Introduction
Catheter Associated Urinary Tract Infections (CAUTIs) are the most common nosocomial infections in hospitals and nursing homes, which constitute 30%-40% of all the hospital acquired infections [1]. They have been associated with increased morbidity, mortality, hospital costs, and length of the hospital stay [2]. The prevalence of CAUTIs in the catheterized patients in acute care settings (catheter used for <7 days) is 3%-7%, in patients who require a urinary catheter for >7 days, it is up to 25% and it approaches 100% after 30 days [3,4]. About 17% of the healthcare associated bacteraemias are from urinary sources, with an associated mortality of approximately 10% [5].
Virtually, all the healthcare-associated Urinary-Tract Infections (UTIs) are caused by the instrumentation of the urinary tract (insertion of catheters). The risk factors which are associated with CAUTIs include female sex, older age, prolonged catheterization, impaired immunity, diabetes, renal dysfunction, severity of illness, insertion of the catheter outside of the operating room, inadequate professional training of the person who inserts the catheter, incontinence and the inpatients in the orthopaedic and the neurology departments [2].
The sources of the microorganisms which cause CAUTIs can be endogenous, i.e., via meatal, rectal or vaginal colonization or exogenous, i.e., via the contaminated hands of the healthcare personnel or via contaminated equipment. Microbial pathogens can enter the urinary tract either by the extra-luminal route [6], along the outside of the catheter, or by the intra-luminal route along the internal lumen of the catheter from the contaminated collection bag or from the catheter drainage tube junction. As the duration of the catheterization increases, there is the formation of a biofilm which renders the bacteria resistant to antimicrobials and difficult to treat [7]. CAUTIs comprise perhaps the largest institutional reservoir of nosocomial pathogens [8–10], the most important of which are multidrug-resistant Enterobacteriacae, other than Escherichia coli, such as Klebsiella, Enterobacter, Proteus, and Citrobacter; Pseudomonas aeruginosa; A. baummannii; Enterococci and Staphylococci and Candida spp [11].
Urinary-Tract Infections (UTIs) are defined by using Symptomatic urinary-Tract Infection (SUTI) criteria or asymptomatic bacteraemic UTI (ABUTI) criteria. UTIs that are catheter-associated (i.e., in which the patients have an indwelling urinary catheter at the time of or within 48 hours before the onset of the event) are reported by using diagnostic criteria as per the CDC guidelines [12].
Supervision programs which involve bundled infection control practices in hospitals do bring the rates of CAUTIs down. About 17%-69% of the CAUTIs may be prevented by taking the recommended infection control measures [13]. Certain issues however remain unresolved. Are the infection control practices labour and cost effective? Is a uniform protocol for the sample collection and the diagnosis of CAUTIs followed by all the clinicians? Which infection control practices result in the maximum reduction of the CAUTIs? To answer all these questions, this study was undertaken.
Methods
The entire study was a before-after study with historical controls, which covered a period of one year from January 2009 to December 2009, in an Indian tertiary care 215 bedded super-speciality hospital setting. In the first 6 months, the data which pertained to the inpatients (in the ICU and the wards) with a urinary catheter was analyzed to see the number of CAUTIs. The urine sample collection protocols were critically examined to detect the deviations from standard guidelines [2] and to institute corrective measures if required. In the microbiology lab, the organisms which were isolated from the urine specimens were subjected to standard identification [14] and sensitivity testing by using VITEK 2 Compact Biomerieux and the results were recorded in the WHONET 5.4 programme. The CAUTIs rates per month were calculated as the number of urinary infections divided by the total number of catheter days. The diagnosis of the urinary tract infections and asymptomatic bacteriuria was done according to the standard definitions for urinary tract infections which was given in the National Healthcare Safety Network (NHSN) guidelines [12]. In the first 6 months, any deviations in the methodology of the UTI diagnosis according to the guidelines were recorded and these were subsequently corrected after the institution of the supervision programme in the month of July. Each CAUTI case was analyzed for the indication for the catheterization, duration of the catheterization, age, sex, and other risk factors.
In the month of July 2009, the UTI supervision program was instituted. Under this program, in the first week, the key areas which required improvement were identified. In the second week, the bundle of prevention measures was implemented by means of a urinary catheter checklist [Table/Fig-1] by giving relevant training. Training was also imparted on the standard definitions and the guidelines, as was outlined by the HICPAC [2]. During the third and the fourth weeks, auditing was conducted by the infection control department to determine the compliance to the urinary catheter checklist and the hand hygiene practices.
Urinary Tract Infection Rates for Year 2009
| Month (2009) | Number of UTI | Total catheter days | Rates of UTI/1000 catheter days |
|---|
| January | 1 | 197 | 5.07 |
| February | 2 | 243 | 8.23 |
| March | 1 | 290 | 3.44 |
| April | 1 | 281 | 4.7 |
| May | 8 | 473 | 16.9 |
| June | 7 | 276 | 25.3 |
| July | 3 | 507 | 5.9 |
| August | 1 | 433 | 2.3 |
| September | 3 | 403 | 7.4 |
| October | 2 | 442 | 4.5 |
| November | 3 | 381 | 7.9 |
| December | 2 | 360 | 5.6 |
| TOTAL | 34 | 4286 | 7.93 |
The urinary catheter checklist adherence by the staff was monitored for all the catheterized patients all over the hospital and the rates were calculated as:

Non-compliance with two components in the checklist, namely bladder irrigation and practising perineal cleaning thrice a day, was still taken as full compliance, but the non-compliance was noted.
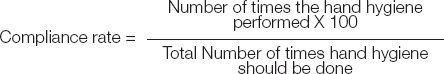
A special emphasis was placed on the hand hygiene and the hand hygiene compliance rate was calculated as
At the end of the supervision program, an assessment was made of the impact of the intervention on the CAUTI rates (comparison of the pre-intervention rates [baseline] with the post-intervention rates).
Results
A total of 34 CAUTI cases were documented in the entire year (Jan 2009-Dec 2009). The average CAUTI rate for the year was 7.93.
Among the 34, 20 infections (58.8%) occurred in the first 6 months. The introduction of the supervision program was done in July and the following 6 months showed 14 infections (41.2%). The average CAUTI rate [Table/Fig-1] in the first 6 months was 10.6 and it reduced to 5.6 (47.1% decrease) in the next 6 months.
The age and gender distribution of the CAUTIs for the different age groups (<5 years to >65 years) showed a higher number of infections in the age groups of 50-65 and >65 years (11 infections each out of 34 infections). The gender distribution showed an almost equal number of infections in both the sexes [18 (52.94%) in males and 16 (47.05%) in females]. The average duration of the catheterization was 17.1 days for all the catheterized patients for the entire year. However, in the first 6 months, the average duration of the catheterization was 23 days and after the supervision program, it reduced to 21 days (8.67% reduction).
The total number of microorganisms which was isolated from the 34 infections was 37, as more than one organism was isolated from some samples and their sensitivity pattern was recorded [Table/Fig-2]. The predominant organisms were Candida spp (29.7%), E.coli (18.9%), Klebsiella pneumoniae (18.9%) and others [Providencia rettgerii (13.5%), Enterococcus spp (5.4%), Pseudomonas aeruginosa (5.4%), Proteus mirabilis (2.7%), Myroides spp (2.7%) and Acinetobacter baumannii (2.7%)].
Antibiotic susceptibility patterns of Organisms Isolated from Positive Urine Cultures
| Organisms Isolated | Number of isolates | Antibiotics Susceptibility |
|---|
| Candida | 11 | NA* |
| Klebsiella pneumoniae | 7 | ESBL† (5)- Polymixin B, Colistin, Tigecycline, Carbapenems Cefoparazone-Sulbactam |
| Non-ESBL(2)- Cefipime, Ciprofloxacin, Cefuroxime, Tigecycline, Colistin, Polymixin B |
| Providencia rettgeri | 5 | Colistin, Polymixin B & Piperacillin-Tazobactam |
| E. Coli | 7 | ESBL (3)- Colistin, Imepenem, Meropenem, Tigecycline, Polymixin B, Nitrofuratoin, Piperacillin-Tazobactam |
| Non-ESBL(4)- Cefipime, Cefuroxime, Amikacin, Imepenem etc |
| Acinetobacter†baumannii | 1 | Colistin, Polymixin B |
| Enterococcus spp (VRE)‡ | 2 | Teicoplanin, Chloramphenicol, Linezolid, Rifampicin |
| Pseudomonas† | 2 | Polymixin B, Colistin, Nitrofurantoin |
| Proteus | 1 | Amikacin, Cefipime, Cefuroxime, Ceftazidime, Nitrofurantoin |
| Myroides | 1 | Multi drug resistant |
Candida is not processed for sensitivity in urine specimens.
Carbapenem Resistant strains.
Vancomycin Resistant Enterococci showing resistance to high level Gentamicin.
The average urinary catheter checklist adherence rate was 45% before the supervision program and it was 65% after the program, which showed an increase of 44.4% (p=0.069) [Table/Fig-3]. The average rates of the hand hygiene compliance [Table/Fig-3] before and after the supervision program were 33% and 51% respectively, thus indicating an increase of 56.4% (p=0.0004).
Comparison of Average rates of Urinary Catheter Checklist Adherence & Hand Hygiene Compliance for the year 2009
| Month (2009) | Average Urinary catheter Checklist Adherence Rate | Average Hand Hygiene Compliance Rate | CAUTI |
|---|
| Pre-Intervention |
| January | 55 | 20 | 1 |
| February | 45 | 25 | 2 |
| March | 55 | 30 | 1 |
| April | 60 | 37 | 1 |
| May | 25 | 40 | 8 |
| June | 30 | 46 | 7 |
| Post Intervention |
| July | 50 | 40 | 3 |
| August | 65 | 45 | 1 |
| September | 60 | 50 | 3 |
| October | 70 | 45 | 2 |
| November | 65 | 60 | 3 |
| December | 80 | 70 | 2 |
A detailed study of the sample collection protocols in the first 6 months revealed a flaw in the sample collection in 5 out of the 20 cases (25%), where a possibly contaminated sample was used for the analysis. The staff were made aware of the standard guidelines for the sample collection. In 4 out of 20 cases (20%), in the first 6 months, there was an inappropriate diagnosis of the UTIs. Overall, 9 out of 20 (45%) cases, in the first 6 months, were not true CAUTIs.
Discussion
There were 34 patients who acquired the catheter associated urinary tract infections as per the study which was conducted for a period of one year. The CAUTI rates varied over the year between 2.3 to 25.3 urinary tract infections per 1000 catheter days. The average CAUTI rate per month for the entire year was 7.93, though the first 6 months showed a rate of 10.6 and the next 6 months showed a rate of 5.6. This was because of the introduction of the UTI supervision program in the middle of the year, which brought the rates down by 47.1%. Multifaceted infection control/quality improvement programs do reduce the risk of the CAUTIs [15,16].
The results which were obtained by Madani N et al., [17] in Morocco corresponded to the results of our study, where the average CAUTI rate was 11.7 per 1000 catheter days. In contrast, findings from New York [18] indicated the average CAUTI rate to be 3.61. The studies which were carried out by WHO [19] also indicated that the developed countries showed a lower rate of UTIs (< 5 CAUTIs per 1000 catheter days) as compared to that in the developing countries (5-15 CAUTIs per 1000 catheter days). This may be because of the high standards of the infection control policies and the protocols which were being followed in the developed countries.
As was observed in the present study, the mean age of the patients who developed CAUTIs was 54.5 years. A surveillance report which was made by Maha Talaat et al., showed that patients above 40 years of age had a significantly higher risk of acquiring CAUTIs [20]. Chao et al., [21] and Hussain et al., [22] indicated that females and elderly and debilitated patients were at a higher risk of acquiring infections. However, in the present study, equal number of males and females [18 (52.94%) males and 16(47.05%) females] were found to develop CAUTIs. This was probably because of the risk factors which contributed equally in both the sexes in the older age group.
For the patients who developed CAUTIs in the first 6 months, the average duration of the catheterization was 23 days and after the supervision program, it reduced to 21 days. These results were similar to those of a study which was done by T Tsuchida et al., [23] in Japan, where the mean duration of the catheterization was 25 days. Other studies have reported the average duration of the catheterization to be 16.4 days [24]. A study which was done by Garibaldi et al., [25] showed that the risk of developing bacteriuria increased by 5% for each additional day when the catheter was in situ and that after the tenth day, 50% of the patients had acquired bacteriuria.
The present study showed that the organism which was most commonly isolated from the CAUTIs was Candida spp, which showed 29.7% prevalence, which was in accordance to that in the prospective studies from the ICUs of Cairo University and Alexandria University Hospital, with 50% and 51% prevalence of Candida spp. in the CAUTIs [26]. Candida was followed by E.coli and K. pneumoniae, which showed an equal prevalence of 18.9%. Among these isolates, there were 42.8% ESBLs in E. coli (3 ESBLs out of 7 E.coli) and 71.4% ESBLs in K. pneumoniae (5 ESBLs out of 7 K. pneumoniae). Other isolates included P. rettgerii (13.5%), Enterococcus spp (5.4%), P. aeruginosa (5.4%), P. mirabilis (2.7%), Myroides spp (2.7%) and A. baumannii (2.7%). In a similar study, Jha et al., [27] found that most of the common organisms which were responsible for CAUTIs were E. coli (49%), Staphylococcus aureus (23%), Proteus spp. (3.6%), Klebsiella (9.71%), P. aeruginosa (0.8%), and Citrobacter (2.8%).
Checklists have tremendous potential for improving the safety and the quality of the infection control guidelines and for reducing the chances of omissions [28]. Therefore, the urinary catheter checklist adherence was an important focus of the supervision program. The average rate of the urinary catheter checklist adherence of the healthcare staff increased by 44.4% after the supervision program. Similarly, the hand hygiene compliance of the staff was also monitored by regular audits and it was found to increase by 56.4%. This steady increase in the rates of hand hygiene compliance in the entire year may have been a result of the continuous implementation of the hand hygiene policies. Similar hand hygiene compliance rates have been reported by INICC (International Nosocomial Infection Control Consortium) in Peru, which were found to range from 20% to 70% [29].
Since, 9 out of 20 (45%) were not true infections, more emphasis should be placed on the standardized guidelines of the sample collection and diagnosis, as was done in the UTI supervision programme. The UTI supervision program which was initiated in July 2009 was successful in bringing down the CAUTI rates in August itself and also thereafter. In spite of all these efforts, the rates rose in September and November to 7.4 and 7.9 respectively. The reason for this may be the patient related factors, as all the patients belonged to the high risk category. Similar results were obtained by Tom J Blodgett et al., [30] in 2009, upon the introduction of the intervention, which resulted in a failure in reducing the CAUTI rates, for which the author proposed methodological flaws as the possible reason for these rates. Another issue of concern which was addressed in the supervision program was the need for catheterization. A study on this aspect indicated that before the introduction of the supervision program, the insertion of a catheter was justified in 14 out of 20 (70%) cases and that after the program, it was justified in 10 out of 14 (71.4%) cases. This clearly showed that even after the supervision program, there was no decrease in the number of patients who had an indwelling catheter and therefore, changing the mindsets of the clinicians was a slow process, which would require further training. From within the bundle, it was observed that bladder irrigation and practising perineal cleaning thrice a day had no observable effects on the development of the infections. However, training of the staff, urinary catheter checklist adherence, hand hygiene compliance and avoiding the urine reflux were important measures which had to be taken. Evidences from earlier studies suggested there was no benefit of the bladder irrigation in patients who had indwelling or intermittent catheters [31,32]. Similarly, maintaining routine hygiene in the catheterized patients (e.g., cleansing of the meatal surface during daily bathing) is recommended instead of repeated antiseptic meatal cleaning regimens during the maintenance of the catheter, to prevent CAUTIs [2,33,34].
*Candida is not processed for sensitivity in urine specimens.
†Carbapenem Resistant strains.
‡Vancomycin Resistant Enterococci showing resistance to high level Gentamicin.
[1]. National Center for Health Statistics, Centers for Disease Control and Prevention, U.S. Dept. of Health and Human Services, September 2004. 13(157). Hyattsville, MD [Google Scholar]
[2]. Gould CV, Umscheid CA, Aggarwal RK, Kuntz G, Pegues DA, Healthcare Infection Control Practices Advisory Committee. Guideline for prevention of catheter-associated urinary tract Infections 2009 [Google Scholar]
[3]. Lo E, Nicolle L, Classen D, Strategies to prevent catheter associated urinary tract infections in acute care hospitalsInfection Cont and Hosp Epid 2008 29(1):s41-50. [Google Scholar]
[4]. Centers for Disease Control and Prevention (CDC)Emerging InfectiousDiseases Posted; Emerging Infectious Diseases 2001 7(2)©2001 [Google Scholar]
[5]. Weinstein MP, Towns ML, Quarterly SM, Clinical significance of positive blood cultures in the 1990s: A prospective comprehension evaluation of the microbiology, epidemiology and the outcome of the bacteremia and fungemia in adultsClin Infect Dis 1997 24(4):584-602. [Google Scholar]
[6]. Tambyah PA, Halvorson KT, Maki DG, A prospective study on the pathogenesis of catheter-assosiated urinary tract infectionsMayo Clin Proc 1999 74(2):131-36. [Google Scholar]
[7]. Saint S, Chenoweth CE, Biofilms and catheter-associated urinary tract infectionsInfect Dis Clin North Am 2003 17(2):411-32. [Google Scholar]
[8]. Stark RP, Maki DG, Bacteriuria in the catheterized patientN Engl J Med 1984 311:560-64. [Google Scholar]
[9]. Maki DG, Nosocomial bacteremia. An epidemiologic overviewAm J Med 1981 70:719-32. [Google Scholar]
[10]. Krieger JN, Kaiser DIL, Wenzel RP, The urinary tract etiology of the bloodstream infections in hospitalized patientsJ Infect Dis 1983 148:57-62. [Google Scholar]
[11]. Maki* Dennis G, Tambyah† Paul A, Engineering Out the Risk for Infection with Urinary CathetersEm Infect Dis 2001 March–April7(2):342-47. [Google Scholar]
[12]. http://www.cdc.gov/nhsn/pdfs/pscManual/7pscCAUTIcurrent.pdf (Accessed on 4 March 2009) [Google Scholar]
[13]. Umscheid C, Mitchell M, Agarwal R, Williams K, Brennan P, The mortality from reasonably-preventable hospital acquired infections which was included in written testimony by the Society of Healthcare Epidemiology of America for the committee on oversight and government reform hearing on healthcare-associated infections: A preventable epidemicchaired by Henry A. Waxman, April 16, 2008, Washington DC, [Congressional testimony] [Google Scholar]
[14]. Collee JG, Miles RS, Collee JG, Duguid P, Fraser AG, Marmion BP, Mackie McCartney Tests for the identification of bacteriaPractical Medical Microbiology 1989 13th edn:141-60. [Google Scholar]
[15]. Stephan F, Sax H, Wachsmuth M, Hoffmeyer P, Clergue F, Pittet D, Reduction of urinary tract infections and antibiotic use after surgery: A controlled, prospective, before-after intervention studyClin Infect Dis 2006 42(11):1544-51. [Google Scholar]
[16]. Jain M, Miller L, Belt D, King D, Berwick DM, Decline in the ICU adverse events, nosocomial infections and cost through a quality improvement initiative focusing on teamwork and culture changeQual Saf Health Care 2006 15(4):235-39. [Google Scholar]
[17]. Madani N, Rosenthal V, Dendane T, AbidiAmine K, Zeggwagh A, Abouqal R, Intravenous literature: Health-care associated infections rates, length of stay, and bacterial resistance in an intensive care unit of Morocco: Findings of the International Nosocomial Infection Control Consortium (INICC)International Archives of Medicine 2009 2:29 [Google Scholar]
[18]. Jordan S, Pogorzelska M, Larson E, Stone P W, The range of policies for the prevention of catheter associated UTIs in Intensive care unitsNew YorkColumbia University School of Nursing [Google Scholar]
[19]. Allegranzi B, Pittet D, Inaugural infection control webinar series: The global burden of health care-associated infections 2010 January19Geneva, SwitzerlandWHO Patient Safety Day [Google Scholar]
[20]. Talaat M, Hafez S, Saied T, Elfeky R, El-Shoubary W, Pimentel G, Surveillance of catheter-associated urinary tract infections in 4 intensive care units at the Alexandria university hospitals in EgyptJournal? 2010 April38(3):222-28. [Google Scholar]
[21]. Kang SC, Hsu NW, Tang GJ, Hwang SJ, The impact of urinary catheterization on geriatric inpatients with community-acquired urinary tract infections 2007 70(6):236-40. [Google Scholar]
[22]. Hussain M, Oppenheim P, O’Neill C, A prospective survey on the incidence, risk factors and the outcome of hospital-acquired infections in the elderlyJournal of Hospital Infection 1996 32:117-26. [Google Scholar]
[23]. Tuschida T, Makimoto K, Yoshida S, Ohsako S, The relationship between catheter care and catheter-associated urinary tract infection at Japanese acute care hospitalsAmerican Journal of Infection Control 2005 33(5):e177-78. [Google Scholar]
[24]. Surveillance of Catheter Associated Urinary Tract Infections Annual Report June 2005, Scottish Surveillance of Healthcare Associated Infection Programme [Google Scholar]
[25]. Garibaldi RA, Burke JP, Dickman ML, Smith CB, Factors which predispose to bacteriuria during indwelling urethral catheterisationThe New England Journal of Medicine 1974 291:213-19. [Google Scholar]
[26]. Swihart K.G., Welch R.A., The HpmA hemolysin is more common than HlyA among the Proteus isolatesInfect. Immun. 1990 58:1853-60. [Google Scholar]
[27]. Jha N, Bapat SK, A study on the sensitivity and resistance of the pathogenic microorganisms which caused UTIs in the Kathmandu valleyKathmandu Univ Med J 2005 3:123-29. [Google Scholar]
[28]. Winters BD, Gurses AP, Lehmann H, Sexton JB, Rampersad CJ, Pronovost PJ, Clinical review: Checklists – translating evidence into practiceCritical Care 2009 13:210 [Google Scholar]
[29]. Rosenthal VD, Salomao R, Leblebicioglu H, Akan O, Sobreyra-Oropeza M, Hand hygiene compliance in Argentina, Brazil, Colombia, India, Mexico, Morocco, Peru and Turkey. Findings of the International Nosocomial Infection Control Consortium (INICC)Proceedings and Abstracts of the 33rd Annual Scientific Meeting of the Association for Professionals in Infection Control and Epidemiology11-15 June 2006Tampa, Florida, U.S.A.:31 [Google Scholar]
[30]. Blodgett JT, Reminder systems to reduce the duration of indwelling urinary catheters: a narrative reviewUrologic Nursing 2009 29(5) [Google Scholar]
[31]. Schneeberger PM, Vreede RW, Bogdanowicz JF, van Dijk WC, A randomized study on the effect of bladder irrigation with povidone-iodine before the removal of an indwelling catheterJ Hosp Infect 1992 21(3):223-29. [Google Scholar]
[32]. Warren JW, Platt R, Thomas RJ, Rosner B, Kass EH, Antibiotic irrigation and catheter-associated urinary-tract infectionsN Engl J Med 1978 299(11):570-73. [Google Scholar]
[33]. Huth TS, Burke JP, Larsen RA, Classen DC, Stevens LE, Randomized trial of the meatal care with silver sulfadiazine cream for the prevention of catheter-associated bacteriuriaJ Infect Dis. 1992 165(1):14-18. [Google Scholar]
[34]. Burke JP, Jacobson JA, Garibaldi RA, Conti MT, Alling DW, Evaluation of the daily meatal care with poly-antibiotic ointment in the prevention of urinary catheter-associated bacteriuriaJ Urol 1983 129(2):331-34. [Google Scholar]