Pseudosarcomatous Myofibroblastic Tumour of the Urinary Bladder: A Case Report
K. Chandramouleeswari1, S. Anita2, B. Shivali3
1 Associate Professor of Pathology, Chengelpet Medical college. Consultant pathologist, Lister Metropolis, Chennai, India
2 Chief of Laboratory Services, Lister Metropolis Labortaory, Chennai. India
3 Junior Pathologist, Lister Metropolis Labortaory, Chennai. India
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. K. Chandramouleeswari, Associate Professor of Pathology, Chengelpet Medical college. Consultant pathologist, Lister Metropolis, Chennai, India.
E-mail: chandrakathir@yahoo.com
A pseudosarcomatous myofibroblastic proliferation is an unusual and a rare benign lesion which arises from the bladder submucosal stroma and is easily mistaken for a malignant neoplasm, clinically, radiologically and histologically. By definition, the tumour is composed of a dominant spindle cell proliferation with a variable inflammatory component. These spindle cells are now known to be myofibroblasts and this is the reason for the current designation for this disease. The term ‘inflammatory’ may not be applicable to all the tumours, since some investigators have demonstrated the presence of chromosomal abnormalities and have documented cases which showed recurrence, thus supporting the theory that at least some of these tumours were true neoplasms.
Non-epithelial tumours account for 2–5% of all the primary urinary bladder neoplasms, with the most common types being rhabdomyosarcoma in patients under the age of 10 years and leiomyosarcoma in adults. A pseudosarcomatous myofibroblastic tumour is a nonepithelial lesion that follows a benign indolent course and a conservative management has been reported as the treatment of choice. Herein, we are reporting a case of a pseudosarcomatous myofibroblastic tumour which was mistaken for a sarcoma clinically and radiologically and which was proved as a pseudosarcomatous inflammatory myofibroblastic tumour by histopathology and immunohistochemistry.
Urinary bladder, Pseudotumour, Pseudosarcomatous myofibroblastic proliferation, Inflammatory pseudotumour
Case REPORT
A 17-year-old female presented with a sharp, lower abdominal pain with the completion of each urination and haematuria. She gave no history of night sweats or fever or urinary tract infections, trauma, instrumentation or any other urological problems.
An ultrasound study of the kidneys and the urinary bladder revealed a broad-based polypoid mass (7 ×4 ×3.2 cm) which was located in the right posterolateral wall of the bladder. Computerized tomography (CT) confirmed the presence of a solid mass which was infiltrating the postero lateral bladder wall and it demonstrated neither perivesical invasion nor pelvic lymphadenopathy. The patient subsequently underwent a cystoscopic biopsy of the lesion. The histologic examination of the excised mass displayed a cellular population of spindle-shaped cells with abundant eosinophilic cytoplasmic processes. The cells were haphazardly arranged, forming fascicles at the focal areas.
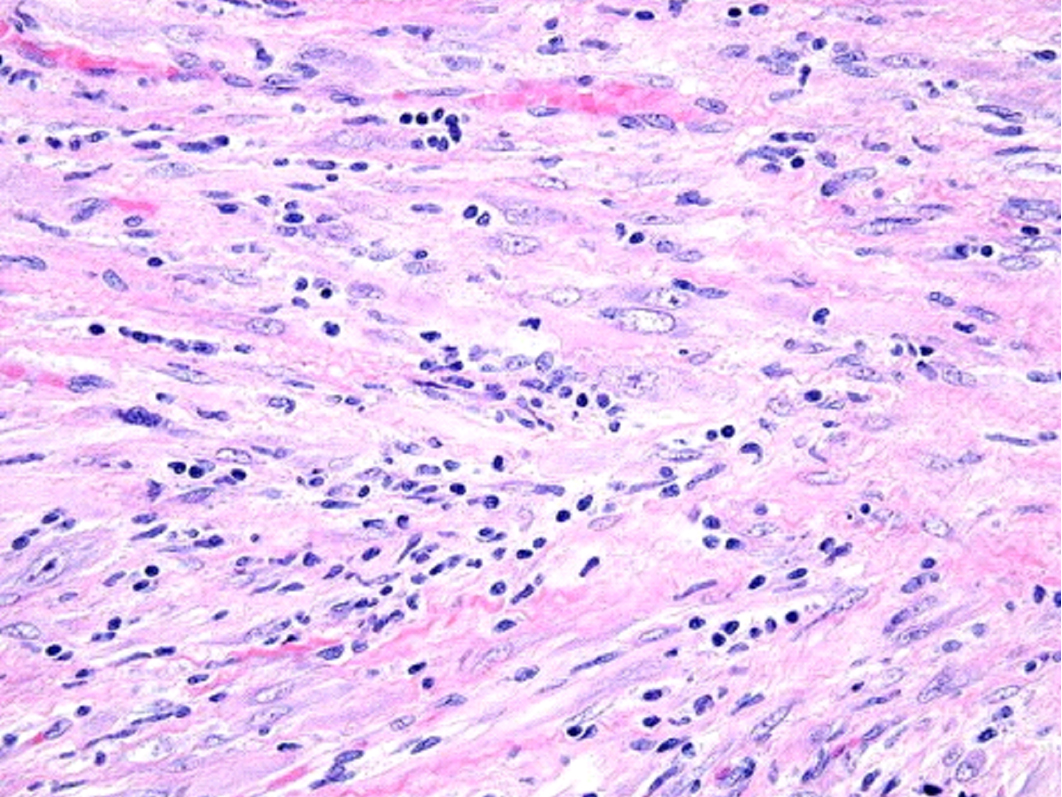
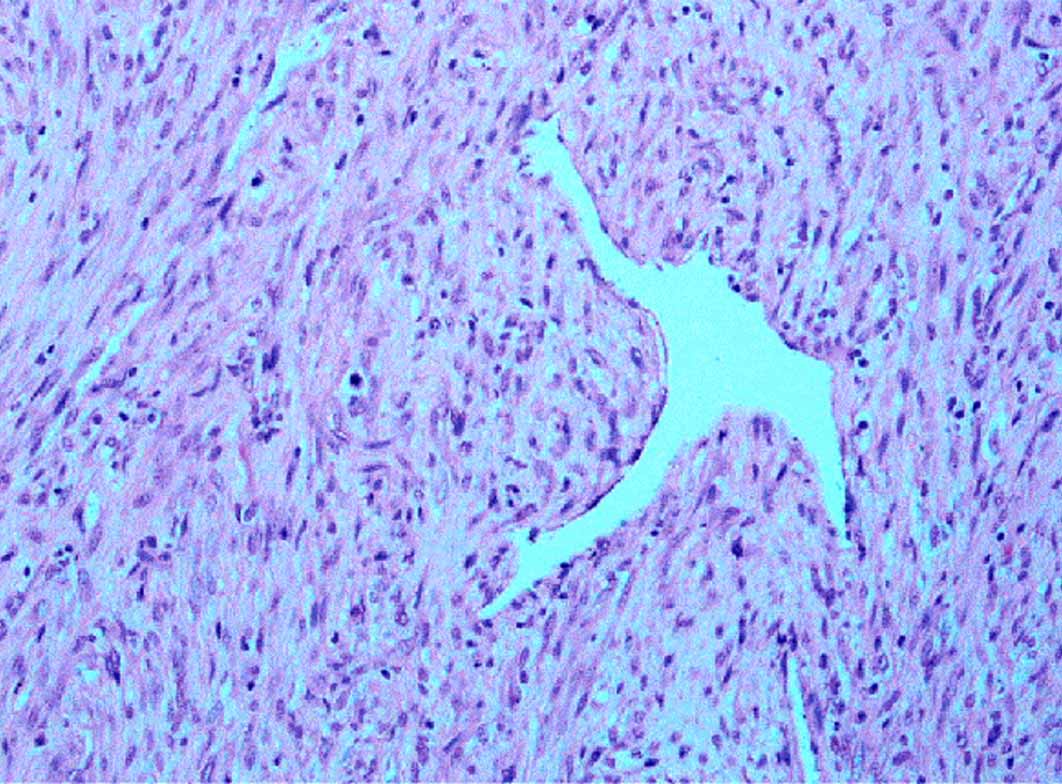
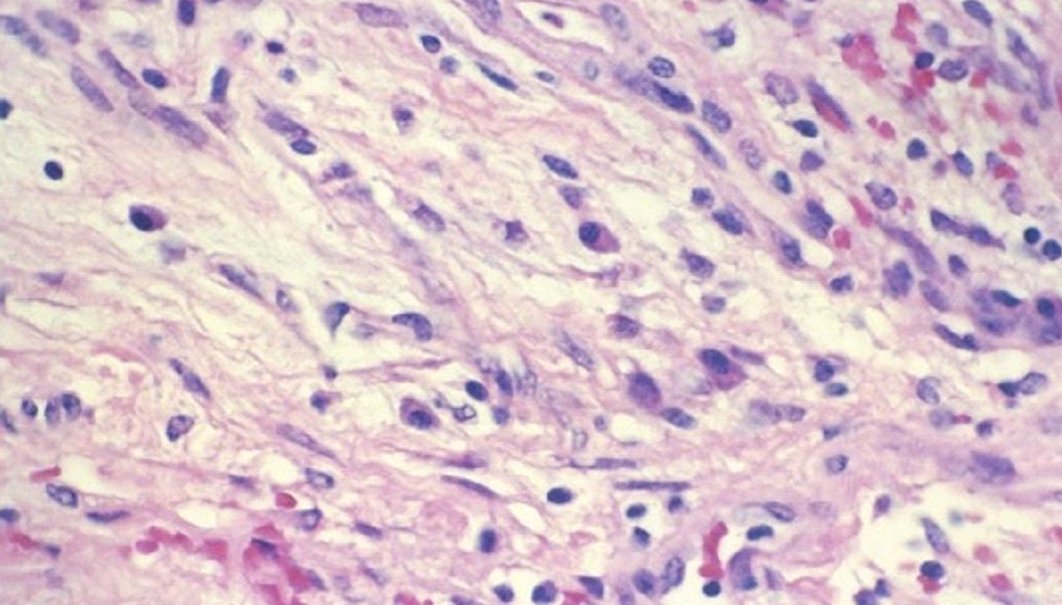
They had large nuclei with prominent nucleoli, but they were without atypia. The mitotic figures were occasional and never abnormal. The cells were separated by a loose, oedematous and myxoid stroma [Table/Fig-1] in which numerous thin-wall blood vessels were present [Table/Fig-2]. There was also a marked inflammatory cell infiltrate which included lymphocytes, neutrophils and eosinophils [Table/Fig-3].
Cellular proliferation of spindle shaped cells arranged in fascicles and an admixture of inflammatory cells.10X view
Spindle cells separated by thin walled blood vessels 10X view
Cellular area showing myofibroblasts and an admixture of inflammatory cells 40X view.
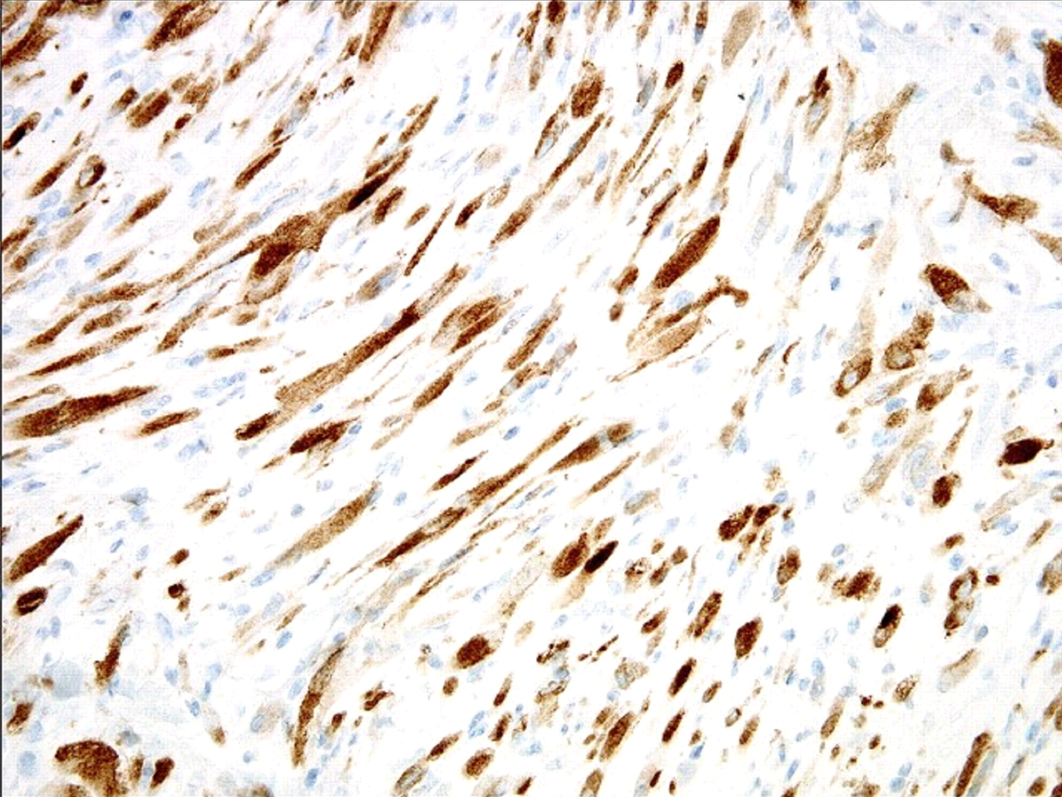
The histochemical studies were positive for mucin and they were negative for the PAS stain in the intercellular areas. On immunohistochemical evaluation, the cells were found to be: positive for vimentin and alk-1 [Table/Fig-4], focally positive for cytokeratins 8/18/19, muscle specific and smooth muscle actins, and desmin and negative for S-100, CD34, C-kit (CD117), h-caldesmon and myod .
Immunohistochemical positivity(nuclear positivity) for anaplastic lymphoma kinase 40X view. This differentiates pseudosarcomatous myofibroblastic tumor from sarcomas and sarcomatoid carcinomas.
A diagnosis of a pseudosarcomatous myofibroblastic tumour was made and a partial cystectomy was done to achieve complete resection of the tumour. The patient has been on surveillance for the past one year and is doing well.
Discussion
The non-neoplastic reactive, mesenchymal proliferation of the urinary bladder is a rare, but distinctive entity, which has been referred to as an inflammatory pseudotumour or a myofibroblastic tumour, a postoperative spindle cell nodule, nodular fasciitis, a pseudosarcomatous myofibroblastic proliferation, a pseudomalignant spindle cell proliferation, or a pseudosarcomatous or an atypical fibromyxoid tumour [1–3]. The unifying feature of these lesions is their tendency to mimic both sarcomas and spindled carcinomas, thus presenting particular diagnostic difficulties in the urinary bladder pathology.
The pathogenesis of an inflammatory myofibroblastic tumour is still in doubt [3]. Some regard this entity as a reactive or an inflammatory condition, while others believe that it represents a low-grade mesenchymal malignancy. The latter endorses the low-grade neoplastic nature of this entity, owing to the occurrence of cases with a deep infiltration of the bladder wall, extension into the perivesical soft tissue and the demonstration of a non-random chromosomal translocation which involves chromosome 2p23, that results in the expression of anaplastic lymphoma kinase (alk) [3].
The pseudosarcomatous myofibroblastic lesions of the bladder may occur at any age (the age ranges from childhood to old age), but they have been reported to typically occur in adult males [2,4,5]. This report was in contrast to other reports [6] that supported a female preponderance. These rare lesions have a non-specific presentation, with painless gross haematuria being the most common presenting symptom. Their size is quite variable, ranging from a few centimeters up to a reported size of 37.5 cm. Endoscopically and radiographically, these cannot be distinguished from malignant tumours [7]. When the tumour was sectioned, the mass was found to be relatively gelatinous and soft or it was found to have a pale, firm cut surface without areas of haemorrhage or necrosis.
Although the lesions are usually confined to the lamina propria, infiltration of the muscularis propria and extension into perivesical soft tissues have been noted [8–10]. Adjacent organ invasion may also be found [8,10]. Distant metastases have not been documented in any of the cases till date. Incomplete excision of the primary site might count for a local recurrence [8].
Sarcomas should mainly be differentiated from this lesion. Some leiomyosarcomas of the urinary bladder can express cytokeratin and they are partially or extensively myxoid to such a degree, that their distinction from inflammatory myofibroblastic tumours may become impossible. However, the reactivity for high-molecular-weight caldesmon, the lack of interspersed inflammatory and red blood cells, and the alk-1 immunostaining in the pseudosarcomatous inflammatory myofibroblastic tumours is of a particular value in the differential diagnosis [11]. Similarly, the sarcomatoid urothelial carcinomas can be distinguished from the inflammatory myofibroblastic tumours by the identification of an in situ or invasive “typical” epithelial component . Another supportive feature which is in favour of the sarcomatoid urothelial carcinomas is their usual alk-1 negativity . With regards to the embryonal rhabdomyosarcomas in the paediatric setting, these can be distinguished from the pseudosarcomatous inflammatory myofibroblastic tumours by the presence of rhabdomyoblasts, a uniform population of small hyperchromatic cells, the presence of a “cambium layer” and positive myogenin (myf4) and myod1 immunostainings [11]. Apart from the sarcomas, the benign lesion which can be confused with the pseudosarcomatous inflammatory myofibroblastic tumours is the post operative spindle cell nodule. But clinically, this occurs in elderly individuals with a history of trauma.
The differentiation of pseudosarcomatous myofibroblastic tumours from rhabdomyosarcomas, leiomyosarcomas or sarcomatoid urothelial carcinomas is important to prevent unnecessary aggressive therapeutic measures (inappropriate radical surgery and adjuvant therapy and their attendant complications), as the complete excision of this tumour by either transurethral resection or partial cystectomy, depending on the size and the extent of tumour, is the recommended treatment of choice. In general, these tumours follow a benign clinical course after their resections, but an additional close follow-up (surveillance cystoscopy and biopsy which are carried out to document the resolution) is advised for most of the cases due to the fact that the biological potential of this entity cannot be accurately assessed [10].
To summarize, an IMT is a rare tumour of the urinary bladder. A high index of suspicion is required for its diagnosis [12]. Biopsy is the gold standard for its diagnosis and immunohistochemistry is very important to confirm the diagnosis. Surgical resection is the treatment of choice.
[1]. Helpap B, Nonepithelial neoplasms of the urinary bladderVirchows Arch 2001 439:497-503. [Google Scholar]
[2]. Watanabe K, Baba K, Saito A, Pseudosarcomatous myofibroblastic tumor and myosarcoma of the urogenital tractArch Pathol Lab Med 2001 125(8):1070-3. [Google Scholar]
[3]. Rosai J, Houston M, Urinary BladderRosai and Ackerman's Surgical Pathology 2004 Volume 19th editionSt LouisMosby:1317-59. [Google Scholar]
[4]. Harik IR, Merino C, Coindre JM, Pseudosarcomatous myofibroblastic proliferations of the bladder: a clinicopathologic study of 42 casesAm J Surg Pathol 2006 30:787-94. [Google Scholar]
[5]. Iczkowski KA, Shanks JH, Gadaleanu V, Inflammatory pseudotumor and sarcoma of the urinary bladder: the differential diagnosis and the outcome in thirty-eight spindle cell neoplasmsMod Pathol 2001 14:1043-51. [Google Scholar]
[6]. Wong-You-Cheong JJ, Woodward PJ, Manning MA, S From the archives of the AFIP: Neoplasms of the urinary bladder: a radiologic-pathologic correlationRadiographics 2006 26:553-80. [Google Scholar]
[7]. Singer AJ, Apple SK, Inflammatory pseudotumor of the urinary bladderInfect Urol 2001 14:68-74. [Google Scholar]
[8]. Gugliada K, Nardi PM, Borenstein MS, Inflammatory pseudosarcoma (pseudotumor) of the bladderRadiol 1991 179:66-8. [Google Scholar]
[9]. Albores-Saavedra J, Manivel JC, Essenfeld H, Pseudosarcomatous myofibroblastic proliferations in the urinary bladder of childrenCancer 1990 66:1234-41. [Google Scholar]
[10]. Controversies in Urological Pathology. International Society of Urological Pathology, Companion meeting 2006 [Google Scholar]
[11]. Lott S, lopez-beltran A, Maclennan GT, Soft tissue tumors of the urinary bladder, Part 1: Myofibroblastic proliferations, benign neoplasms, and the tumors of uncertain malignant potentialHum Pathol 2007 38:807-23. [Google Scholar]
[12]. Stark GL, Feddersen R, Iowe BA, Inflammatory pseudotumor (pseudoscarcoma) of the bladderJ Urol 1989 141:610-2. [Google Scholar]