Case Report
A 52-year-old non diabetic, non hypertensive male patient first presented in 2019 complaining of severe anorexia, evening rise of low-grade temperature up to 99.4°F, and 1.5 to 2 kg weight loss in the past few months with a current body weight of 52.4 kg. There was no history of chronic cough or haemoptysis, no family history of TB, or exposure to TB patients in the past. At that time clinical examination and laboratory investigations including sputum examination for AFB and GeneXpart revealed no significant findings. Viral serology for HIV and hepatitis B and C were also found to be non reactive. Chest X-ray shows no abnormalities. The patient was put on symptomatic management with oral antipyretic i.e., Paracetamol 500 mg twice daily and oral antibiotics i.e., Azithromycin 500 mg, once daily for five days. The symptoms were resolved eventually. The patient again presented with similar symptoms, three years after the first visit, around the same time of the year. He also gave a history of Coronavirus Disease-2019 (COVID-19) infection in between for which he was treated at home and subsequently received two doses of the Covishield vaccine. On general examination, there were no significant findings apart from mild pallor and laboratory examination was significant for anaemia with a haemoglobin level of 10.2 gm% along with raised Erythrocyte Sedimentation Rate (ESR) of 112 mm/hour and CRP of 144.8 mg/L. However, the patient was lost to follow-up [Table/Fig-1].
Haematological and biochemical parameters of the patient.
| Haematological and biochemical parameters | Values | Reference range |
|---|
| Haemoglobin (gm/dL) | 10.9 | 14-17 |
| Total leucocyte count (cells/mm3) | 8600 | 4,000-11,000 |
| Platelet count (lac cells/mm3) | 2.21 | 1.5-4.5 |
| RDW (%) | 15.3 | 11.5-14.5 |
| Peripheral blood smear | Normochromic and normocytic |
| ESR (mm/hour) at 1st hour | 52 | 0-15 |
| CRP (mg/dL) | 56.77 | Up to 6 |
| Blood Urea Nitrogen (BUN) (mg/dL) | 22.16 | 10-45 |
| Creatinine (mg/dL) | 0.87 | 0.6-1.2 |
| Lipase (IU/L) | 59.3 | Up to 90 |
| Amylase (IU/L) | 33.6 | Up to 60 |
| Total serum bilirubin (mg/dL) | 0.51 | 0-1 |
| SGOT (IU/L) | 22 | 0-37 |
| SGPT (IU/L) | 10.3 | 0-41 |
| Albumin (gm/dL) | 3.78 | 3.5-5.2 |
| Prothrombin Time (PT) (seconds) | 13.6 | 11-15 |
| INR | 1.15 | - |
| APTT (seconds) | 27.2 | 22-37 |
| Fasting blood glucose (mg/dL) | 87 | Less than 100 |
| Angitensonogen converting enzyme (U/L) | 41.8 | 8-52 |
| Alpha Feto Protein (AFP) (ng/mL) | 3.49 | 0-7 |
| CA-19.9 (U/mL) | 11.85 | Less than 39 |
| Carcino Embryonic Antigen (CEA) (ng/mL) | 3.68 | Less than 5 |
| LDH (U/L) | 253 | 230-460 |
| Calcium (mg/dL) | 7.78 | 8.5-10.2 |
| Vitamin D3 (ng/mL) | 18.9 | 30-100 |
| FT4 (ng/dL) | 1.42 | 0.8-2 |
| TSH (μIU/mL) | 2.95 | 0.3-4.5 |
| Anti-nuclear Antibody (ANA) (Au.mL) | 4.61 | Less than 25 |
| Anti-CCP (RU/mL) | 3.79 | Less than 10 |
| RA factor (IU/mL) | 18.6 | 0-20 |
| Stool calprotectin (μg/g) | 10.39 | Less than 50 |
RDW: Red cell distribution width; SGPT Serum glutamic-pyruvic transaminase; SGOT: Serum glutamic oxaloacetic acid transaminase; INR: International normalised ratio; LDH: Low-density lipid; RA: Rheumatoid arthritis; CA: Cancer antigen; FT4: Thyroxine free; Anti-CCP: Anti-cyclic citrullinated peptide
One year after the last visit the patient was once again presented with similar symptoms, around the same time of the year, but with a more severe form having visible weight loss of around 4 kg, cachexia, severe anorexia, along with similar evening rise of low-grade temperature accompanied by body aches and pain around bilateral wrist and ankle joint. On general examination, there were no significant findings except mild pallor and there was no lymphadenopathy. Wrist and ankle joints were found to be mildly tender. Systemic examination revealed no abnormal findings. On initial laboratory examination, the patient was found to be mild anaemic with a haemoglobin level of 9.9 gm% along with raised ESR of 95 mm/hour and CRP of 108.2 mg/L. RDW was within normal limits. Total leucocyte level was normal. Peripheral blood smear showed normochromic microcytic RBCs. Other biochemical work-ups including Blood Urea Nitrogen (BUN), creatinine, uric acid, liver function test, and thyroid function test were found to be within normal limits. Various auto-immune markers i.e., Rheumatoid (RA) factor, anti-CCP, and Anti-nuclear Antibodies (ANA) were found to be negative and ultrasonography of the wrist and ankle joint revealed no abnormality. Tumor markers such as CA 19.9, Alpha-fetoprotein (AFP), Carcinoembryonic Antigen (CEA), and LDH were also within normal limits except for a raised RA factor (44.1 IU/mL) [Table/Fig-1].
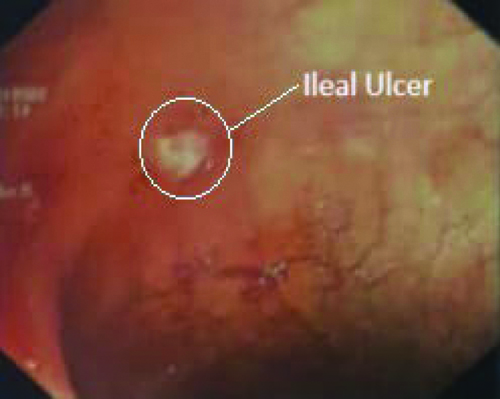
On sputum examination, again it was found to be negative for AFB in Ziel Neelsen (ZN) stain and GeneXpert. Viral serology for HIV, hepatitis B and C were repeated and again found to be non reactive. Owing to the history of occupation of sanitary work and possible contact with animal caraccas, brucella was excluded by negative results for anti-brucella IgG and IgM antibodies. Pyrexia of unknown origin was evaluated for enteric fever, malaria, and dengue, all were found to be negative. IGRA was found to be positive indicative of latent tubercular infection but active TB infection can’t be proven due to the absence of any infective foci which can be tested for AFB (ZN stain or GeneXpart) or histopathologicalor cytopathological examination [Table/Fig-2]. Radiological investigation including initial Chest-X ray [Table/Fig-3] and Ultrasonography (USG) of the whole abdomen along further High-resolution Computed Tomography (HRCT) thorax and CECT whole abdomen revealed no significant findings. A provisional diagnosis of anaemia of chronic disease with Palindromic Rheumatism was made and upper GI endoscopy and colonoscopy was done. Upper GI endoscopy was normal except for healed duodenal ulcers and fundal erosions but colonoscopy showed multiple terminal ileal ulcers [Table/Fig-4]. Histopathological examinations {Haematoxylin and Eosin (H&E)} of the tissue sample from the ulcer showed non specific ileitis with infiltration of lymphocytes and histiocytes. He was again put on symptomatic management with oral hematinic i.e., iron-folic acid combination twice daily and immunomodulators i.e., hydroxy-chloroquine 200 mg once daily and the symptoms resolved mid-year. On the follow-up visit after one year there was no recurrence of symptoms and haemoglobin level was increased up to 11.5 gm% but CRP remained constantly raised at 54.99 mg/L.
Currently, he presented in the Emergency Department with a severe and recurrent history of pain abdomen along with recurrence of similar constitutional symptoms of evening rise of temperature and body aches along with significant weight loss (10% of body weight) General examination revealed painless cervical lymphadenopathy and blood examination showed normal blood count except raised ESR and CRP levels. Blood and urine culture shows no growth. Serum Angiotensinogen Converting Enzyme (SACE) was within normal limits excluding sarcoidosis [1]. Vitamin D levels were found to be very low (18.9 ng/mL) along with low calcium levels (7.78 mg/dL). Upper GI endoscopy showed a fundal ulcer [Table/Fig-5] which was positive for the rapid urease test but colonoscopy showed no significant findings. The Mantoux test was found to be negative. Magnetic Resonance Imaging (MRI) enterographyand stool calprotectin level estimation was done to rule out Inflammatory Bowel Disease (IBD) i.e., Chron’s disease which revealed no abnormalities [2,3]. CECT abdomen showed conglomerated upper abdominal lymphadenopathy and further PET-CT scan of the whole body shows metabolically active lymph nodes in the neck (bilateral level i.v. lymph nodes along with left supraclavicular lymph node), mediastinum (para-tracheal and para-aortic), and abdomen (peri-gastric, gastro-hepatic, peri-portal, and mesenteric) [Table/Fig-6].
Microbiological parameters of the patient.
| Microbiological parameters | Results/Values | Reference range |
|---|
| HIV- I and II | Non reactive | - |
| Hepatitis B surface antigen | Non reactive | - |
| Anti-HCV antibody | Non reactive | - |
| Enteric fever, IgM and IgG antibody | Non reactive | - |
| Malaria parasite dual anitgen | Non reactive | - |
| Dengue NS1 ELISA (Abs) | 2.86 | Less than 9 |
| Brucella IgG antibody (U/mL) | 0.81 | Less than 9 |
| Brucella IgM antibody (U/mL) | 0.51 | Less than 9 |
| Manutox test (at 72 hours) | 4 mm induration, Negative | More than 4 mm |
| TB- IGRA quantiferon | Positive | - |
| Sputum for AFB (ZN stain) | Negative | - |
| Sputum for GeneXpart | Negative for Mtb | - |
| Tissue for AFB (ZN stain) | Negative | - |
| Tissue for GeneXpart | Negative for Mtb | - |
| Tissue for Mtb culture (BACTEC) | No growth after 8, 18, 28, 43 days | - |
| Blood and urine culture | No growth | - |
NS1 ELISA: Non structural protein 1 enzyme-linked immunosorbent assay, TB-IGRA: Tuberculosis-interferon gamma release assay; Mtb: Mycobacterium tuberculosis; HCV: Hepatitis C virus
Chest radiograph of the patient.
Ileal ulcer seen in colonoscopy.
Gastric ulcer seen in upper GI endoscopy.

PET-CT showing metabolically active lymph nodes in the body.
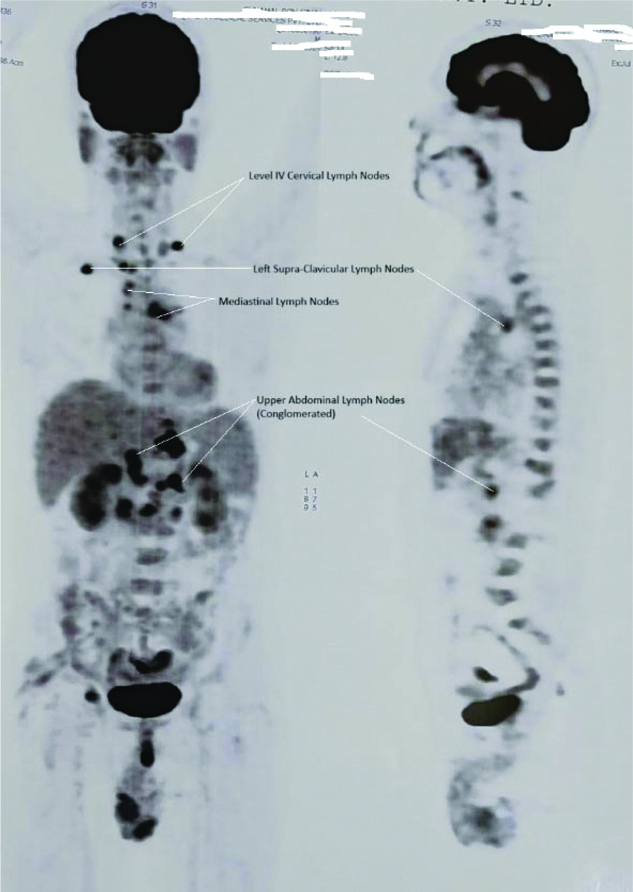
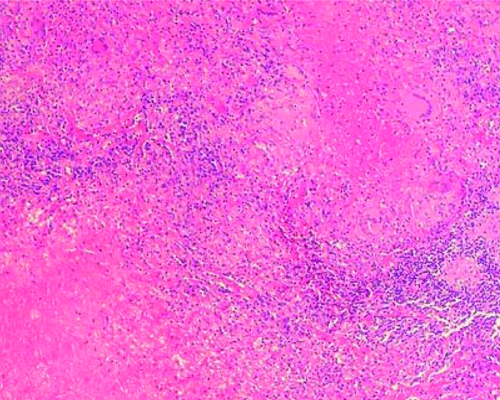
An excision biopsy was taken from the left supraclavicular lymph node under general anaesthesia and on histopathological examinations with haematoxylin and eosin [Table/Fig-7], it showed areas of caseous necrosis with epithelioid cell granuloma containing Langhan giant cells compatible with mycobacterial infection [4]. However, it was negative for AFB smear, GeneXpart, and culture. Finally, a diagnosis of disseminated TB lymphadenitis was confirmed due to the involvement of three non contagious sites i.e., abdomen, mediastinum, and neck along with peptic ulcer disease [5].
Caseous necrosis and giant cells in histopathological examination of left supraclavicular lymph node (H&E, 10x magnification).
The patient was put on first-line anti-tubercular therapy for six months (two months intensive phase i.e., Isoniazid, rifampicin, pyrazinamide, ethambutoland four months continuation phase i.e., Isoniazid, rifampicin, ethambutol) along with daily Vitamin B6 supplementation. Complete Blood Count (CBC), Liver Function Test (LFT) and uric acid levels were monitored during the treatment period. An eye examination was carried out before starting the Anti-tubercular Drug (ATD) and repeated every two months to rule out any ATD-related adverse effects. Adjacent to that triple regimen (Clarithromycin, Lansoprazole, Amoxicillin) was given for Helicobacter Pylori for 14 days. Vitamin D and calcium supplementation were also given.
On the follow-up visit, the patient showed significant clinical improvement with an increase in body weight i.e., 55 kg, and good appetite. There were no ATD-related side effects except asymptomatic hyperuricaemia (uric acid levels were 25 mg/dL), most probably due to pyrazinamide, for which the patient was given febuxostat 40 mg once daily at bedtime. On his last visit, uric acid levels were within normal limits i.e., 6.4 mg/dL.
Discussion
The TB is a chronic granulomatous infectious disease and it remains a significant public health challenge in India, the largest contributor (27%) to the global burden of TB. Though Pulmonary Tuberculosis (PTB) is the most common, 16% of all TB cases globally were EPTB [6]. Among these EPTB cases, tubercular lymphadenitis is the most common, accounting for 35% of all EPTB cases [7]. Scrofula or cervical lymph nodes were the most common lymph nodes involved in TB lymphadenitis [8].
The EPTB is relatively challenging to diagnose as conventional microbiological tests like ZN stain for AFB and GeneXpart often show negative results due to the pauci-bacillary nature of the infection. Other than that, EPTB can affect almost any body system and presents with diverse, often non-specific symptoms that mimic other diseases [9]. Thus, to identify the infective foci and its sampling, we have to rely on various non-invasive and invasive radiological imaging and sometimes surgical procedures, respectively. On the other hand, in the absence of any direct microbiological evidence, histopathological evidence of tubercular infection like granuloma, and caseating necrosis was a useful way to confirm the diagnosis of TB.
The above-mentioned patient was a unique case of disseminated TB lymphadenitis in an adult HIV-negative, immunocompetent individual, which is extremely rare but there were previous precedents though general constitutional symptoms like the mild rise of temperature in the evening, night sweats, body aches, cachexia, and anorexia were always there to raise suspicion of TB, a microbiologically negative sputum sample and normal chest X-ray ruled out pulmonary TB at first hand [7,8,10]. Anaemia of chronic disease and constantly raised inflammatory markers i.e., CRP throughout the period over four to five years suggested the presence of an underlying chronic inflammatory condition but the absence of any infective foci like lymphadenopathy in initial radiological imaging made further EPTB-related work-up difficult which is further complicated by the periodic nature of the constitutional symptoms mimicking relapse and remission in Chron’s disease.
This periodicity in the general constitutional symptoms may be explained by the waxing-waning phenomenon. After primary infection with TB bacilli was established, it leads to an unstable disease control state where precipitating factors like vitamin D deficiency, malnutrition, viral infection, etc., cause reactivation of latent TB infection and again followed by the control phase. [9] In present case, IGRA-proven latent TB infection periodically got reactivated and subsequent control may be responsible for this unique waxing-waning presentation.
The differential diagnosis in present case was considered as other chronic inflammatory conditions like Chron’s disease, sarcoidosis, HIV infections, and any slow-growing lymphoma.
This diagnosis of disseminated TB lymphadenitis in an adult, HIV-negative, immunocompetent individual was difficult due to the periodic relapse and negative initial diagnostic. Despite the absence of microbiological confirmation, the diagnosis was ultimately achieved through histopathological examination.
Future research should be focused on developing new diagnostic tools, sensitive and specific for diagnosing EPTB, and further investigating the underlying pathophysiology for this unique waxing-weaning course, which can be proven valuable for the management of future similar cases.
Conclusion(s)
Tubercular lymphadenitis with a waxing-waning pattern is a unique presentation. In the absence of traditional microbiological evidence like GeneXpart, the role of radiological imaging, and histopathological examination were pivotal for diagnosis and subsequent treatment.
RDW: Red cell distribution width; SGPT Serum glutamic-pyruvic transaminase; SGOT: Serum glutamic oxaloacetic acid transaminase; INR: International normalised ratio; LDH: Low-density lipid; RA: Rheumatoid arthritis; CA: Cancer antigen; FT4: Thyroxine free; Anti-CCP: Anti-cyclic citrullinated peptide
NS1 ELISA: Non structural protein 1 enzyme-linked immunosorbent assay, TB-IGRA: Tuberculosis-interferon gamma release assay; Mtb: Mycobacterium tuberculosis; HCV: Hepatitis C virus
[1]. Wessendorf TE, Bonella F, Costabel U, Diagnosis of sarcoidosisClin Rev Allergy Immunol 2015 49(1):54-62.10.1007/s12016-015-8475-x25779004 [Google Scholar] [CrossRef] [PubMed]
[2]. Sinha R, Murphy P, Sanders S, Ramachandran I, Hawker P, Rawat S, Diagnostic accuracy of high-resolution MR enterography in Crohn’s disease: Comparison with surgical and pathological specimenClin Radiol 2013 68(9):917-27.10.1016/j.crad.2013.02.01223622798 [Google Scholar] [CrossRef] [PubMed]
[3]. Kopylov U, Yung DE, Engel T, Avni T, Battat R, Ben-Horin S, Fecalcalprotectin for the prediction of small-bowel Crohn’s disease by capsule endoscopy: A systematic review and meta-analysisEur J Gastroenterol Hepatol 2016 28(10):1137-44.10.1097/MEG.000000000000069227415156 [Google Scholar] [CrossRef] [PubMed]
[4]. Ahmed HG, Nassar AS, Ginawi I, Screening for tuberculosis and its histological pattern in patients with enlarged lymph nodePatholog Res Int 2011 2011:41763510.4061/2011/41763521660265PMC3108380 [Google Scholar] [CrossRef] [PubMed]
[5]. Ayaslioglu E, Basar H, Duruyurek N, Kalpaklioglu F, Gocmen S, Erturk A, Disseminated tuberculosis with lymphatic, splenic and scrotal abscesses: A case reportCases J 2009 2:699510.4076/1757-1626-2-699519918502PMC2769332 [Google Scholar] [CrossRef] [PubMed]
[6]. World Health OrganizationGlobal tuberculosis report 2023 2023 GenevaWorld Health Organization[cited 2024 Dec 5]. Available from: https://www.who.int/teams/global-tuberculosis-programme/tb-reports [Google Scholar]
[7]. Sharma SK, Mohan A, Extrapulmonary tuberculosisIndian J Med Res 2004 120(4):316-53.15520485 [Google Scholar] [PubMed]
[8]. Singh SK, Tiwari KK, Tuberculous lymphadenopathy: Experience from the referral center of Northern IndiaNiger Med J 2016 57(2):134-38.10.4103/0300-1652.18207727226690PMC4872492 [Google Scholar] [CrossRef] [PubMed]
[9]. Esmail H, Barry CE, Young DB, Wilkinson RJ, The ongoing challenge of latent tuberculosisPhilos Trans R SocLond B Biol Sci 2014 369(1645):2013043710.1098/rstb.2013.043724821923PMC4024230 [Google Scholar] [CrossRef] [PubMed]
[10]. Gerogianni I, Papala M, Kostikas K, Ioannou M, Karadonta AV, Gourgoulianis K, Tuberculous disseminated lymphadenopathy in an immunocompetent non-HIV patient: A case reportJ Med Case Rep 2009 3:931610.1186/1752-1947-3-931620062745PMC2803839 [Google Scholar] [CrossRef] [PubMed]