Introduction
The word ‘tetanus’ comes from the greek word, tetanos, which is derived from teinein, which means, to stretch. Tetanus was well known to the ancient physicians of Egypt and Greece, but since the institution of active immunization in 1940, it has become an old forgotten disease in the developed countries [1]. The tetanus which is caused by a spore forming bacterium, Clostridium tetani, is an acute and often a fatal disease that is characterised by a generalized increased rigidity and convulsive spasms of the skeletal muscles [2]. The Clostridium tetani spores are found in soil and in animal and human faeces. The contamination of wounds with the spores of C.tetani is probably a frequent occurrence. Their germination and the toxin production, however, take place only in the wounds with a low oxygen-reduction potential, such as those with devitalized tissue, foreign bodies, or active inflammation. The toxin which is released in the wound binds to the peripheral motor neuron terminals, it enters the axon, and it is transported to the nerve-cell body in the brain stem and the spinal cord by a retrograde intraneuronal transport. The toxin then migrates across the synapse to the presynaptic terminals, where it blocks the release of the inhibitory neurotransmitters, glycine and gamma aminobutyric acid (GABA) from the vesicles. The blocking of the neurotransmitter release by tetanospasmin, results in a diminished inhibition due to which the resting firing rate of the alpha motor neuron increases, thus producing rigidity. The loss of inhibition of the preganglionic sympathetic neurons may produce a sympathetic hyperactivity and high circulating levels of catecholamins [3]. The muscle tone is increased, thus producing the characteristic trismus, risus sardonicus, and the opisthotonus. The spasms typically develop one to four days after the initial symptoms. The wounds do not need to be obviously contaminated for tetanus to develop, and in unvaccinated individuals or in people with a waning immunity, even minor wounds can cause a fatal disease [4]. Tetanus is a non-communicable disease and it is not transmitted from person to person [2].
The global incidence of tetanus is estimated to be one million cases annually, with a case fatality rate which ranges from 6% to 72%, depending on the availability of well equipped intensive care units [5].
In the developed countries, its incidence has genuinely declined since 1940, mainly due to the wide spread vaccine coverage [1]. In most of the countries, however, no provision exists for vaccinating the people who were born before these programmes were implemented, thus providing the boosters which are required for a long term protection, or for protecting those who missed the schedules. Even in the countries with good primary immunization programmes, the elderly people may still be vulnerable, either because of the incomplete primary vaccination or because the protective antibody levels decline over time [6,7]. In India, like in most of the developing countries in the world, tetanus is endemic and it remains a public health problem even today. Few studies which were done in India have revealed the prevalence of tetanus and the mortality which is caused by tetanus to be high [8–11]. The present study was a maiden attempt in this part of the country to know the socio-demographic characteristics and the clinical profile, as well as the outcome of the tetanus patients who were admitted at the Epidemic Disease (ED) Hospital, Mysore, India.
Material and Methods
Study Setting and Design
This was a 10 year, retrospective, record based study which was done on adult patients who presented with tetanus to the ED Hospital, Mysore (Karnataka, India), between January 2001 and December 2010. This is a referral hospital for epidemic diseases, which is run by the Government of Karnataka. The hospital caters to the people of Mysore and the neighbouring districts. The consultation, the ward charges and the drugs are provided free of cost. The hospital has 50 beds which include those in the isolation wards for the tetanus patients, excluding those in the intensive care units. A consent was obtained from the institution prior to the start of the study.
Study Subjects
The study included all the patients above the age of 15 years, who were clinically diagnosed to be suffering from tetanus. Details of the demographic data, clinical presentations, management, related complications, duration of the hospital stay, the pre-existing conditions and the outcome were obtained from the medical records and they were entered in a questionnaire before their analysis.
Statistical Analysis
The statistical analysis was performed by using the EPI INFO software package 6.04 version and SPSS, version 16.0. The percentages were calculated for the various parameters which were under study and the Chi square test was applied to test the significance.
Results
The Demographic Profile
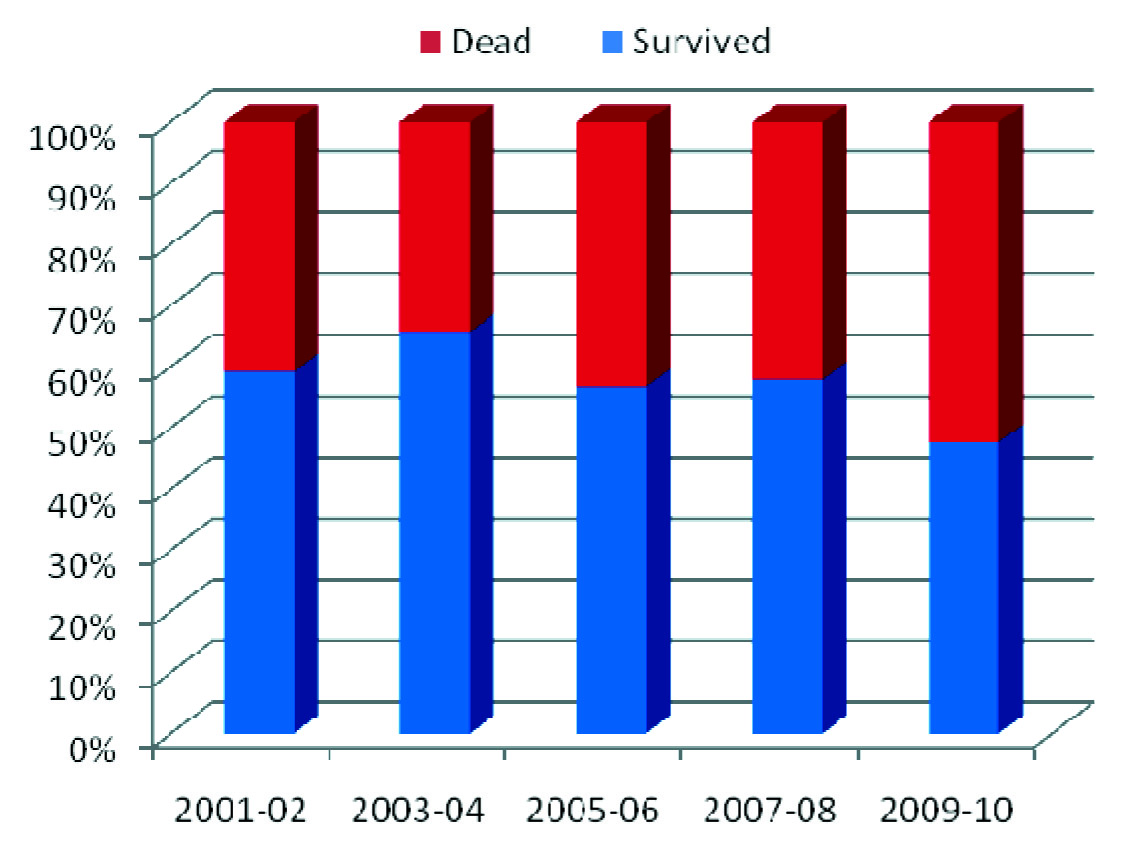
A total of 512 patients were treated during the study period of January 2001 to December 2010. 375 (73.2%) patients were above 40 years of age [Table/Fig-1]. 379 (74%) were males and 133 (26%) were females, with a male to female ratio of 2.8: 1. Their ages ranged from 15 to 81 years, with a mean and a standard deviation respectively of 47.7 and 15.0 years. On an average, about 50 patients per year, got admitted over the past one decade (range-68-39 patients). [Table/Fig-2] shows the outcome trend (which survived versus the dead) over the past decade, which was not statistically significant.
Outcome of tetanus patients admitted over ten year period
Age wise distribution of the tetanus patients
| Age group (years) | Number | Percentage |
|---|
| 15-29 | 60 | 11.7 |
| 30-39 | 77 | 15.0 |
| 40-49 | 125 | 24.4 |
| 50-59 | 112 | 21.9 |
| ≥ 60 | 138 | 27.0 |
| Total | 512 | 100.0 |
Portals of the Entry and the Type of Injury
Acute injuries like pricks, puncture wounds and lacerations were the most common portals of entry in 245 (47.9%) cases and a history of a previous wound was present in 75 (14.6%) patients. The other portals of entry included road traffic accidents (RTA), bites, burns, fissures of the foot and post surgical wounds. The portals of entry were not identified in 111 (21.7%) patients. The most common anatomical site of the injury was the lower limb ie. in 306 (59.8 %) patients [Table/Fig-3].
| Risk Factors | Number of Patients | Percentage |
|---|
| Acute Injury | 245 | 47.9 |
| History of Wound | 75 | 14.6 |
| Fissure Foot | 32 | 6.2 |
| Road Traffic Accident(RTA) | 26 | 5.1 |
| Bites | 10 | 1.9 |
| Surgical Procedure | 7 | 1.4 |
| Burns | 6 | 1.2 |
| None | 111 | 21.7 |
Clinical Profile
All the 512 patients had generalized tetanus. About 40% of the patients who survived, stayed in the hospital for over 20 days or more [Table/Fig-4]. The most common presenting symptoms were trismus -490 (95.7%), neck stiffness- 457 (89.3%), body spasms and stiffness -374(73%) and dysphagia -199 (38.9%) [Table/Fig-5].
Duration of hospital stay of tetanus patients who survived (N=295)
| Duration of stay (in days) | Number | Percentage |
|---|
| <5 | 12 | 4.1 |
| 5-9 | 35 | 11.9 |
| 10-14 | 58 | 19.7 |
| 15-19 | 72 | 24.4 |
| ≥ 20 | 118 | 40.0 |
Presenting complaints of tetanus patients
| Presenting Complaint | Number of Patients | Percentage |
|---|
| Trismus | 490 | 95.7 |
| Neck Stiffness | 457 | 89.3 |
| Body Spasm/Rigidity | 374 | 73.0 |
| Dysphagia | 199 | 38.9 |
| Body Pain | 46 | 9.0 |
| Dyspnea | 38 | 7.4 |
| Fever | 30 | 5.9 |
| Others* | 16 | 3.1 |
Urinary retention, headache, cough
Treatment
All the patients were managed with the tetanus toxoid (0.5ml I.M.), human tetanus immunoglobulin (3000IUIM), antibiotic therapy (penicillin and metronidazole) and muscle relaxants (diazepam or methocarbamol), depending on the severity, wound care and throat suction with oxygen through a mask, whenever it was required. Supportive therapy such as fluids and calorie intake, prevention of gastric ulcers and prevention of bed sores were provided to all the patients. For some periods between 2001 to 2005, in the absence of the availability of the human tetanus immunoglobulin, the anti- tetanus serum (ATS) after the test dose, was used.
Outcome
Of the total 512 patients, 296 (57.8%) survived, 21 (4.1%) patients were DAMA (Discharged Against Medical Advice) and 5 (1%) patients were referred. The case fatality rate was 42.2%. Of the 375 people who were above the age of 40 years, 181(42.3%) died and out of the 137 patients below the age of 40 years, 35 (25.5%) died. There was a statistically significant relationship with respect to the age and outcomes (survival and death) [Table/Fig-6].
Distribution of tetanus patient’s outcome according to various parameters
| Variables | Outcome of treatment | X2 Value | P-value |
|---|
| Survive (N/%) | Dead (N/%) |
|---|
| Age (years) (n=512) |
| <40 | 102 (74.5) | 35 (25.5) | 21.236 | 0.000* |
| ≥ 40 | 194 (51.7) | 181 (48.3) |
| Sex (n=512) |
| Male | 222 (58.6) | 157 (41.4) | 0.348 | 0.555 |
| Female | 74 (55.6) | 59 (44.4) |
| Incubation period (days)(n=466)† |
| < 7 | 26 (43.3) | 34 (56.7) | 3.49 | 0.062 |
| ≥ 7 | 296 (72.9) | 110 (27.1) |
| Complications (n=496)† |
| Yes | 12 (5.5) | 207 (94.5) | 4.453 | 0.000* |
| No | 276 (99.6) | 01 (0.4) |
| Pre-existing condition (n=463)† |
| Yes | 08 (42.1) | 11 (57.9) | 2.456 | 0.117 |
| No | 267 (60.1) | 177 (39.9) |
| Place of residence (n=512) |
| Urban | 25 (65.8) | 13 (34.2) | 1.07 | 0.301 |
| Rural | 271 (57.2) | 203 (42.8) |
P value <0.05 is statistically significant at df=1
Data not available for all subjects
Discussion
Tetanus is still prevalent in the developing world with a significantly high morbidity and mortality, despite the availability of an effective vaccine. Of the total 512 cases which were studied in the 10 year period between 2001 to 2010, 379 (74%) were males and 133 (26%) were females. The male pre-ponderance in this study was in accordance with the findings of other Indian studies [8,10,11] and with that of other studies which were done in the developing world [12–17]. This can be explained by the fact that men spend more time in farming activities and other field work and that hence they are more likely to be exposed to the Clostridium tetani spores which are ubiquitous in the soil and that the females are protected against tetanus by the TT immunization which is given during the antenatal period. About 474 (92.5%) patients were from the rural areas as compared to 38 (7.4%) patients from the urban areas, which reflected the high risk population in terms of the occupational and the general propensity to the risk of injury due to the poor environmental conditions. In the present study, 375 (73.2%) patients were above the age of 40 years and 137(26.7%) patients were below the age of 40 years, which was in sound agreement with the findings of the studies which were done in Malaysia and Bangladesh [13,17]. This could be attributed to a low immunity against tetanus, as they would have never received the vaccination. This observation was also consistent with a population based serologic survey which was done in the United States of America, which showed that the prevalence in Americans of the protective levels of the tetanus antibody declined rapidly, starting at the age of 40 years and that most cases of tetanus occurred in persons of the older age groups [1,7]. The present study also showed that the mortality was more in people who were above 40 years, which was in agreement with the findings of a study which was done by Chalya et al. [12].
As in other studies, a majority of the patients were daily wage workers or farmers (91.1%) [10–14,16,17]. This can be explained by the fact that most of the people who worked barefoot in the fields were at a higher risk of exposure to the tetanus spores. Homemakers and other professionals constituted only 9% of the patients. All the 512 cases were of generalized tetanus in the present study, with the most common presenting symptoms of trismus -95.7%, neck stiffness -89.3%, body spasms/stiffness -73% and dysphagia- 38.9%, which was in accordance with the findings of other studies. Thus, a high amount of clinical suspicion is necessary whenever the patients present with the above symptoms, as tetanus is mainly diagnosed clinically and as the laboratory tests and cultures are of little diagnostic value [2]. Of the total 512 patients, 13 patients were known cases of Diabetes mellitus and seven patients had chronic suppurative otitis media (CSOM).
The most important risk factor for the disease was acute injury, which was seen in 47.9% patients. 14.6% patients had a history of wounds and 5.1% patients developed tetanus after meeting with road traffic accidents (RTA). 10 patients developed tetanus secondary to animal bites, which included dog, snake, cat and bat bites, 7 patients developed tetanus after undergoing a surgical procedure and 6 patients developed tetanus secondary to burns. In 111 (21.7%) patients, there was no identifiable portal of entry, thus reflecting that the injuries were very trivial for the patients to be recalled. A majority of the injuries occurred on the lower limb, which was in accordance with the findings of other studies [8,10,12–14]. This may be due to the practice of working barefoot in the fields and also due to the lack of protective footwear. The incubation period, which is defined as the time between the inoculation of the wound and the onset of the symptoms, was identified in only 314 patients. Of these, 60 (19.1%) patients had an incubation period which was lesser than 7 days and 254 (80.9%) patients had an incubation period of more than 7 days. The duration of the hospital stay for the patients who were discharged alive, was between 1 to 54 days, with a mean of 17.38 + 7.05 days. Only 72 (14.1%) patients had received the post injury prophylaxis with the tetanus toxoid. None of the tetanus cases which were identified had a documented evidence of the primary immunization against tetanus.
Complications were seen in 241(47%) people, with cardio-respiratory arrests being seen in 193 (37.7%) patients and aspiration pneumonia in 38 (7.4%) of the total patients. The presence of the complications had a statistical significance with respect to the outcome of the patients [Table/Fig-5]. None of the patients underwent tracheostomy nor were they put on mechanical ventilators for want of an ICU facility.
A varied prognosis of the patients with tetanus has been reported from different studies, which was found to range from 10%-60%. In this study, the mortality was found to be 42.2% which was comparable with the observations which were reported by Chalya et al., [12] from Tanzania L Ramkrishna et al., [10] reported a mortality of 23.3% and Patel et al., [8] reported a mortality of 58.3% in non- neonates, with an incubation period which was less than seven days. A lower mortality was reported from Malaysia [13] (18.2%), Nigeria [14] (32.91%), Ethiopia [15] (38%) and Thailand [16] (4%). The poor prognostic factors which were seen in this study included age more than 40 years, the presence of complications and a lack of tracheostomy due to the absence of a well equipped ICU facility. Most of the deaths were due to cardio-respiratory arrests, an observation which was similar to those which were seen in other studies [12,17].
The limitations of the present study were, the fact that we could not group the patients based on the severity and that the information about some patients was incomplete in view of the retrospective nature of the study, which may have introduced some bias into our findings.
Conclusion
Though tetanus is a vaccine preventable illness, its prevalence is still high in this part of the country. It still remains a difficult disease to treat, with high morbidity and mortality. The incidence of tetanus can be reduced with
Effective immunization programs for the adults, as neonates and small children are already covered under the National Universal Immunisation Program.
An early diagnosis, a proper wound management immediately after the injury, health education programs to create awareness among the public and establishing an ICU facility in the hospital would definitely decrease the morbidity and the mortality.
[1]. Bleck TP, Mandell GL, Bennett JE, Dolin R, Clostridium TetaniPrinciples and Practices of Infectious Diseases 2005 vol 26th editionPhiladelphiaChurchill Livingstone:2817-22. [Google Scholar]
[2]. Tejpratap SP, Tiwari MD, Sandra WR, Lynne M, Linda MB, TetanusManual for the Surveillance of Vaccine Preventable Diseases 2011 5th edAtlanta, GACentre for Disease Control and prevention:1-6. [Google Scholar]
[3]. Elias Abrutyn, Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, TetanusHarrison’s Principle’s of Internal Medicine 2008 17th edNew YorkMc Graw Hill Inc:898-900. [Google Scholar]
[4]. Farrar JJ, Yen LM, Cook J, Fair WN, Binch N, Parry J, TetanusJournal of Neurology, Neurosurgery and Psychiatry 2000 69(3):292-301. [Google Scholar]
[5]. Oladerian I, Meir DE, Ojelade AA, Olaolorn DA, Adeniran A, Tarpley JL, Tetanus- a continuing problem in the developing worldWorld J Surgery 2002 26(10):1282-85. [Google Scholar]
[6]. Thwaites CL, Farrar JJ, Preventing and treating Tetanus-The challenge continues in the face of neglect and lack of researchBMJ 2003 326:117-18. [Google Scholar]
[7]. Gregen PJ, McQuillan G, Kiely M, Ezzati Rice TM, Sutter RW, Virella G, A population-based serologic survey on the immunity to tetanus in the United StatesN England Journal Medicine 1995 332:761-66. [Google Scholar]
[8]. Patel JC, Mehta BC, Tetanus: A study on 8697 casesIndian J Med Science 1999 53:393-401. [Google Scholar]
[9]. Pawar AB, Kumawat AP, Bansal RK, An epidemiological study on the Tetanus cases which were admitted to a referral hospital in SolapurIndian Journal of Community Medicine 2004 29(3):115-116.Available from: http://www.ispub.com:80/journal/a-retrospective-clinical-study-of-factors-affecting-tetanus.html/ [Google Scholar]
[10]. Ramachandra L, Shobha KL, Arun Kannan P, A retrospective clinical study on the factors which affected TetanusThe Internet Journal of Microbiology 2009 7(1)(cited 2011 Dec 14) [Google Scholar]
[11]. Chavada VK, To study the clinic – epidemiological factors of the Tetanus cases which were admitted to a tertiary care hospital during the last 10 yearsJournal of Clinical and Diagnostic Research 2010 4:2649-51. [Google Scholar]
[12]. Chalya PL, Joseph BM, Ramesh MD, Nkinda M, Stephen EM, Japhet MG, A 10-year experience with Tetanus at a tertiary hospital in north western Tanzania: A retrospective review of 102 casesWorld Journal of Emergency Surgery 2011 6:20 [Google Scholar]
[13]. Lau LG, Kong KO, Chew PH, A 10-year retrospective study on Tetanus at a general hospital in MalaysiaSingapore Med J 2001 42(8):346-50. [Google Scholar]
[14]. Adekanle O, Ayodeji OO, Olatunde LO, Tetanus in a rural setting of south-western Nigeria: A ten year retrospective studyLibyan J Med 2009 4:100-04. [Google Scholar]
[15]. Amare A, Yami A, The case fatality of adult Tetanus at the Jimma University Teaching Hospital, southwest EthiopiaAfrican Health Sciences 2011 11(1):36-40. [Google Scholar]
[16]. Pornchai S, Chutarat S, Kitti L, Suwanna S, Kanitpong P, Tetanus -A retrospective study of the clinical presentations and the outcomes in a medical teaching hospitalJ Med Assoc Thai 2009 92(3):315-19. [Google Scholar]
[17]. Feroz AHM, Rahman MH, A ten-year retrospective study of tetanus at a teaching hospital in BangladeshJ Bangladesh Coll Phys Surg 2007 25:62-69. [Google Scholar]