Management of Parastomal Hernia using Laparoscopic Keyhole Mesh Repair: A Case Report
Pushkar Galam1, Parin Nilesh Patel2, Dakshayani Satish Nirhale3, Kishore Jeughale4, Siddharth Veerla5
1 Assistant Professor, Department of General Surgery, Dr. D. Y. Patil Medical College and Hospital, Pune, Maharashtra, India.
2 Junior Resident, Department of General Surgery, Dr. D. Y. Patil Medical College and Hospital, Pune, Maharashtra, India.
3 Head, Department of General Surgery, Dr. D. Y. Patil Medical College and Hospital, Pune, Maharashtra, India.
4 Associate Professor, Department of General Surgery, Dr. D. Y. Patil Medical College and Hospital, Pune, Maharashtra, India.
5 Junior Resident, Department of General Surgery, Dr. D. Y. Patil Medical College and Hospital, Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Parin Nilesh Patel, 31, Royal Enclave Behind Zydus Hospital, Thaltej, Ahmedabad-380059, Gujarat, India.
E-mail: daringparin@gmail.com
Parastomal Hernia (PSH) is a frequent and challenging complication of stoma creation, with an incidence of up to 50% within two years postsurgery. This condition often presents with swelling, discomfort, or complications such as obstruction or strangulation. Surgical repair, particularly using minimally invasive techniques, is the definitive treatment for symptomatic or complicated hernias. This case report presents a 65-year-old female with a symptomatic PSH following anterior perineal resection and colostomy for rectal cancer. The hernia was successfully managed with a laparoscopic keyhole mesh repair. The procedure involved meticulous adhesiolysis and the placement of a composite mesh to reinforce the abdominal wall while maintaining stoma function. Postoperative recovery was uneventful, and the patient experienced complete symptom resolution with no recurrence at the one-month follow-up. This report underscores the efficacy and safety of laparoscopic keyhole mesh repair in the management of PSH and highlights the importance of individualised surgical planning and precision in achieving optimal outcomes.
Adhesiolysis, Colostomy, Laparoscopic surgery
Case Report
A 65-year-old female presented with intermittent colicky pain for one year and swelling around the colostomy site, which had an insidious onset and was gradually progressive. The swelling increased with walking and reduced when lying down over the past year. The patient was a known case of moderately differentiated rectal cancer, diagnosed three years earlier, and had undergone anterior perineal resection with the creation of a colostomy. She was also a known case of hypertension, taking Telmisartan 40 mg once daily for the last 15 years. Over the past year, she experienced reduced appetite and symptoms of indigestion.
On examination, the patient was moderately built and nourished, with a Body Mass Index (BMI) of 27.6 kg/m2 and all other vital parameters were within normal limits. Local examination revealed a spherical swelling extending 2 cm lateral to the umbilicus and 2 cm medial to the anterior superior iliac spine around the colostomy site. Inferiorly, it extended up to 4 cm above the pubic tubercle. The swelling was soft, non tender and reducible in the supine position. It became prominent on coughing or performing a straight leg raising test. The colostomy itself was healthy and functional, without signs of infection or ischaemia [Table/Fig-1,2].
Preoperative image showing a spherical swelling around the colostomy site in the supine position.

Preoperative image showing the increased size of the swelling in standing position.

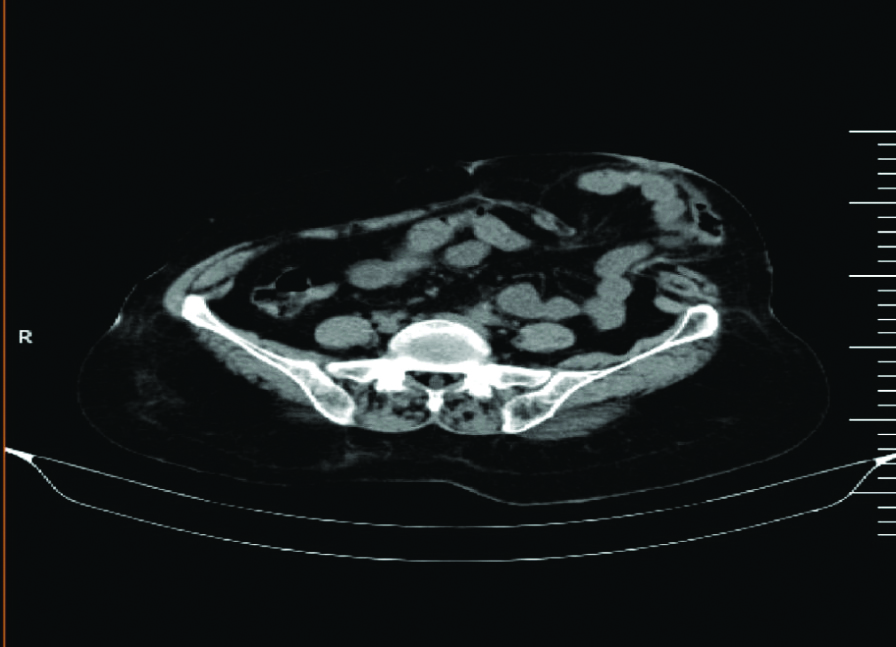
Further imaging studies were conducted to confirm the diagnosis. A contrast-enhanced Computed Tomography (CT) scan of the abdomen and pelvis demonstrated herniation of the descending colon and a substantial segment of the small bowel, along with mesentery, through a parastomal defect measuring 58×54 mm. There were no signs of bowel obstruction, strangulation, or ischaemia [Table/Fig-3]. Based on the clinical and radiological findings, a diagnosis of symptomatic PSH was established. After discussing the risks, benefits and alternatives with the patient, a laparoscopic repair using a keyhole mesh technique was planned.
CT abdomen and pelvis showing herniation of bowel through parastomal defect.
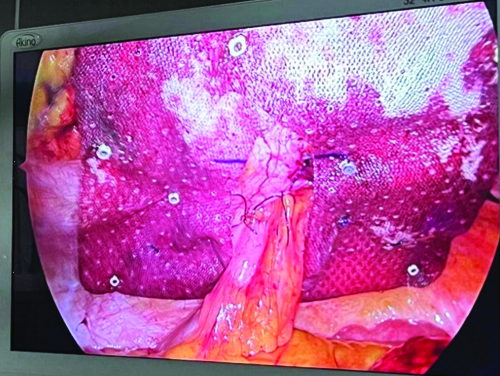
The patient was positioned supine under general anaesthesia. Pneumoperitoneum was established and laparoscopic ports were placed strategically for optimal visualisation and access to the parastomal region. Intraoperatively, extensive Grade 4 adhesions were encountered between the bowel loops, omentum and the anterior abdominal wall near the stoma. These adhesions were carefully lysed to ensure bowel safety and to facilitate adequate mesh placement. A composite mesh measuring 15×15 cm was prepared by creating a keyhole to accommodate the stoma. The mesh was positioned around the stoma and fixed circumferentially using prefixed sutures. The keyhole defect in the mesh was closed with barbed sutures to prevent future herniation through the mesh [Table/Fig-4]. Haemostasis was meticulously achieved and the abdomen was desufflated. No intraoperative complications occurred.
Intraoperative image showing keyhole mesh repair around the stoma.
The patient had an uneventful postoperative recovery. She was mobilised on the first postoperative day and resumed a liquid diet, which was gradually advanced. The colostomy remained functional throughout the postoperative period. The patient was stable when discharged on postoperative day three. At the one-month follow-up, the patient reported complete resolution of preoperative symptoms [Table/Fig-5]. Clinical examination revealed no hernia recurrence and the colostomy site was intact, without signs of infection or inflammation. The patient expressed satisfaction with the surgical outcome and reported a significant improvement in her quality of life.
Postoperative image after one month.

Discussion
PSH presents a significant challenge in the postoperative care of colostomy patients. The development of PSH is influenced by patient-related factors, including age, obesity and chronic conditions, as well as surgical factors such as the size, placement and surgical technique of the stoma [1]. The hernia in this case likely developed due to increased intra-abdominal pressure and the natural weakening of the abdominal wall around the stoma.
Management of PSH is based on the severity of symptoms and the presence of complications. While conservative approaches may be directed toward symptomatic relief only, they do not address the defect itself and are usually reserved for asymptomatic patients. Surgical intervention, on the other hand, offers a definitive repair and prevents progression into complications such as obstruction or strangulation [2,3].
Laparoscopic repair has gained traction among surgical options due to its minimally invasive nature and superior outcomes compared to open techniques. The keyhole mesh technique is particularly advantageous in managing PSH. It involves the use of a composite mesh designed to minimise adhesion formation and promote tissue integration. By creating a central opening (keyhole) to accommodate the stoma, the technique ensures robust reinforcement around the stoma while maintaining its functionality [4]. Previous reports have highlighted the efficacy of laparoscopic repair in reducing recurrence rates and postoperative complications compared to open repair. Salvilla SA et al., conducted a meta-analysis of observational studies and observed a decreased rate of hernia recurrence with laparoscopic treatment as opposed to open repair [5]. Another meta-analysis by DeAsis FJ et al., noted that laparoscopic mesh repair is both safe and effective in treating PSH [6]. In present case, the successful application of the keyhole mesh technique aligns with these findings, reinforcing its role as a reliable approach.
Despite the documented benefits, challenges remain, particularly in patients with extensive adhesions or large hernia defects. This case underscores the importance of meticulous adhesiolysis to facilitate mesh placement and prevent bowel injury. Similar challenges were reported by Berger D and Bientzle M, who noted that advanced laparoscopic skills are critical for managing such complexities [7].
Postoperative outcomes in this patient were excellent, with complete resolution of symptoms, no evidence of recurrence and significant improvement in quality of life. These results are consistent with the findings of Byrd JF et al., who highlighted the long-term benefits of composite mesh in minimising adhesion-related complications and ensuring durable repairs [8]. However, long-term follow-up is crucial to monitor for recurrence, which remains a concern in hernia repairs. Factors such as surgical expertise, patient compliance with postoperative care and lifestyle modifications play pivotal roles in achieving durable outcomes. Comparative analyses of outcomes across different repair techniques could further refine management strategies for PSH.
Conclusion(s)
Laparoscopic repair using the keyhole mesh technique is an effective and safe approach for managing symptomatic PSH. This case emphasises the timeliness of intervention and the potential benefits of minimally invasive techniques on patients’ outcomes and quality of life.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 21, 2025
Manual Googling: Feb 27, 2024
iThenticate Software: Mar 01, 2025 (2%)
[1]. Manole TE, Daniel I, Alexandra B, Dan PN, Andronic O, Risk factors for the development of parastomal hernia: A narrative reviewSaudi J Med Med Sci [Internet] 2023 11(3):187-92.Available from: https://dx.doi.org/10.4103/sjmms.sjmms_235_2210.4103/sjmms.sjmms_235_2237533654PMC10393091 [Google Scholar] [CrossRef] [PubMed]
[2]. Luan L, Liu Q, Cui C, Cheng Y, Zhang G, Li B, Surgical treatment strategy for recurrent parastomal hernia: Experiences from 17 casesFront Surg [Internet] 2022 9:928743Available from: https://dx.doi.org/10.3389/fsurg.2022.92874310.3389/fsurg.2022.92874335983552PMC9379134 [Google Scholar] [CrossRef] [PubMed]
[3]. Mizrahi H, Geron N, Parker MC, Parastomal hernia is a problem yet to be solvedJ Curr Surg [Internet] 2015 5(2-3):151-56.Available from: https://dx.doi.org/10.14740/jcs268w10.14740/jcs268w [Google Scholar] [CrossRef]
[4]. Gillern S, Bleier JIS, Parastomal hernia repair and reinforcement: The role of biologic and synthetic materialsClin Colon Rectal Surg [Internet] 2014 27(4):162-71.Available from: https://dx.doi.org/10.1055/s-0034-139409010.1055/s-0034-139409025435825PMC4226750 [Google Scholar] [CrossRef] [PubMed]
[5]. Salvilla SA, Thusu S, Panesar SS, Analysing the benefits of laparoscopic hernia repair compared to open repair: A meta-analysis of observational studiesJ Minim Access Surg [Internet] 2012 8(4):111-17.Available from: https://dx.doi.org/10.4103/0972-9941.10310710.4103/0972-9941.10310723248436PMC3523446 [Google Scholar] [CrossRef] [PubMed]
[6]. DeAsis FJ, Lapin B, Gitelis ME, Ujiki MB, Current state of laparoscopic parastomal hernia repair: A meta-analysisWorld J Gastroenterol [Internet] 2015 21(28):8670-97.Available from: https://dx.doi.org/10.3748/wjg.v21.i28.867010.3748/wjg.v21.i28.867026229409PMC4515848 [Google Scholar] [CrossRef] [PubMed]
[7]. Berger D, Bientzle M, Laparoscopic repair of parastomal hernias: A single surgeon’s experience in 66 patientsDis Colon Rectum [Internet] 2007 50(10):1668-73.Available from: https://dx.doi.org/10.1007/s10350-007-9028-z10.1007/s10350-007-9028-z17680310 [Google Scholar] [CrossRef] [PubMed]
[8]. Byrd JF, Agee N, Nguyen PH, Heath JJ, Lau KN, McKillop IH, Evaluation of composite mesh for ventral hernia repairJSLS [Internet] 2011 15(3):298-304.Available from: https://dx.doi.org/10.4293/108680811X1307118040739310.4293/108680811X1307118040739321985713PMC3183537 [Google Scholar] [CrossRef] [PubMed]