Rupia derives its etymological roots from the Greek word “Rhupos,” meaning dirt. “Rupioid” describes distinct, cone-shaped plaques with dense, dark, lamellate, and adherent crusts on the skin, resembling oyster or limpet shells. Rupioid psoriasis, a morphological subtype of plaque psoriasis characterised by hyperkeratotic lesions, is a prevalent dermatological condition affecting approximately 2.5% of the global population. Given its autoimmune nature, psoriasis lacks a definitive cure. Its clinical features are similar to those observed in Kitibha Kushtha, a type of MahaKushtha (major skin disease) in Ayurveda. The treatment approach involves purificatory therapies alongside internal medicine. This case report details a 46-year-old male patient who presented with symptoms of rupioid psoriasis for eight years. The patches thickened and gradually darkened to a blackish hue. The itching intensified gradually. The intervention included purificatory therapies, emesis, and purgation, followed by internal medicine and topical application. The combination of purificatory therapies, followed by external and internal administration of Ayurvedic formulations, proved highly effective in managing the patient’s KitibhaKushtha (rupioid psoriasis).
Case Report
A 46-year-old male healthcare provider presented to the institutional outpatient department complaining of hard, crust-like skin lesions and wounds on both forearms, accompanied by itching for eight years. The condition gradually spread to his hands, trunk, and back. The patches turned a blackish hue, and the itching worsened, particularly at night. The patient initially consulted a homeopathy clinic without relief. He subsequently attended the dermatology department of a tertiary hospital, where a biopsy was recommended. Due to the patient’s refusal of histopathology, a diagnosis of rupioid psoriasis was made based on clinical presentation. The patient received treatment with methotrexate, cetirizine, and folic acid, along with topical steroids, for three months under the care of a dermatologist, providing temporary relief. New lesion formation ceased during treatment, but the condition relapsed upon cessation of medication. He then sought care at an Ayurvedic hospital. The patient had no significant past history of rupioid psoriasis or other skin problems, and no family history was reported. He maintained a mixed diet (vegetarian and non-vegetarian), experienced sleep disturbance due to itching, and had no harmful habits (Vyasan). On examination, the patient’s vital signs were normal. His pulse was 80 beats per minute and regular, with a blood pressure of 120/90 mmHg (Vata Kaphaj). Respiratory rate was 18 breaths per minute, and temperature was normal (98.2°F). Ashtavidha Pariksha (eight diagnostic tools) revealed normal findings except for Malabaddhata (constipation); his tongue (Jivha) was Saam, and his skin (Sparsha) was Khar with Raktawarna. He also exhibited Kshudhamandya (impaired digestion). Dermatological examination revealed multiple, well-demarcated, raised, black lesions with thick, lamellate, and adherent crusts on both hands. The diagnosis was made by comparison with other conditions exhibiting similar features [Table/Fig-1].
Showing differential diagnosis.
| Kapala Kushtha | Eka Kushtha | Kitibha Kushtha |
|---|
| Krushna Arun (Blackish reddish discolouration) | Aswedana means Dry and rough lesions | Shavya Varna (blackish brown colour) |
| Kapalabham (Skin resembles same as a piece of the earthen pot) | Mahavastu, which encompasses the entire body | Kin KharaParusham (hard to touch or Rough like scar tissue similar to the granulation process in wound |
| Yadruksham (Dryness) | Matsyashakalawat consists of well-demarcated raised patches with large, silvery, loose scaling, causing the skin to resemble fish scales |
| Parusham (Hard plaques) | Krishna-ArunaVarnata means Erythematous, black |
| Tanu (Thin) |
| Vishamakar (irregular borders) |
| Todabahulam (Pricking type of pain) |
Assessment criteria: The Psoriasis Area Severity Index (PASI) score [Table/Fig-2] was used to assess severity [1]. The scale ranges from 0 to 4, representing no severity to maximum severity. The body is divided into four sections: head (H) (10% of the skin), arms (A) (20%), trunk (T) (30%), and legs (L) (40%). Each section is scored individually, and the scores are combined to determine the final PASI score. For each section, the percentage of skin area involved is estimated and graded from 0 to 6. Based on erythema, induration, and desquamation, the patient initially scored 4 on the PASI scale.
Displaying area involved with grading.
| % of occupied area | Grades |
|---|
| 0%- occupied area | Grade 0 |
| <10% involved area | Grade 1 |
| 10-29% occupied area | Grade 2 |
| 30-49% occupied area | Grade 3 |
| 50-69% occupied area | Grade 4 |
| 70-89% occupied area | Grade 5 |
| 90-100% occupied area | Grade 6 |
Treatment: Treatment commenced with Gandhak Rasayan, Avipathikar Churna, Vetapalai Oil, and Padachira Ointment, along with Panchatikta Ghrita and Trikatu Churna as preparation for Shodhan Karma. Shodhana Chikitsa (purificatory therapy) involved sequential Vamana (emesis) and Virechana (purgation) as part of Purvakarma, Pradhankarma, and Paschatkarma. Purgation was performed 20 days after emesis.
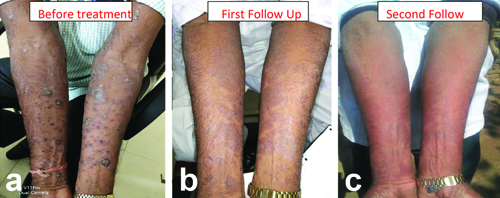
Follow-up and outcome: Following Vamana, erythema, induration, and desquamation scores reduced to 1, 2, and 2, respectively. After Shodhan, Shaman Chikitsa was administered [Table/Fig-3]. A second follow-up after Vamana and Virechana showed further reduction to 0 for these symptoms [Table/Fig-4,5]. Pre-Shodhana procedures, formulations, doses, drugs, and properties are detailed in [Table/Fig-6,7,8 and 9]. Vamana involved 2600 mL intake and 3200 mL output with nine vega; Virechana resulted in expulsion of Pitta dosha with twenty-four vegas [Table/Fig-10].
Shows formulations of Shaman Chikitsa.
| S. No. | Formulations | Contents | Dose and Anupan (vechicle) | Duration |
|---|
| 1. | Gandhak Rasayan | Purified Sulphur powder, Phyllanthus Emblica Bhringaraj (Ecliptidca Alba), Haritaki (Terminalia-Chebula) Terminalia belerica, Guduchi (Tinospora- cordifolia) | 500 mg BD (Twice a day) after meal | For 15 days |
| 2 | Avipattikar Churna | Amla (Emblica officinalis) Cardamom (Elettaria- cardamomum) Behada (Terminalia- belerica) Clove (Syzygium aromatic) Ginger (Zingiber officinale) Turpeth (Operculinatur pethum) Long pepper (Piperlongum) Haritaki (Terminalia chebula) Black pepper (Piper nigrum) Nutgrass (Cyperus rotundus) Indian bay leaf (Cinnamomum tamala) Vidanga (Embelia ribes)
| 3 grams
Two times/day, empty stomach |
| 3 | Vetapalai
Thailam | Wrightia tintoria,
Cocos nucifera | External application |
| 4 | Padachira Ointment | ShudhaTurti (alum), Ghruta (Clarified butter), Kapur (Camphor), Rai (Mustard seed), ShudhaChuna (Lime), ShudhaSuvarnaGarik (Slicate of alumina), Kokamoil (Garcinia
indica) KaduNimb oil (Azadirachta indica) | External Application |
| 5 | Skin Powder | Haridra (Curcumalonga),
Amalaki (Phyllanthus - emblica),
Behada (Terminaliabellirica), ShudhaGandhaka (Purified Sulphur) Nagarmotha (Cyperusrotundus) Manjistha (Rubia-cordifolia) | External Application |
a) presence of darker lesions on forearms; b) 1st Follow up image showing no lesions only scars remain; c) On 2nd Follow-up showing healed lesions and scars.
Displaying assessment of parameters.
| S. No. | Signs and symptoms | Before treatment | Follow-up after Vamana | Follow-up after Virechana |
|---|
| 1 | Erythema (redness) | Grade 4 | Grade 1 | Grade 0 |
| 2 | Induration (thickness) | Grade 4 | Grade 2 | Grade 0 |
| 3 | Desquamation (scaling) | Grade 4 | Grade 2 | Grade 0 |
Dose, anupan, route, and time of taking medicine in pre-procedure.
S.
No. | Name of formulation | Dose
(Vamana) | Dose
(Virechana) | Route | Duration | Anupam |
|---|
| 1 | Trikatu-Churna (1) | 3 gram | 3 gram | Oral | 1/day empty stomach | Warm water |
| 2 | Panchatikta Ghrita (2) | On 1st day 30 mL, then increase by 30 mL per day up to 6th day
On 6th day- 180 mL is given | On 1st day, 30 mL, then increase by 30 mL per day till the 7th day on
7th day, 220 mL is given | Oral | Early morning | Warm water |
| 3 | SarvangaSnehan (Body Massage) with Tail (Marichadi)
Sarvanga
Swedan | | Two days before and on the day of Virechana | External application | One day before and on the day of Vamana therapy | -- |
Ingredients and properties of the formulations used in Purvakarma (Deepan, Pachan, Abhyanga, and Swedana).
| S. No. | Name of
medicine | Contains | Properties and use |
|---|
| 1. | Trikatu-churna | Sunth (Zingiber officinale) Pippali (Piper longam), Marich (Piper nigrum) | Agnideepan |
| 2. | Panchatiktaghrita (Snehapan) | Patol (Luffaacutangula), (Adhatoda vasica), Neem (Azardirachta indica), Vasa Vyaghari (Solanum xanthocarpum), Guduchi (Tinospora cordifolia), and ghee | Dipana, Pachana, Amapachaka, Raktaprasadan Raktashodhaka, Strotoshodhaka, Kandughna, Varnya
Kushthaghna |
| 3. | Marichaditail (Abhyanga) | Marich (Piper nigrum), Nagarmotha (Cyperus rotundus), Gorasa, Indrayanamula (Citrullus cococynthis), Arkadugdha (Calotrpis procera), Raktachandana (Pterocarpus santalinus), Vatsanabha (Aconitum ferox), Kaneramulatwak (Neriumindicum), Haridra (Curcuma longa), Devdaru (Cedrus deodara), Nishoth (Operculi Nipomoca), Manahshila, Kushtha (Saussurea lappa), Daruharidra (Berberis aristata), Hartaal, Sarshaptail (Brassica alba) | Raktashodhak, Vranropak, and Twachya benefit Dadru, Shwitra, and all types of Kushtha |
Ingredients and properties of the drugs used in Vaman Karma.
| S. No. | Name of ingredients | Latin name | Dose | Properties |
|---|
| 1 | Madan-phala powder | Randiadumetorum | 3 gm | Vamanopag |
| 2 | Honey | - | 25 mL | Abhishyandi, Yogavahi |
| 3 | SaindhavLavan | Rock-Salt | 5 grams | Shodhak |
| 4 | Vacha powder | Acorus Calamus | 5 gm | Vamanopag |
| 5 | Yashtimadhuphant | Glycyrrhizaglabra | 1000 mL | Vamanopag |
| 6 | Milk | - | 2500 mL | Vamanopag |
Ingredients and properties of drugs used in Virechana Karma.
S.
No. | Name of
ingredients | Latin name | Dose | Properties |
|---|
| 1. | Triphala Kwath | Haritaki (Terminalia chebula), Amalaki (Emblica
Officinalis) Vibhitaki (Terminaliabellirica) | 160 mL | Purgative |
| 2. | Katuki Churna | Picrorhizakurroa | 25 g | Vishamajwara, Daha, Kusta, Krimi, Hridroga, Pandu, Grahani and Arochaka |
| 3. | Trivrit Churna | Operculina-turpethum | 30 gm | Purgation, constipation, oedema, liver health, arthritis, and osteoarthritis. Anti-diabetic, anti-inflammatory, and blood purification |
| 4. | Ichchabhedi Rasa | | 250 mg tablet | Ascites, constipation |
Virechana procedure done with 24 vega as Madhyam Shudhi
Assessment of Samyaka Vamana and Virechana.
| S. No. | Measurement intake and output | Procedural inference | No. of Vega | Symptoms |
|---|
| Vamana | 2600 mL
3200 mL | Pittantak
Vamana | 9 | Kaphachadrika was present in the vomitus, with no bleeding observed |
| Virechana | 160 mL+25 g+30 gm+250 mg (1 tablet) | Pintantak | 24 | Daurbalyam (weakness), Laghavam (feeling of lightness), HridShuddhi (clarity in thoracic region), Vyadhinamanuta or Anaamayatvam (subsidence of disease), VarnaShuddhi (improved complexion) Glani (fatigue) |
Discussion
Rupioid psoriasis is a unique form of psoriasis characterised by distinctive lesions. Unlike other psoriasis types, it presents with cone-shaped, thick, crusted black lesions, and patients exhibit periods of remission. Few infectious aetiologies are relevant to the differential diagnosis of rupioid presentations. These include syphilis, HIV, scabies, histoplasmosis, Rupioid Psoriasis (RupP), and reactive arthritis. Diagnosis is based on Kushta symptoms. Eka Kushta presents with dry skin and lesions covering the entire body. KapalaKushta features black, hard, dry plaques resembling an earthen pot. Kitibha Kushtha presents with black-brown lesions that are hard to the touch, similar to wounds. Based on these symptoms, this case was diagnosed as Kitibha Kushtha, correlating with rupioid psoriasis due to similar signs and symptoms. Ayurvedic research has addressed erythrodermic psoriasis, plaque psoriasis, and scalp psoriasis using Shodhan Karma [2,3]. However, no case studies specifically address rupioid psoriasis treated with Shodhan and Saman Chikitsa in Ayurveda. Therefore, based on the presented findings, the diagnosis was Kitibha Kushtha and Shodhan followed by Shaman Chikitsa was recommended.
Shodhan Chikitsa: Before purificatory therapies, Purva karma improved digestion. Pradhan karma, involving Vamanopag Dravyas (drugs used in emesis therapy), works at a microcellular level, aiding detoxification, improving immunological function, and preventing recurrence. After Shodhan Karma, Dhoomapan was administered via Aguru (Aquilaria agallocha Roxb) stick in each nostril for five minutes. Sansarjana Karma (post-detoxification diet) was prescribed for five days. The post-Vamana and Virechana dietary regimen enhanced Jatharagni (digestive capacity), replenishing Jatharagni in the stomach and intestines and gradually enhancing acid and alkaline secretions. The regimen included Vilepi, Akrita Mamsarasa, Peya Krita Yusha, Akrita Yusha, and Krita Mamsaras.
In Virechana, the drug properties facilitated expulsion of morbid factors via the anal route due to the predominance of Jala, Prithvi Mahabhuta, and Adhobhaga Prabhava.
Internal medicine included Panchatikta Ghrita (Snehapan) containing Patol (Luffa acutangula), Neem (Azadirachta indica), Vyaghri (Solanum xanthocarpum), Vasa (Adhatoda vasica), Guduchi (Tinospora cordifolia), and ghee. It acts as a digestive stimulant, cleanser of bodily channels, blood purifier, antipruritic, anti-dermatitis agent, and complexion enhancer [4]. Gandhak rasayan, a widely recommended formulation for skin diseases, possesses antibacterial, antiviral, and antimicrobial properties. Purified sulphur reduces infection and alleviates itching, improving skin complexion and aiding digestion. Sulphur is administered orally and topically as a blood purifier, mitigating burning sensations (Daha) and itching (Kandu). The formulation is Raktashodhak (blood-purifying), Vranaropak (wound-healing), Twachya (skin-friendly), and Krumighna (antiparasitic), reducing infection and alleviating Raag (redness) and Pidika (eruption) [5].
Topical application: Padachira Ointment moisturises and softens the skin. Vetapalai oil possesses Kushthaghna (skin disease reducing) properties, being antibacterial, antiviral, anti-inflammatory, antifungal, and antimicrobial. It manages itching, pruritus, and psoriasis, improving digestion, skin complexion, and acting as a painkiller and wound healer. All constituents hydrate the skin and exhibit Tridosha (three humours reducing) properties [6]. Skin powder possesses antiviral, antibacterial, and antifungal properties, treating skin diseases, reducing infection and itching, and lessening Daha (burning sensation) and Kandu (itching). It is also blood-purifying, wound-healing, skin-friendly, and antiparasitic [7].
Conclusion(s)
Rupioid psoriasis correlates with Kitibha Kushtha, a Maha Kushtha subtype. Effective treatment involves Shodhana procedures (Vamana and Virechana), followed by Shaman Chikitsa, including Gandhaka Rasayan and topical application of Vetapalai oil, Padachira ointment, and skin powder. The synergistic effect of Shodhana Chikitsa and Shaman Aushadhi yielded improved outcomes.
Virechana procedure done with 24 vega as Madhyam Shudhi
[1]. Jacobson CC, Kimball AB, Rethinking the psoriasis area and severity index: The impact of the area should be increasedBr J Dermatol 2004 151(2):381-87.10.1111/j.1365-2133.2004.06035.x15327545 [Google Scholar] [CrossRef] [PubMed]
[2]. Sharma D, Garg I, Yadav S, Effect of ayurveda interventions in the management of chronic plaque psoriasis: A case reportInternational Research Journal of Ayurveda & Yoga 2023 6(7):43-50.Available from: https://doi.org/10.48165/IRJAY.2023.670710.47223/IRJAY.2023.6707 [Google Scholar] [CrossRef]
[3]. Abhilesh VS, Prathibha CKB, Anandaraman PVS, Management of erythrodermic psoriasis through ayurveda - A case reportPerm J 2021 25:20.22110.7812/TPP/20.22135348057PMC8784040 [Google Scholar] [CrossRef] [PubMed]
[4]. Yadavji Trikamji Achary, Agnivesha, Charaka Samhita, Ayurveda Deepika commentary of Chakrapani 2019 VaranasiChoukhamba Surabharati PrakashanChikitsa Sthana 13 chapter; verse 14, Reprint [Google Scholar]
[5]. Kaushik H, Tomar BS, Chawla SK, Role of gandhak rasayan in kshudra kushtha - A review articleJ Ayurveda Integr Med Sci 2024 9(3):168-72.10.21760/jaims.9.3.25 [Google Scholar] [CrossRef]
[6]. Lalitha K, Chandrasekar R, Muthukumar R, Mathukumar S, Christian J, Elansekaran S, An integrated approach of Psoriasis in the light of Siddha and Ayurveda- A clinical case reportBiomedicine 2023 43:1353-56.10.51248/.v43i4.2362 [Google Scholar] [CrossRef]
[7]. Deshmukh SG, Thakre TI, Approach towards kushta (psoriasis) with ayurveda - A case studyInt J Res Pharm Sci 2020 11(4):5546-54.10.26452/ijrps.v11i4.3189 [Google Scholar] [CrossRef]