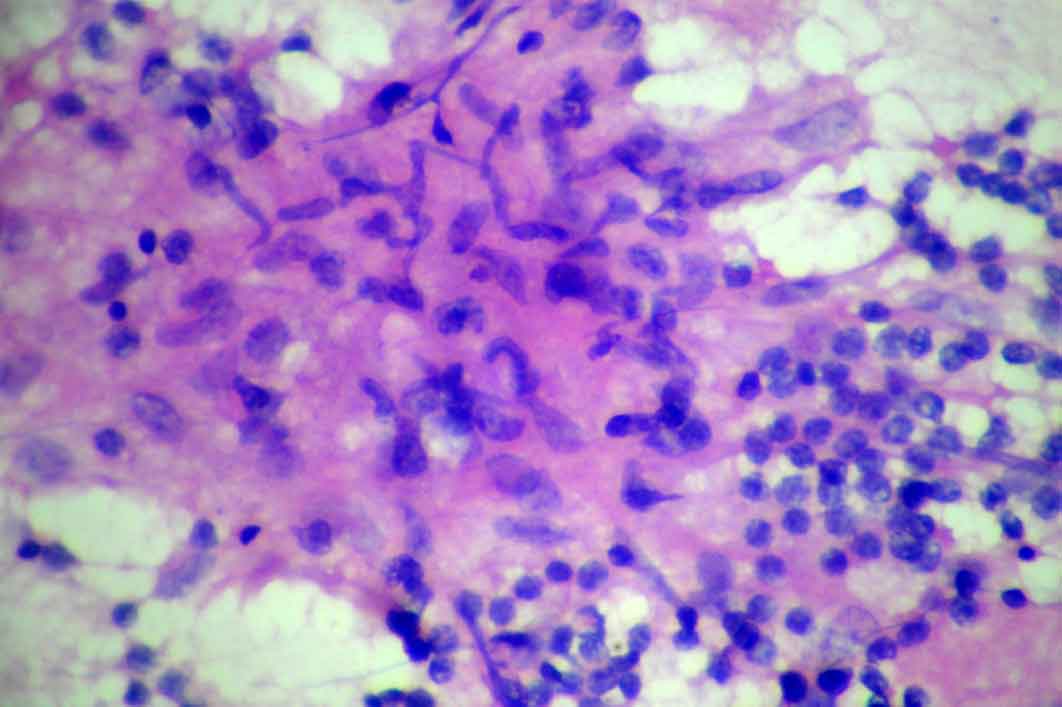
An informed written consent was obtained from the patient after explaining to her, the dangers of performing the FNAC in that setting, in her language. An FNAC was done under ultrasound guidance by using a 21 gauge needle. The slides were fixed in 90% alcohol for hematoxylin and eosin staining and they were air dried for the May Grunwald Giemsa staining. The smears showed polygonal cells which were arranged predominantly in a microacinar pattern, with many cells showing anisonucleosis, [Table/Fig-2]. The individual cells showed an abundant amount of eosinophilic granular cytoplasm, nuclei with prominent nucleoli, binucleation and multinucleation. Intra cytoplasmic and intranuclear inclusions were seen [Table/Fig-3]. The background showed the characteristic Nissl’s substance. A possible diagnosis of pheochromocytoma was made. The urinary catecholamine level was 16 ng/dl. The cytology of the cervical lymph nodes showed the features of tuberculous lymphadenitis [Table/Fig-4]. Acid fast staining was positive for the tubercle bacilli. The culture of the FNAC specimen showed that the morphology of the isolates resembled that of Mycobacterium tuberculosis. Chest X ray did not show any evidence of pulmonary tuberculosis. The sputum for acid fast bacilli test as well as the culture was negative. After the control of the hypertension, the surgical excision of the tumour was done, which confirmed the diagnosis of benign phaechromocytoma on histopathology. The patient was started on antituberculous therapy, category 1, of the Revised National Tuberculosis Control Programme. The patient is on regular followup and is doing well after 6 months.
Photomicrograph showing cells in loose clusters and microacinar pattern with anisonucleosis[May GrunwaldGiemsa(MGG) x 40]. Inset shows a microacinar pattern [MGG x 100].
Photomicrograph showing intracytoplasmiceosinophilic granules Inset shows intranuclear inclusion. [MGG x 400].
Cytology smears from cervical lymph node showing epithelioid cells in syncytial clusters admixed with lymphocytes.
Discussion
Pheochromocytoma is a rare tumour which accounts for 0.1% of the hypertensive cases [1]. EAP accounts for 10% of the pheochromocytoma cases and it presents as soft tissue mass lesion which runs parallel along the entire length of the abdominal aorta [2]. The most common sites for EAP include the paraadrenal area, followed by the organ of Zuckerkandel at the aortic bifurcation, the chest, the inferior mesenteric artery, over left common iliac artery, the bladder wall, and the celiac plexus, the superior mesenteric artery, the renal vessels, over right iliac artery, beneath the diaphragm and around the left ureter, in the decreasing order of frequency [6].
The patients are usually adults who present with the early and the classic symptoms of headache, palpitation and sweating. It is more likely for the clinician to elicit a history of an attack of hypertension than to observe it. At times, even the history is not available, especially in cases of a sustained hypertension [3]. An abdominal mass and pain, which are commonly seen in the late stages, however, may at times be the first presentations and in such cases, usually, the diagnosis is delayed by up to three years [7].
Traditionally, FNAC has been contraindicated in the diagnosis of pheochromocytoma due to the untoward reactions and its fatality. However, when it is used in the unsuspected cases of EAP which present as abdominal masses, no complication is noted [4,5]. The cytological diagnosis of pheochromocytoma has certain limitations. Gong et.al., in a report on two cases of EAP which were diagnosed by FNAC, while describing the pitfalls, have eloquently elucidated the clues for the correct diagnosis at cytology [4]. A microacinar formation may at times be misinterpreted as an adenocarcinoma. The dense eosinophilic cytoplasm may be suggestive of a squamous differentiation. However, like any other endocrine neoplasm, a marked pleomorphism and prominent nucleoli, binucleation, multinucleation and an intracytoplasmic and an intranuclear inclusion with a background which shows the pink eosinophilic Nissl’s substance may aid in arriving at a correct diagnosis [4,5].
The different modalities for the diagnosis of pheochromocytoma include pharmacological tests, radiology which includes ultrasound, CT, metaiodobenzylguanidine (MIBG) scan, FNAC and biochemical tests. CT scan is useful for localizing and assessing the extension of the tumour. Urine catecholamines and their metabolites are sensitive tests both in the diagnosis and the follow up of pheochromocytomas [8].
Bayle, in 1810, first stated that the coexistence of tuberculosis and malignancy in the lung was definitely occurring more commonly than it would occur by chance [9]. Since then, the association of tuberculosis and malignancy has been investigated extensively. In a large review which was written by Falgas et.al., the authors have put forth three different types of associations between TB and malignancy: i) the development of cancer on the background of a previous tuberculous infection, ii) the concurrent existence of TB and malignancy in the same patient(s) or clinical specimen(s), and iii) the diagnostic challenges which arise from the multifaceted presentations of these two disorders [10].
The common malignancies which coexist with TB include lung cancer, haematological malignancies which include non-Hodgkin’s and Hodgkin’s lymphomas, chronic myeloid leukaemia, breast cancer, gastrointestinal tract malignancies, endometrial carcinomas, fallopian tube carcinomas and rarely, thymic carcinomas [10].
There are only two case reports on the concomitant occurrence of TB and pheochromocytoma. In one case which was reviewed by Grace and Walter, an intrathroracic pheochromocytoma was found to be associated with pulmonary TB [3]. In another case which was reported by Toure et.al., a multifocal extrapulmonary TB was associated with an adrenal pheochromocytoma [11]. As has been depicted in the above cases, a clinical overlap and the misleading manifestations of the two diseases could render the diagnosis challenging and either could be missed.
Though many speculations have been made regarding the concurrent occurrence of TB in malignancy, the exact mechanism has yet to be elucidated. Much weight has been given to the postulate that the immunosuppression which is caused by a local or a systemic effect of malignancy might reactivate the preexisting tuberculous lesion or that it may result in the acquisition of a new primary infection [10].
The diagnosis of a coexisting pheochromocytoma and TB is not only of academic interest, but it has several clinical implications. The pheochromocytoma may hinder the treatment of the tuberculosis. In the case which was reported by Grace and Walter, the patient responded to the antituberculous therapy only after the surgical removal of the pheochromocytoma [3].
The presence of a palpable lymph node which is caused by tuberculosis may lead to an over staging in the TNM system [12]. The symptoms of TB may be mistakenly attributed by the treating clinician to a complication of the chemotherapy or to a worsening of the underlying disease.
Conclusion
The clinician and the pathologist must be aware that pheochromocytoma and tuberculosis may coexist and that this may pose a diagnostic challenge due to the overlapping clinical manifestation, especially in a country with a high prevalence of TB.
FNAC is an easy, safe and a cost effective test in the diagnosis of pheochromocytoma, in a well-equipped hospital, as this will help in the management of the hypertensive crisis if there is any.
A high degree of suspicion, careful attention to the cytology and the appropriate biochemical markers aid in making a correct diagnosis.
[1]. Goldfarb DA, Novick AC, Bravo EL, Straffon RA, Montie JE, Kay R, An experience with extra adrenal pheochromocytornaJ Urol 1989 142:931-6. [Google Scholar]
[2]. Whalen K, Althausen AF, Daniels GH, Extra-adrenalpheochromocytomaJ Urol 1992 147:1-10. [Google Scholar]
[3]. Grace MR, Walter FK, Evaluation of pharmacologic tests as aids in the diagnosis of pheochromocytomas: with the report of a case of pheochromocytoma and tuberculosisDis Chest 1957 32:295-304. [Google Scholar]
[4]. Gong Y, DeFrias DV, Nayar R, The pitfalls in the fine needle aspiration cytology of an extraadrenalparaganglioma – a report of 2 casesActa Cytol 2003 47:1082-6. [Google Scholar]
[5]. Rangaswamy M, Sandeep PK, Asha M, GV Manjunath GV, The CT-guided fine needle aspiration cytology diagnosis of an extra-adrenal pheochromocytomaJ Cytol 2010 27:26-8. [Google Scholar]
[6]. Atiyeh BA, Barakat AJ, Abumrad NN, Extra-adrenal pheochromocytomaJournal of Nephrology 1997 10:25-9. [Google Scholar]
[7]. Mannelli M, Ianni L, Cilotti A, Conti A, Pheochromocytoma in Italy: a multicentric retrospective studyEur J Endocrinol 1999 141:619-24. [Google Scholar]
[8]. Sherif L., Hegde R., Shetty K., Gurumurthy T., Jain P., The anesthetic management of a rare case of an extra adrenal pheochromocytoma- A case reportThe Internet Journal of Anesthesiology 2009 22(1) [Google Scholar]
[9]. Patel KC, Shah DP, Sheth SM, Kamat SR, The association between tuberculosis with malignancyJ Postgrad Med 1977 23:193-6. [Google Scholar]
[10]. Falagas ME, Kouranos VD, Athanassa Z, Opterides PK, Tuberculosis and malignancyQ J Med 2010 103:461-87. [Google Scholar]
[11]. Toure P.S., Elfajri S., Diop M., Leye Y.M., Leye A, Diop M.M., Ka M., The metastases of pheochromocytoma or multifocal tuberculosis? The difficulty in the diagnosis; A case reportThe Internet Journal of Endocrinology 2011 6(2) [Google Scholar]
[12]. Tulasi NR, Raju PC, Damodaran V, Radhika TS, A spectrum of coexistent tuberculosis and carcinoma in the breast and the axillary lymph nodes: a report of five casesBreast 2006 15:437-9. [Google Scholar]