Splenic Artery Pseudoaneurysm (SAP) is an uncommon false aneurysm that essentially develops due to the weakening of the vessel wall as a result of various local pathologies. Hereby, the authors present a case report, of a 32-year-old male with Human Immunodeficiency Virus (HIV) and Mycobacterium Tuberculosis (TB) co-infection presented with generalised weakness, vomiting, and a history of fever and cough. After admission, he developed massive haematemesis followed by hypotension; this led to an inconclusive upper gastrointestinal endoscopy. This prompted the authors to perform a contrast-enhanced Computed Tomography (CT) scan with angiography of the abdomen, which revealed an SAP, likely due to tubercular vasculitis. Embolisation of the pseudoaneurysm was performed using coils and N-Butyl Cyanoacrylate (NBCA) glue to stop the life-threatening haematemesis. The present case highlights the importance of considering SAP as a differential diagnosis in cases of unexplained haematemesis and emphasises the necessity of early embolisation as a life-saving measure due to its high fatality rate.
Angiography, Embolisation, Haemorrhage, Human immunodeficiency virus-tuberculosis, Tuberculoma, Vasculitis
Case Report
A 32-year-old male presented to the hospital with a seven-day history of generalised weakness and vomiting, along with a two-month history of fever and cough with whitish expectoration. He had been diagnosed with HIV infection and disseminated tuberculosis of the abdomen and thorax two months ago and had been on Antiretroviral Therapy (ART) (Tenofovir, Lamivudine, Dolutegravir) and Antitubercular Therapy (ATT) (Isoniazid, Rifampicin, Pyrazinamide, Ethambutol) since the diagnosis.
On examination, his blood pressure was 100/70 mmHg, pulse was 110/min, and oxygen saturation was 98% on room air. His temperature was 100 degrees Fahrenheit. General examination revealed the presence of icterus along with cervical lymphadenopathy. On systemic examination, he exhibited bronchospasm in both lungs and diffuse tenderness all over the abdomen. Routine laboratory investigations were performed [Table/Fig-1].
All routine investigations done on day 1.
| Investigations (day 1) | Value | Reference range |
|---|
| Haemoglobin | 10.4 g/dL | 13-16 g/dL |
| Total leukocyte count | 13410/microL | 4000-10000/microL |
| Platelets | 350000/microL | 150000-410000/microL |
| Urea | 18 mg/dL | 17-49 mg/dL |
| Creatinine | 0.8 mg/dL | 0.6-1.35 mg/dL |
| Total bilirubin | 2.26 mg/dL | 0.22-1.20 mg/dL |
| Conjugated bilirubin | 2.02 mg/dL | upto 0.5 mg/dL |
| Unconjugated bilirubin | 0.24 mg/dL | 0.1-1 mg/dL |
| SGOT | 208 IU/L | 8-48 IU/L |
| SGPT | 56 IU/L | 7-55 IU/L |
| ALP | 228 IU/L | 55-150 IU/L |
| Total protein | 6.8 g/dL | 6.4-8.3 g/dL |
| Albumin | 3.5 g/dL | 3.5-5.2 g/dL |
| PT-INR | 11.63 secs | 1.13 secs |
| Serum amylase | 40 IU/L | 30-110 IU/L |
| Serum lipase | 65 IU/L | 0-160 IU/L |
SGOT: Serum glutamic-oxaloacetic transaminase; SGPT: Serum glutamic pyruvic transaminase; ALP: Alkaline phophatase; PT-INR: Prothrombin-international normalised ratio
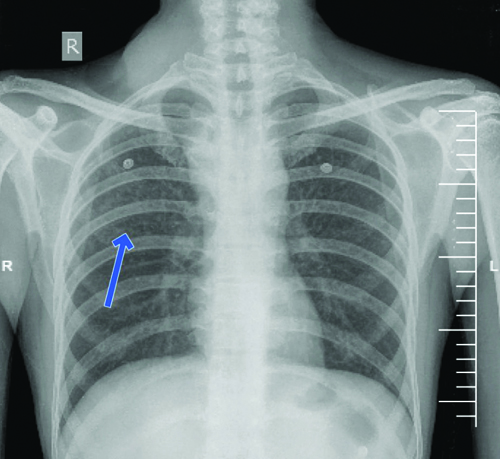
The routine laboratory investigations suggested drug-induced liver injury, most probably caused by the ATT, along with mild leukocytosis. A chest X-ray was done, which suggested scattered small nodular lesions indicative of Koch’s [Table/Fig-2].
The chest X-ray of the patient, performed on day 1, revealed the presence of multiple small nodular opacities scattered throughout the lung fields (marked by blue arrow). These opacities are characteristic of miliary or disseminated tuberculosis, indicating widespread haematogenous spread of Mycobacterium tuberculosis.
Routine ultrasonography of the abdomen revealed multiple small hypoechoic lesions in the spleen, suggestive of splenic abscesses, and multiple necrotic mesenteric lymph nodes. He was started on Injection Cefepime-Tazobactam 1.125 g intravenously three times daily, along with Tablet Cotrimoxazole 160 mg/800 mg twice daily. Nebulisation with salbutamol was initiated three times daily. The ongoing ATT regimen was stopped in view of drug-induced liver injury, and the patient was switched to an alternative ATT regimen consisting of Injection Streptomycin 750 mg once daily, Tablet Levofloxacin 750 mg once daily, and Tablet Ethambutol 60 mg once daily. ART was continued, and the patient was advised adequate oral hydration.
On the third day of admission, the patient experienced two episodes of haematemesis, each approximately 200 mL, consisting of altered blood. After the haematemesis episodes, the patient developed hypotension and was shifted to the Intensive Care Unit (ICU) for further management. He was started on a single inotrope, Injection Noradrenaline 8 mg in 50 mL normal saline, and the dose was titrated according to blood pressure. He received one packed cell volume transfusion, a Ryles tube was inserted, cold saline lavage was administered, and the patient was kept Nil by mouth.
On the fourth day of admission, an upper gastrointestinal tract endoscopy was performed by the medical gastroenterology team, which was inconclusive as nothing could be visualised due to the presence of blood in the stomach. This led to proceed with contrast-enhanced CT of the thorax and abdomen, along with angiography for further investigation. Laboratory investigations were repeated on the fourth day of admission, and the results were as follows [Table/Fig-3].
Laboratory investigations done on day 4.
| Investigations (day 4) | Value | Reference range |
|---|
| Haemoglobin | 8.4 g/dL | 13-16 g/dL |
| Total leucocyte count | 12000/microL | 4000-10000/microL |
| Platelet counts | 489000/microL | 150000-410000/microL |
| D-dimer | 1842 ng/mL | 0-500 ng/mL |
| PT-INR | 12.7 secs/1.24 | 10.35-12.90 secs |
| aPTT (patient value) | 32.33 secs | 28.05-36 secs |
| Serum fibrinogen | 225 mg/dL | 238-498 mg/dL |
aPTT: Activated partial thromboplastin time
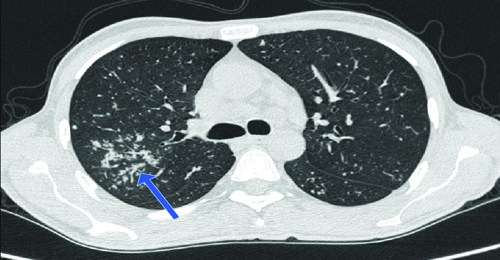
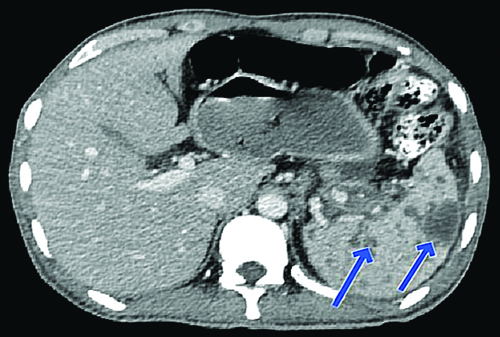
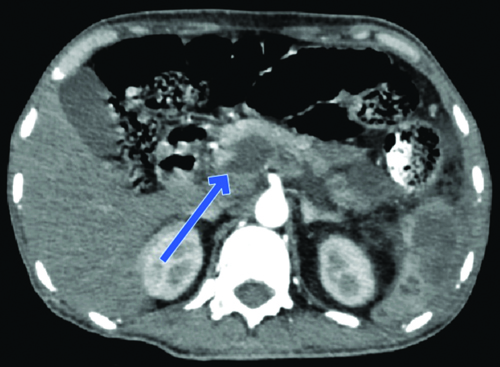
The International Society of Thrombosis and Haemostasis (ISTH) criteria for the diagnosis of Disseminated Intravascular Coagulation (DIC) were applied, resulting in a score of three points, which was not indicative of overt DIC. He received one packed cell volume transfusion, and his requirement for Noradrenaline continued to decrease on the fourth day, eventually leading to its cessation on the same day. Multiple centrilobular nodules with a tree-in-bud appearance were observed in the right upper lobe of the lung [Table/Fig-4]. Additionally, multiple hypodense lesions scattered throughout the spleen, likely granulomas or tubercular abscesses, were seen [Table/Fig-5]. The Computed Tomography (CT) reports revealed a well-defined, homogeneously enhancing lesion in the distal body and tail of the pancreas, suggestive of a pseudoaneurysm originating from a pancreatic branch of the splenic artery, likely secondary to tubercular vasculitis [Table/Fig-6,7].
Contrast-enhanced Computed Tomography (CT) of thorax showing multiple centrilobular nodules with tree in bud appearance in right upper lobe of lung as marked by blue arrow, suggestive of pulmonary tuberculosis as the primary source of dissemination of tuberculosis.
The contrast-enhanced Computed Tomography (CT) of the abdomen reveals multiple splenic abscesses, as indicated by the blue arrows. These abscesses appear as ill-defined, hypodense lesions scattered throughout the spleen, which are suggestive of infectious or granulomatous involvement secondary to disseminated tuberculosis.
Contrast-enhanced Computed Tomography (CT) with angiography of abdomen showing a well-defined homogeneously enhancing lesion in dorsal portion of distal body and tail of pancreas in arterial phase suggestive of pseudoaneurysm arising from pancreatic branch of splenic artery as marked by blue arrow.
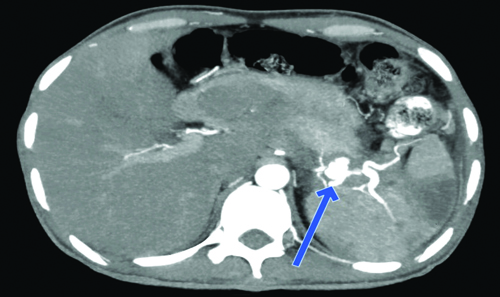
Contrast-enhanced Computed Tomography (CT) of abdomen showing ill-defined hypodense lesion in body and tail of pancreas suggestive of pancreatic tuberculosis as marked by blue arrow. This explains the involvement of pancreatic branch of splenic artery and development of pseudoaneurysm.
Given these findings, an interventional radiology consultation was sought, and the patient was scheduled for splenic artery pseudoaneurysm embolisation to prevent further life-threatening bleeding.
On the fifth day of admission, the patient underwent selective embolisation of the pseudoaneurysm via right femoral arterial access. The procedure involved deploying multiple pushable coils and 33% NBCA glue mixed with lipiodol to achieve haemostasis.
The patient was observed for two days and was subsequently discharged when he was asymptomatic. He was instructed to Follow-up in the Outpatient Department (OPD)) after four days for reintroduction of the HRZE (Isoniazid, Rifampicin, Pyrazinamide, Ethambutol) regimen of ATT.
The patient followed-up four days later, and the reintroduction of the HRZE regimen was initiated in a phased manner. However, the patient was lost to follow-up two weeks after the reintroduction of the previous ATT regimen of HRZE, and his long-term response could not be properly monitored.
Discussion
The most common causes of upper gastrointestinal bleeding are non variceal, with peptic ulcers and mucosal erosive diseases being far more prevalent in that order of incidence [1]. However, Splenic Artery Pseudoaneurysm (SAP) is an uncommon cause of haematemesis, often linked to vasculitis or direct vascular erosion by tuberculous abscesses [2]. Aneurysms associated with tuberculosis are pseudoaneurysms in 87% of cases rather than true aneurysms [3]. SAP ruptures and leaks into the pancreatic duct, leading to haematemesis and melena [4]. This phenomenon of bleeding into the pancreatic duct is also known as haemosuccus pancreaticus [4]. Contrast-enhanced CT of the abdomen, along with angiography, is the preferred investigation for early diagnosis, as abdominal ultrasound can sometimes miss findings in cases of small aneurysms [4].
In the case of mycotic aneurysms related to tuberculosis, large arteries are more prone to involvement, but small to mid-sized arteries are at greater risk of rupture, leading to increased mortality in these cases [2]. Tuberculous affection of the pancreas has been implicated in causing pseudoaneurysms of the splenic artery, and almost 50% of these cases have been found to have co-infection with HIV [5], with the most commonly involved portion of the pancreas being its body [5]. The risk of rupture of SAP is not dependent on its size, and post-rupture mortality remains as high as 90% if not treated promptly [6]. The use of NBCA glue has proven to be as effective as surgical intervention [7]. The mortality rate after surgical resection of SAP can be as high as 10% [7]. The last resort after the failure of embolisation of the pseudoaneurysm is surgical intervention, which may consist of arterial ligation, splenectomy, or resection with bypass [8].
Both minimally invasive embolisation and surgical intervention have similar efficacy when compared, whereas surgical intervention carries a morbidity rate of around 9% [6]. Given the high mortality associated with delayed intervention, clinicians should maintain a high index of suspicion for vascular complications in immunocompromised patients with unexplained gastrointestinal bleeding. Minimally invasive procedures should be prioritised to improve outcomes. Further research with a large sample size is required to study the long-term outcomes and associated complications of minimally invasive endovascular embolisation procedures for SAP.
Conclusion(s)
The present case report highlights SAP as a rare but life-threatening cause of haematemesis in a patient with HIV and tuberculosis co-infection. Early diagnosis using CT with angiography of the abdomen is crucial, as upper gastrointestinal endoscopy is sometimes inconclusive. Ultrasonography of the abdomen is less sensitive compared to CT with angiography, and the latter should be performed without delay in such patients for accurate diagnosis and prompt initiation of treatment. Successful embolisation with coils and NBCA glue prevented further haemorrhage and eliminated the need for high-risk surgery.
SGOT: Serum glutamic-oxaloacetic transaminase; SGPT: Serum glutamic pyruvic transaminase; ALP: Alkaline phophatase; PT-INR: Prothrombin-international normalised ratio
aPTT: Activated partial thromboplastin time
[1]. Gralnek IM, Dumonceau JM, Kuipers EJ, Lanas A, Sanders DS, Kurien M, Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) guidelineEndoscopy 2015 47:a1-46.10.1055/s-0034-139317226417980 [Google Scholar] [CrossRef] [PubMed]
[2]. Yi S, Wang L, Clinical features of tuberculous pseudoaneurysm and risk factors for mortalityJ Vasc Surg 2022 75(5):1729-38.e2.10.1016/j.jvs.2021.10.04834788648 [Google Scholar] [CrossRef] [PubMed]
[3]. Irfan M, Thiavalappil F, Nagaraj J, Brown TH, Roberts D, McKnight L, Tuberculous pancreatitis complicated by ruptured splenic artery pseudoaneurysmMonaldi Arch Chest Dis 2013 79(3-4):134-35.10.4081/monaldi.2013.521224761532 [Google Scholar] [CrossRef] [PubMed]
[4]. Tessier DJ, Stone WM, Fowl RJ, Abbas MA, Andrews JC, Bower TC, Clinical features and management of splenic artery pseudoaneurysm: Case series and cumulative review of literatureJ Vasc Surg 2003 38(5):969-74.10.1016/S0741-5214(03)00710-914603202 [Google Scholar] [CrossRef] [PubMed]
[5]. Sharma V, Rana SS, Kumar A, Bhasin DK, Pancreatic tuberculosisJ Gastroenterol Hepatol 2016 31(2):310-18.10.1111/jgh.1317426414325 [Google Scholar] [CrossRef] [PubMed]
[6]. Varshney P, Songra B, Mathur S, Gothwal S, Malik P, Rathi M, Splenic artery pseudoaneurysm presenting as massive haematemesis: A diagnostic dilemmaCase Rep Surg 2014 2014:50193710.1155/2014/50193724716077PMC3971889 [Google Scholar] [CrossRef] [PubMed]
[7]. Tonpe S, Warbhe H, Banode P, Waghulkar S, Dugad S, Suryadevara M, Splenic artery pseudoaneurysm management with cyanoacrylate glue: A case reportCureus 2024 16(8):e6592610.7759/cureus.65926 [Google Scholar] [CrossRef]
[8]. Corvino F, Giurazza F, Ierardi AM, Lucatelli P, Basile A, Corvino A, Splenic artery pseudoaneurysms: The role of CE-CT for diagnosis and treatment planningDiagnostics (Basel) 2022 12(4):101210.3390/diagnostics1204101235454060PMC9024490 [Google Scholar] [CrossRef] [PubMed]