Introduction
The fractures of the distal radius represent the most common fractures of the upper extremity. The reported overall incidence of the distal radius fractures (DRFs) per year, ranges from 280 to 440 per 100,000 individuals. As many as 20% to 50% of the DRFs are considered to be inadequately reduced and they require surgical fixation [1].
The nondisplaced stable DRFs in physiologically inactive patients are immobilized for a minimal period of time and good results are expected [2–6]. But for the displaced, unstable and the active patients, internal or external fixators have been used. Regardless of the methods of fixation, the principle of reduction is to restore the articular congruity, the radial height, the radial tilt and the volar tilt.
DRFs are recognized as complex injuries with a variable prognosis, depending on several variables which include the fracture type and the method of treatment. The failure to reduce these fractures is associated with more subtle, later problems such as midcarpal instability, incongruity or instability of the distal radioulnar joint, the ulnar impaction syndrome, post traumatic arthritis and pain syndromes which are secondary to small degrees of radial malalignment or intracarpal ligament disruption. Although DRFs cause substantial physical problems and a financial burden to the afflicted patients, the factors that lead to good or poor outcomes after the treatment have not been well characterized [1].
One well-accepted concept is the importance of restoring the articular congruity of the displaced, intra-articular DRFs, especially in young active patients [4]. Several studies have shown that restoring the articular surface favourably influences the functional outcome and that it decreases the incidence of posttraumatic arthrosis [7]. Knirk and Jupiter [8], in a clinical study on patients who were less than forty years old with DRFs with intra-articular involvement, found that the prevalence of osteoarthritis and a poor functional outcome at a mean of 6.7 years after the injury was higher for the fractures which healed with an incongruous radiocarpal joint, than for those which healed with a congruous joint. Trumble et al., [9] suggested that the presence of step off and gap deformities which followed the operative treatment, tended to be associated with worser functional and radiographic outcomes. Further on, he said it had been difficult to demonstrate conclusively that the reduction of the displaced fracture fragments reduced the rate of posttraumatic osteoarthritis and that they led to improved clinical results. However, other authors concluded that despite the progression of arthrosis, the patients showed a high level of function. No statistical correlation was noted between the radiographic or CT scan radiocarpal arthrosis and the clinical function [4].
In a study which was done by Chung et al., [1] they did not find any relationship between the following potential predictors which were identified in the literature as the important factors which influenced the outcomes after DRF: hand dominance, gender, AO fracture classification, radial height, radial inclination, complications, ulnar styloid fracture and ulnar variance.
However, there is an anonymous view that DRFs have to be reduced as anatomically as possible, but whether this anatomic reduction will ultimately lead to a better wrist function, is still in debate. Demographic or radiological parameters with a greater influence on the outcome is also in question, although articular congruity is given priority by many authors [1,9–13] [Table/Fig-1].
Demographic, Injury, and Treatment Data of 80 Patients with Distal Radius
| Average Age (years) | | 37 (21-71) |
|---|
| Gender | Male | 48 |
| Female | 32 |
| Fractured Side | Right | 52 |
| Left | 28 |
| Dominant Hand fractured | | 55 |
| Mechanism of injury | High velocity | 20 |
| Moderate velocity | 35 |
| Low velocity | 25 |
| AO Classification | 23A | 30 |
| 23B | 12 |
| 23C | 38 |
| Displacement | Volar | 22 |
| Dorsal | 58 |
| Mode of Treatment | CR + Cast | 18 |
| CR + Multiple Pinning | 32 |
| CR + Pin ± Ex-Fixator | 20 |
| ORIF | 10 |
The purpose of this study was to prospectively follow a large cohort of patients with DRFs and to determine whetherif the individual radiographic parameters and the overall acceptability of the alignment of the healed DRFs influenced the patient-reported pain and the disability at 3 months, as was given by the standardized patient-rated pain and the disability scores, Gartland and Werley’s Functional Scoring System and the Modified Mayo Scoring System.
Methods and Materials
From January 2007 to March 2012, 80 patients with a mean age of 37 years (range -21 to 71 years) with closed DRFs were treated in our institution within 3 weeks of their injuries. We excluded the skeletally immature patients or those patients with congenital anomalies of the wrist, radio-carpal arthritis, open fractures, neurovascular injuries, associated injuries of the ipsilateral upper limb, bilateral wrist injury, mental incompetence and other systemic injuries. Also, all those patients with incomplete data and those patients who had lost to follow up were excluded from our study. Our research protocols and procedures were approved by the ethical committee of our hospital. 52 of our patients were right handed and 28 were left handed. There were 48 males and 32 females. The injuries were sustained as a result of high velocity road traffic accidents (20 cases), moderate velocity fall and pedestrian injuries (35 cases) and low velocity fall (25 cases). Thirty had the AO type A, 12 had the AO type B, and the remaining 38 had the AO type C fractures. Fifty eight fractures were dorsally displaced and 22 were volarly displaced. The following treatment was employed: fingertrap traction; manipulation to obtain as near an anatomic reduction as possible; application of an above-the-elbow plaster cast for 18 patients, closed reduction and multiple pinning for 32, closed reduction and external fixation for another 20 and open reduction and internal fixation by using a plate and screws for the remaining 10.
After the initial management, X-rays were taken, evaluated and scored by using Sarmiento et al’s modification of the Lidstrom’s scoring system [Table/Fig-2]. Thus, the patients were categorized as having an excellent: 0, good: 1-3, fair: 4-6 or poor: 7-12 reduction. All those patients with an excellent or a good X-ray score or an articular gap of less than 2mm were considered to have an acceptable reduction and those who had a fair or poor X-ray score or an articular gap of more than 2 mm were considered to have unacceptable reduction.
Sarmiento et al’s modification of Lidstrom’s scoring system
| Dorsal Angle (°) | Loss of Radial Length (mm) | Loss of Radial Tilt (°) | Score for Each Measurement |
|---|
| Neutral | <3 | 0-4 | 0 |
| 1-10 | 3-6 | 5-9 | 1 |
| 11-14 | 7-11 | 10-14 | 2 |
| ≥ 15 | ≥ 12 | ≥ 15 | 4 |
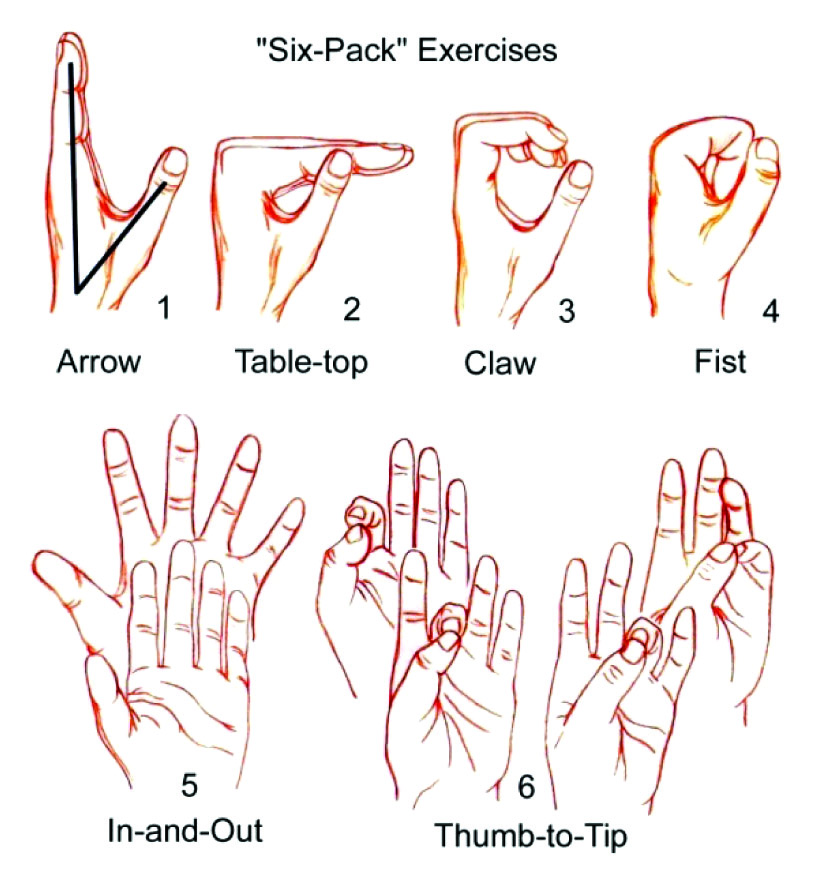
Regardless of the treatment options, all the patients underwent similar post-operative rehabilitation protocols of the department. Active and Passive ROMEs (Range of Motion Exercises) (6 pack exercises) [Table/Fig-3] for the thumb and the digits were started at 2 weeks for half an hour, three times a day. In the 4-6 weeks post-operation, the cast or the pins or the external fixator were removed after evaluating the patients clinically and radiologically. Clinically, there should be a decrease in the pain and minimal tenderness and radiologically, there should be a callus in at least 3 surfaces in the two standard wrist X-ray. A well molded wrist immobilization splint was fitted to wear between the exercise sessions and at night. At 8 weeks, the wrist immobilization splint was gradually worn off and the Active and Passive ROMEs were continued.
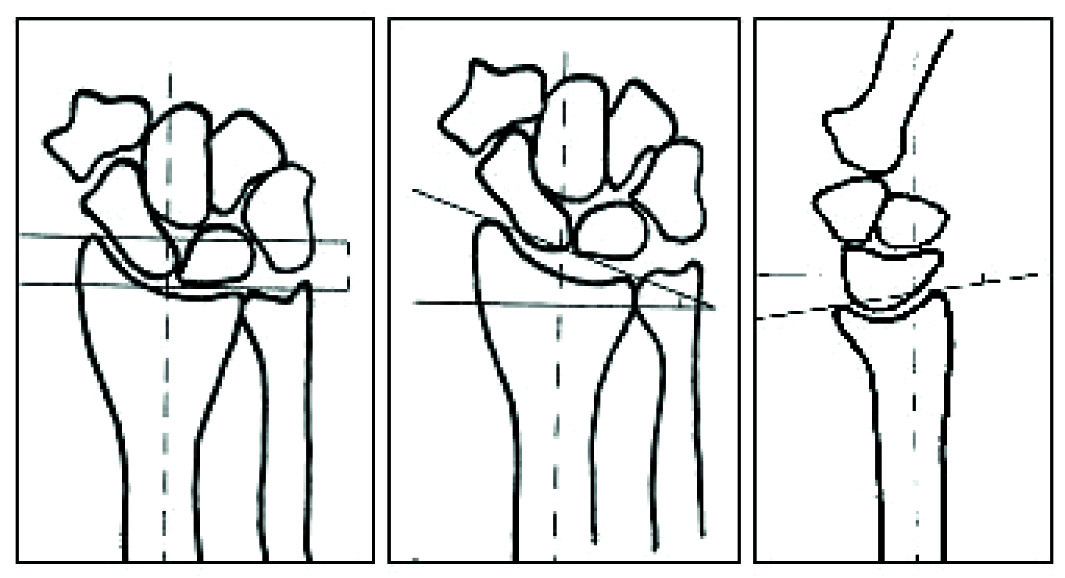
We followed up these patients at 1.5 and 3 months and evaluated them both clinically for the VAS score, the wrist range of motion and the grip strength of the involved and uninvolved hands by using a dynamometer with the arm adducted at the patient’s side and the elbow flexed to 90°, and radiologically for the radial height, radial tilt, volar tilt, ulnar variance, step off and the articular gap. The radiographic parameters in the standard views (PA and lateral), were as follows:
Radial Height: The distance between the tip of the styloid process and the most proximal point of the articular surface of the radius.
Radial Tilt: The inclination of the articular surface of the radius in the frontal plane.
Volar tilt: The inclincation of the articular surface of the radius in the sagittal plane (positive values when it was volar and negative values when it was dorsal).
Ulnar Variance: The distance between the most proximal point of the articular surface of the radius and the ulnar head (positive values when the ulna was more distal than the radius and negative values when it was more proximal) [Table/Fig-2].
Step off: The vertical height between the two fracture fragments.
Articular Gap: The horizontal distance between the two articular fracture fragments.
To analyze the variations between the different scoring systems, we also evaluated them by using the Modified Mayo Scoring System and categorized them into four groups: excellent: 91-100, good: 81-90, fair: 65-80 and poor: <64 [Table/Fig-4].
Modified Mayo Scoring System
| Pain | Functional Status | Motion (% of Normal) | Grip (% of Normal) |
|---|
| 25-No pain | 25-Return to regular employment | 25-90-100 | 25-90-100 |
| 20-Mild, occasional | 20-Restricted employment | 20-80-89 | 15-75-89 |
| 15-Moderate, tolerable | 15-Able to work, but unemployed | 15-70-79 | 10-50-74 |
| 0- Severe to intolerable | 0-Unable to work due to pain | 10-50-69 | 5-25-49 |
| | 5-25-49 | 0-0-24 |
Excellent: 91-100, Good: 81-90, Fair: 65-80 and Poor: <64
The functional status, disability and the return to the pre-injury status were also determined. The evaluation of the results was based on the Gartland and Werley’s Functional Scoring System [Table/Fig-5], which has four categories: excellent- 0-2, good- 3-8, fair- 9-14, and poor -15 and above [Table/Fig-6], [Table/Fig-7].
Radiological evaluation in two standard wrist X-rays. Radial Height, b. Radial Tilt, c.Volar Tilt
Gartland and Werley’s Functional Scoring System
| Pain | Limitation of Motion | Disability | Restricted Activity | Result & Score |
|---|
| None | None | None | None | Excellent, 0 |
| Occasional | Slight | None | None | Good, 2 |
| Occasional | Slight | None if careful | Present | Fair, 4 |
| Often | Present | Present | Marked | Poor, 6 |
| Movement | Range | Score |
|---|
| Extension | <45° | 5 |
| Flexion | <30° | 1 |
| Ulnar deviation | <25° | 3 |
| Radial deviation | <15° | 1 |
| Supination | <50° | 2 |
| Pronation | <50° | 2 |
| Circmduction FFFFff | Loss | 1 |
| Finger flexion | Not to proximal crease/distal crease | 1-2 |
| Grip | Loss of strength | 1 |
| Median nerve compression | Mild, moderate, severe | 1-3 |
Excellent: 0-2, Good: 3-8, Fair: 9-14, and Poor: 15
Results of functional scores, grip strength and complications
| G & W score | 1.5 months | 3 months |
|---|
| Excellent | 0 | 1 |
| Good | 2 | 3 |
| Fair | 5 | 4 |
| Poor | 1 | 0 |
| MM score | | |
| Excellent | 0 | 0 |
| Good | 1 | 1 |
| Fair | 6 | 6 |
| Poor | 1 | 1 |
| Grip strength (% of normal side) | 59 | 70 |
| Pin tract infection 12 of 80 (15%) |
Results
After the initial management, 68 patients had an acceptable reduction whereas 12 patients had an unacceptable reduction. All the 80 patients were followed up at 1.5 and 3 months at our out-patients clinic for the clinical and the radiological evaluations. All the fractures were found to be healed by the end of the study. Of the 80 patients, 12 developed a pin tract infections, (who were treated by closed reduction and with multiple pins with/without an external fixator), all of which subsided within two weeks of taking oral antibiotic treatment.
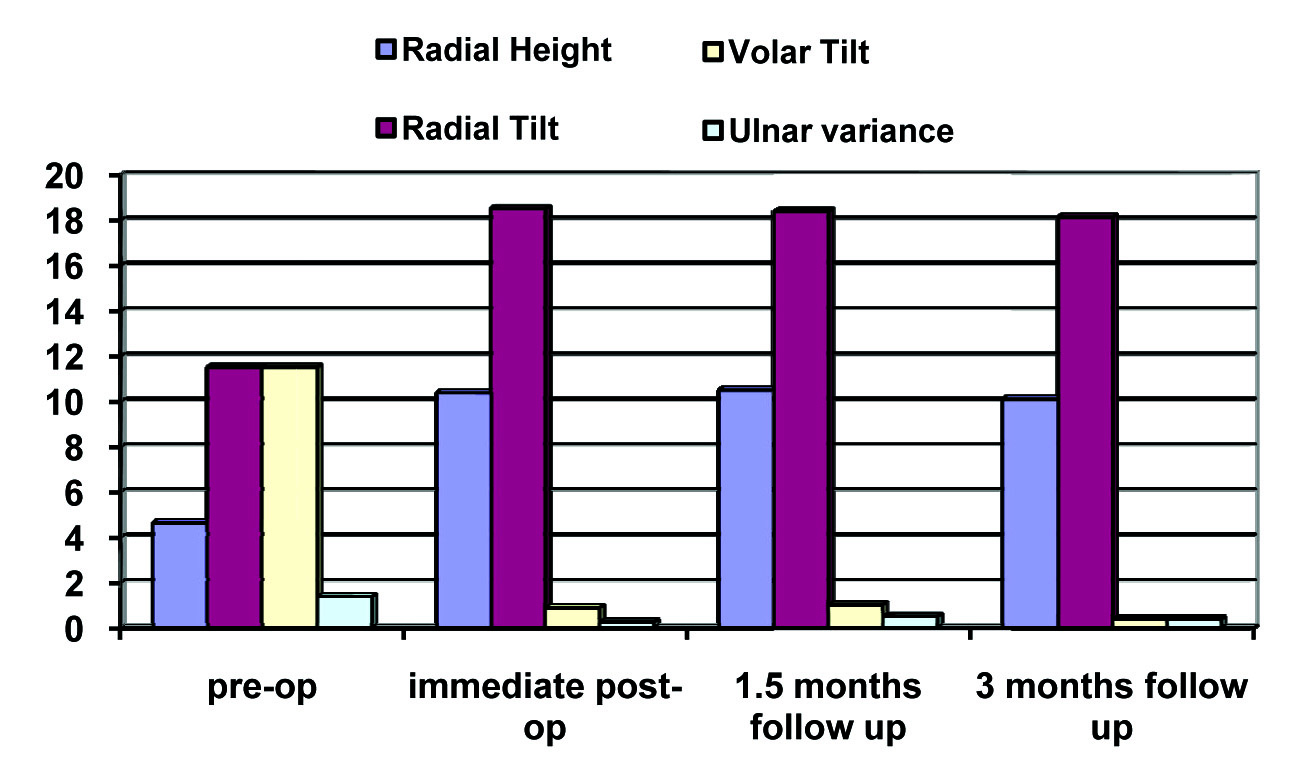
The radiological parameters improved from the pre-operative to the immediate post-operative X-ray and all the parameters remained the same till 3 months of follow up. The grip strength improved from 59% at 1.5 month to 70% at 3 months follow up. We also observed that the functional outcome did not correlated with the X-ray scores. We also observed that the patients with an X-ray score of 10 had only a fair G and W score and MM score [Table/Fig-8], [Table/Fig-9], [Table/Fig-10].
Mean of the Radiological parameters
| Patient | Pre-treatment | Immediate post-op | 1.5 months follow up | 3 months follow up |
|---|
| 1 | 3 | 2 | 2 | 2 |
| 2 | 8 | 5 | 4 | 4 |
| 3 | 4 | 1 | 1 | 1 |
| 4 | 4 | 2 | 1 | 1 |
| 5 | 6 | 2 | 1 | 1 |
| 6 | 4 | 1 | 1 | 1 |
| 7 | 7 | 3 | 2 | 2 |
| 8 | 12 | 10 | 10 | 10 |
| Mean | 6 | 3.25 | 2.375 | 2.375 |
Result of X-ray, MM score and G&W score at 1.5 and 3 months
| Results | X-ray | MM Score | G&W Score |
|---|
| 1.5 month | 3 month | 1.5 month | 3 month | 1.5 month | 3 month |
|---|
| Excellent | | | | | | 10 |
| Good | 60 | 65 | 10 | 15 | 20 | 35 |
| Fair | 10 | 10 | 50 | 55 | 50 | 35 |
| Poor | 10 | 5 | 20 | 10 | 10 | |
We did not also observe any correlation between the two scoring systems and with the final functional outcome.
Discussion
In our series of 80 patients, we found out that all the radiological parameters improved from the pre treatment to the post treatment. Among the radiological parameters, we did not find a particular variable that was associated with either a good or a bad functional outcome at 3 months.
Both the functional outcome measures (the G and W and the MM scores) did not correlate between each other and also with the X-ray score, thus we are not able to determine as to which outcome measure reflected the true functional status among the patients with DRFs. We saw an improving trend for the grip strength and the VAS score along with time. We believe that this trend may continue if these patients are followed up until 1 year.
Various studies [14–16] had experienced complications which were related to hard wares, loose wires, loss of reduction, radial sensory numbness or paresthaesias, extensor tenosynovitis, extensor tendon rupture and post traumatic arthritis . But in our series, we observed 12 pin tract infections and 5 k-wire loosening cases. We attributed this to the short duration of the follow up. However, no patients in our series underwent any secondary procedures.
Evaluating the predictors of the functional outcomes after DRF is difficult because of the variability in the treatment methods, differences in the surgeons’ expertise, the lack of a well-defined study protocol to collect all the relevant data, and the inconsistency in the follow-up times. The purpose of this study was to address many of the deficiencies in the literature, to collect comprehensive outcome data, and to further define these predictors to assist the future treatments. The outcome variables were based on the data from the Gartland and Werley and the Modified Mayo scoring systems, both of which had been shown to be reliable and valid outcome tools for the upper extremity. The outcome questionnaires had been used in other studies [3,11,17–22] in evaluating DRFs, and these questionnaires had provided robust and sensitive dependent variables for constructing a predictive model that could not be accessed via objective measures alone [8,23].
Previous studies [20,24] had shown that the variability in the treatment type had an important effect on the outcomes of the DRF treatment. Therefore, the consistency in using one surgical technique would be an ideal situation in defining the final functional outcome. However, we included all the modes of treatment, so as to increase the sample size, which was still not adequate. For any outcome study such as this project, the prospective data collection is very important to avoid the issues which are related to the missing data and the potential recall bias that can occur with retrospective studies. All the relevant data were collected to find the correlations between them. In our series, we had 18 physiologically old patients whom we treated by closed reduction and long arm casting, as we thought that they were functionally less demanding, as was suggested by Altissimi [2].
The outcome studies [1] have shown that the patients with DRF reach a very high level of clinical functioning at 12 months and that they have little functional improvement thereafter. It was also observed that the recoveries at 3 and 6 months were not statistically significant. Thus, we followed up the patients till 3 months and presented the preliminary results in this paper.
We had an incidence of 12 (15 %) pin tract infections, which was comparable to those in other studies [3,17,25,26] (7-15 %) and 5 k-wire loosening cases. No patients underwent any secondary procedure in our series.
Conclusion
We could not find any correlation between an acceptable reduction to a better functional outcome according to the G and W and the MM scorse. We believe that the results of these data are preliminary and that we need to have more patients to correlate the radiologically acceptable reduction with a good functional outcome. Also, a longer follow up will give us the true functional outcome of these patients and thus a true picture of the correlation between them. However, we still believe that these DRFs should be reduced as anatomically as possible.
Excellent: 91-100, Good: 81-90, Fair: 65-80 and Poor: <64
Excellent: 0-2, Good: 3-8, Fair: 9-14, and Poor: 15
[1]. Chung KC, Kotsis SV, Kim MH, Predictors of the functional outcomes after the surgical treatment of distal radius fracturesJ Hand Surg 2007 32A:76-83. [Google Scholar]
[2]. Altissimi M, Antenucci R, Fiacca C, The long-term results of the conservative treatment of fractures of the distal radiusClin Orthop 1986 206:202-10. [Google Scholar]
[3]. Anzarut A, Johnson JA, Rowe BH, Radiologic and patient-reported functional outcomes in an elderly cohort with conservatively treated distal radius fracturesJ Hand Surg 2004 29A:1121-27. [Google Scholar]
[4]. Burk YT, Vernal TU, Ghazi RM, The outcome following the nonoperative treatment of displaced distal radius fractures in low-demand patients who were older than 60 yearsJ Hand Surg 2000 25A:19-28. [Google Scholar]
[5]. Cassebaum WH, Colles’ fractures: a study on the end resultsJAMA 1950 143:963-65. [Google Scholar]
[6]. Sarmiento A, Pratt GW, Berry NC, Colles’ fracturesJBJS 1975 57A:311-17. [Google Scholar]
[7]. Knirk JL, Jupiter JB, Intra-articular fractures of the distal end of the radius in young adultsJBJS 1986 68:647-59. [Google Scholar]
[8]. Amadio PC, Silverstein MD, Ilstrup DM, The outcome after Colles fractures: the relative responsiveness of three questionnaires and physical examination measuresJ Hand Surg 1996 21A:781-87. [Google Scholar]
[9]. Stewart HD, Innes AR, Burke FD, Functional cast-bracing for Colles’ fracturesJ Bone Joint Surg 1984 66B:749-53. [Google Scholar]
[10]. Keder HJ, Hanel DP, Agel J, Indirect reduction and percutaneous fixation versus open reduction and internal fixation for displaced intra-articular ractures of the distal radius: a randomised, controlled trialJBJS 2005 Jun87:829-36. [Google Scholar]
[11]. Mac Dermid JC, Roth JH, Richards RS, Pain and disability which were reported in the year following a distal radius fracture: a cohort studyBMC Musculoskelet Disord 2003 4:24 [Google Scholar]
[12]. McKay SD, Mac Dermid JC, Roth JH, Assessment of the complications of the distal radius fractures and the development of a complication checklistJ Hand Surg 2001 26A:916-22. [Google Scholar]
[13]. Tsukazaki T, Takagi K, Iwasaki K, Poor correlation between the functional results and the radiographic findings in Colles’ fracturesJ Hand Surg 1993 18B:588-91. [Google Scholar]
[14]. Leon BS, Keith MP, Laura SD, The outcome of the intra-articular distal radius fractures which were treated with fragment-specific fixationJ Hand Surg 2006 31A:1333-39. [Google Scholar]
[15]. Rozental TD, Beredjiklian PK, Bozentka DJ, The functional outcome and complications following two types of plating for unstable fractures of the distal radiusJ Bone Joint Surg 2004 85A:1956-60. [Google Scholar]
[16]. Burk TY, Vernal UT, Ghazi MR, The outcome following the nonoperative treatment of displaced distal radius fractures in low-demand patients who were older than 60 yearsJ Hand Surg 2000 25A:19-28. [Google Scholar]
[17]. Beaulé PE, Dervin GF, Giachino AA, Self-reported disability following distal radius fractures: the influence of hand dominanceJ Hand Surg 2000 25A:476-82. [Google Scholar]
[18]. Catalano LW, IIICole RJ, Gelberman RH, Displaced intra-articular fractures of the distal aspect of the radius. Long-term results in young adults after open reduction and internal fixationJBJS 1997 79A:1290-302. [Google Scholar]
[19]. Fernandez JJ, Gruen GS, Herndon JH, A study on the outcome of distal radius fractures by using the Short Form 36 health surveyClin Orthop 1997 341:36-41. [Google Scholar]
[20]. Gliatis JD, Plessas SJ, Davis TR, Outcome of the distal radial fractures in young adultsJ Hand Surg 2000 25B:535-43. [Google Scholar]
[21]. Karnezis IA, Fragkiadakis EG, Association between the objective clinical variables and the patient-rated disability of the wristJ Bone Joint Surg 2002 84B:967-70. [Google Scholar]
[22]. Mac Dermid JC, Donner A, Richards RS, Patient versus injury factors as the predictors of pain and disability, six months after a distal radius fractureJ Clin Epidemiol 2002 55:849-54. [Google Scholar]
[23]. Mac Dermid JC, Richards RS, Donner A, Responsiveness of the Short From-36, disability of the arm, shoulder, and hand questionnaire, patient-rated wrist evaluation, and physical impairment measurements in evaluating the recovery after a distal radius fractureJ Hand Surg 2000 25A:330-40. [Google Scholar]
[24]. Wilson FC, Dirschl DR, Bynum DK, Fractures of the radius and the ulna in adults: an analysis of the factors which affected the outcomeIowa Orthop J 1997 17:14-19. [Google Scholar]
[25]. Aro HT, Koivunen T, Minor axial shortening of the radius affects the outcome of the Colles’ fracture treatmentJ Hand Surg 1991 16A:392-98. [Google Scholar]
[26]. Field J, Warwick D, Bannister GC, Long term prognosis of displaced Colles’ fractures: a 10-year prospective reviewInjury 1992 23:529-32. [Google Scholar]