An Atypical Case of Primary Angiitis of Central Nervous System Featuring Normal Cerebrospinal Fluid Analysis and Multiple Cavernomas
Salil Gundewar1, Pravin Naphade2, Satish Nirhale3, Prajwal Rao4, Pranit Khandait5
1 Senior Resident, Department of Neurology, Dr. D. Y. Patil Medical College and Research Centre (DPU), Pune, Maharashtra, India.
2 Associate Professor, Department of Neurology, Dr. D. Y. Patil Medical College and Research Centre (DPU), Pune, Maharashtra, India.
3 Professor, Department of Neurology, Dr. D. Y. Patil Medical College and Research Centre (DPU), Pandharpur, Maharashtra, India.
4 Professor, Department of Neurology, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Dr. D. Y. Patil Vidyapeeth, (Deemed to be University), Pimpri, Pune, Maharashtra, India.
5 Senior Resident, Department of Neurology, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Dr. D. Y. Patil Vidyapeeth, (Deemed to be University), Pimpri, Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Salil Gundewar, Gangaskies Apartment, Pimpri, Pune, Maharashtra, India.
E-mail: salil.gundewar386@gmail.com
Primary Angiitis of Central Nervous System (PACNS) is a rare disease with an incidence of 2.4 cases per 10000 persons per year. Diagnosis of the condition is challenging due to its variable presentation. Delay in treatment may cause irreversible neurological consequences. Evaluation includes laboratory tests such as complete blood count, renal function tests, urine routine microscopy, Erythrocyte Sedimentation Rate (ESR), Anti-Nuclear Antibodies (ANA) by Immunofluorescence Assay (IFA) and blot method, complement (C3 and C4) levels, Cerebrospinal Fluid (CSF) evaluation and neuroimaging, including Magnetic Resonance Imaging (MRI) of the brain. Digital Subtraction Angiography (DSA) and High-Resolution Vessel Wall Imaging (HRVWI) may help establish the diagnosis. The Gold standard investigation for diagnosis of PANCS is histopathology of brain biopsy tissue. Here, a case of a 40-year-old male with acute and chronic infarcts in multiple territories with no prior co-morbid conditions is presented. CSF study was within normal limits. Although, DSA and HRVWI showed inflammation in the walls of the left Middle Cerebral Artery (MCA) (M2, M3 segment) and bilateral Anterior Cerebral Arteries (ACAs). This highlights the extremely rare association of PACNS with normal CSF analysis. Diagnosing PACNS is challenging due to its variable presentation, and CSF analysis is typically abnormal in 80-90% of cases. However, the CSF analysis was normal in this case, underscoring the importance of further evaluation in cases with a high suspicion of PACNS.
Digital subtraction angiography, High-resolution contrast-enhanced vessel wall imaging, Systemic vasculitis
Case Report
A 40-year-old male, a shopkeeper by occupation, presented with complaints of acute onset confusion with instances of getting lost in the surroundings and inability to perform monetary transactions at his shop for one week. He had a history of acute onset weakness in the right upper limb and lower limb one month back which improved partially over a period of one week. There were no other comorbidities with no significant family history. Higher mental examination showed a forward digit span of six, a backward digit span of four and right parietal lobe dysfunction in the form of constructional apraxia and topographical disorientation. Mini Mental Scale Examination (MMSE) showed a score of 24/30 with loss of points in calculation and orientation [1]. Frontal Assessment Battery (FAB) score was 12/18 [2]. Motor examination showed power of grade 4+/5 in the right upper and lower limbs. On the basis of history and examination, recurrent stroke involving different territories was the likely provisional diagnosis. Differential diagnosis included PACNS, and Reversible Cerebral Vasoconstriction Syndrome (RCVS).
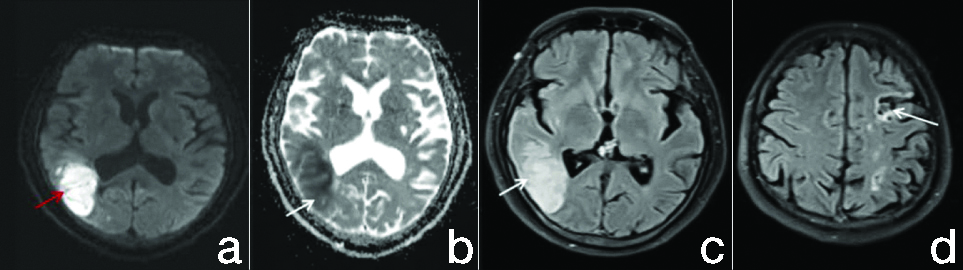
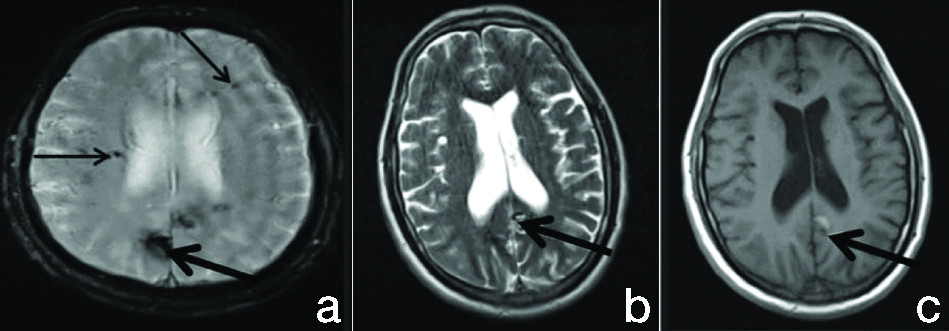
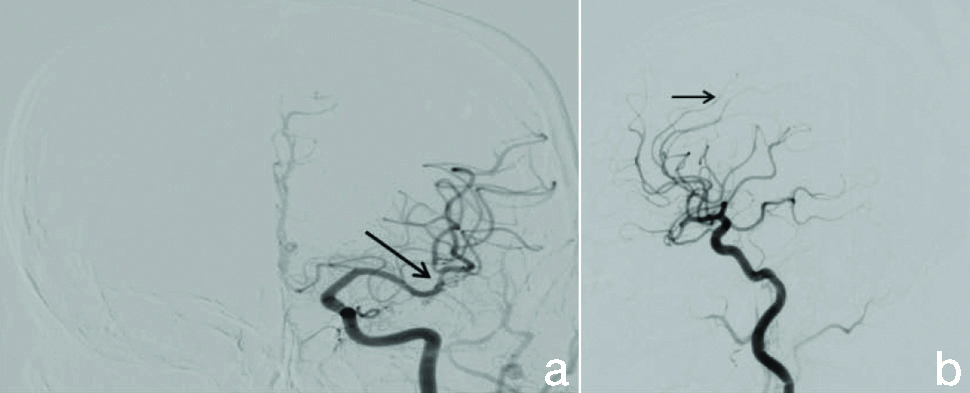
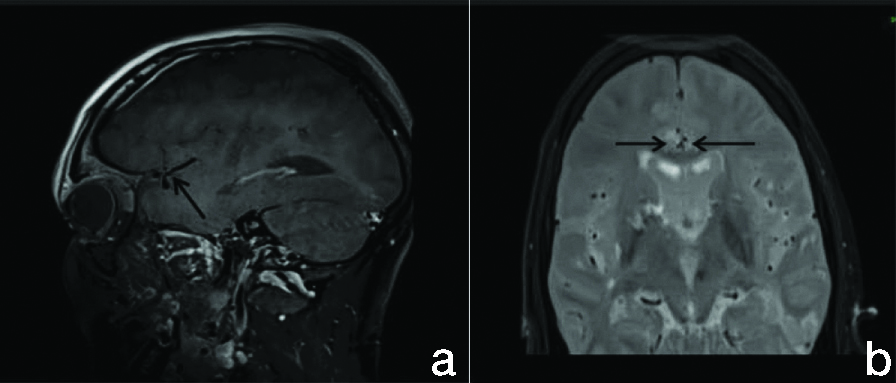
All routine investigations were normal. MRI brain showed acute ischaemic stroke in right parietal lobe and gliosis in left internal capsule suggestive of chronic infarct [Table/Fig-1]. Susceptibility Weighted Imaging (SWI) showed large areas of blooming with popcorn appearance on T1 and T2 weighted imaging. Additional microbleeds were seen on SWI [Table/Fig-2]. All these findings were reported as multiple cavernomas. D-dimer levels were 1642 ng/mL. Cardiac work up including two-dimensional Echocardiography (2D ECHO) and 48 hours Holter monitoring were normal. Suspecting malignancy, whole body Positron Emission Tomography (PET) scan was done which did not show any metabolically active lesions in the body. CSF examination was within normal limits. ANA by IFA was weakly positive (+1). ANA blot was negative. Computed Tomography Angiography (CTA) head and neck vessels was normal. Due to high suspicion of PACNS, DSA was done which showed a beading appearance in the left MCA M2 segment, bilateral ACAS [Table/Fig-3]. HRVWI showed inflammation in the walls of left MCA (M2, M3 segment) and bilateral ACAs [Table/Fig-4]. Thus, PACNS vasculitis was strongly suspected considering clinical presentation and investigations.
(a) Diffusion restriction in the right parietal lobe on Diffusion-Weighted Imaging (DWI) sequence; (b) low Apparent Diffusion Coefficient (ADC) values on ADC sequence; (c) hyperintensity on Fluid Attenuated Inversion Recovery (FLAIR) sequence; and (d) hypointensity in the left high frontal region on T1 sequence.
(a) Multiple large and small bloomings on the Susceptibility Weighted Imaging (SWI) sequence; (b) popcorn appearance with mixed hyper and hypointensities on T2 sequence; and (c) popcorn appearance with mixed hyper and hypointensities on T1 sequence.
a) Beading appearance (arrow) in bilateral Anterior Cerebral Artery (ACA) terminal branches; and (b) Beading appearance (arrow) in the left Middle Cerebral Artery (MCA) M2, M3 segment.
(a) Left MCA M2 segment wall contrast uptake (arrow) in T1 black blood sequence; and (b) bilateral ACA wall contrast uptake (arrow) in T1 black blood sequence.
Patient was advised brain biopsy but he did not give consent for the same. Hence patient was given methylprednisolone pulse dose therapy of 30 mg/kg for five days followed by cyclophosphamide 750 mg as per body surface area as induction phase. This was followed by monthly maintenance dosages of cyclophosphamide 750 mg per body surface area. Repeat DSA done at eight weeks has revealed no changes as compared to the previous study. The patient has demonstrated gradual improvement in his symptoms with no new signs of stroke on follow-up.
Discussion
PACNS is a rare disease with an incidence of 2.4 cases per 10000 persons per year [3]. PACNS has a highly variable presentation. PACNS is a diagnosis of exclusion. Patients with suspicion for PACNS should undergo CSF routine microscopy examination, and radiological investigations including MRI brain, HRVWI, DSA and brain biopsy [4]. PACNS’s incidence is 2.4 cases per 1,000,000 persons/year with a male-to-female ratio of 1:1. It involves inflammation of blood vessels in the central nervous system due to activation of T cells specifically CD45R0+ T cells. It leads to three types of vasculitic patterns. These include the granulomatous, necrotising, and lymphocytic type. It usually presents with an insidious onset headache along with cognitive impairment. Strokes tend to involve multiple territories. Other rare clinical manifestations include convulsions and states of altered sensorium, ataxia and cranial neuropathies. A high index of suspicion is required owing to its variable presentation [5]. Differential diagnoses include infections like syphilis, herpes simplex infection, systemic vasculitis including systemic lupus erythematosus, Sjogren’s syndrome, autoimmune encephalitis and paraneoplastic causes. Extensive evaluation is required in suspected cases of PACNS to rule out other causes [6].
Evaluation includes laboratory tests such as complete blood count, renal function tests, urine routine microscopy, ESR, CRP, ANA by IFA and blot method, and complement (C3 and C4) levels. Patients also require CSF evaluation and neuroimaging, including Magnetic Resonance Imaging (MRI) of the brain. CSF analysis is abnormal in 80-90% of the cases with the presence of lymphocytic pleocytosis, elevated proteins, and normal glucose concentrations. This suggests that it can be normal in about 10% of the cases suggesting that normal CSF does not exclude the diagnosis [7]. Patients should undergo Magnetic Resonance Angiography (MRA) or CTA of head and neck vessels. If these tests are normal, DSA should be performed as it has higher sensitivity for detecting the involvement of medium and small-sized vessels compared to MRA and CTA [7]. In 2017, McVerry F et al., conducted a study on the published cases of PACNS. He found that 124 out of 484 patients had normal CSF findings [8]. While RCVS should be considered in patients with normal CSF findings, the current case did not have its hallmark feature of thunderclap headache. Additionally, persistence of findings on repeat DSA after 6-8 weeks strongly suggests PACNS rather than RCVS [9]. HRVWI is a non invasive investigation that aids in the diagnosis of PACNS. It includes black blood sequences which differentiate the vessel wall from its lumen. It provides complimentary evidence in the diagnosis of PACNS [10]. The gold standard for the diagnosis of PACNS is histopathology of brain biopsy tissue. It has a sensitivity of 75%, suggesting that 25% of the cases could still be missed out [11].
In biopsy-proven cases of PACNS, treatment modalities include glucocorticoids and cyclophosphamide. In patients who cannot tolerate cyclophosphamide, rituximab can be given. In possible cases of PACNS, initially, patients can be given pulse dose therapy of glucocorticoids followed by slow tapering. Cyclophosphamide can be added depending on the extent and severity of neurological deficits [12].
Conclusion(s)
Consideration of PACNS is essential in young males presenting with strokes in multiple vascular territories, chronic headaches, cognitive decline, and no known risk factors for stroke. A high index of suspicion is warranted due to its variable and often subtle presentation. Notably, routine CSF microscopy is abnormal in up to 90% of PACNS cases suggesting that it could be normal in approximately 10% of the cases. In such cases, a differential diagnosis of RCVS should be explored. However, patients with RCVS typically present with severe thunderclap headaches, in contrast to the mild and persistent headaches observed in the current case. Persistence of findings on repeat DSA after 6-8 weeks would strongly favour a diagnosis of PACNS vasculitis over RCVS. To date, very few cases of PACNS vasculitis with normal CSF have been documented, making this a truly unique and rare case.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 04, 2024
Manual Googling: Jan 10, 2025
iThenticate Software: Feb 22, 2025 (9%)
[1]. Su Y, Dong J, Sun J, Zhang Y, Ma S, Li M, Cognitive function assessed by Mini-mental state examination and risk of all-cause mortality: A community-based prospective cohort studyBMC Geriatr 2021 21(1):52410.1186/s12877-021-02471-934600472PMC8487495 [Google Scholar] [CrossRef] [PubMed]
[2]. Lima CF, Meireles LP, Fonseca R, Castro SL, Garrett C, The Frontal Assessment Battery (FAB) in Parkinson’s disease and correlations with formal measures of executive functioningJ Neurol 2008 255(11):1756-61.10.1007/s00415-008-0024-618821046 [Google Scholar] [CrossRef] [PubMed]
[3]. Agarwal A, Sharma J, Srivastava MVP, Sharma MC, Bhatia R, Dash D, Primary CNS vasculitis (PCNSV): A cohort studySci Rep 2022 12(1):1349410.1038/s41598-022-17869-735931755PMC9355950 [Google Scholar] [CrossRef] [PubMed]
[4]. Kraemer M, Berlit P, Primary central nervous system vasculitis – An update on diagnosis, differential diagnosis and treatmentJ Neurol Sci 2021 424:11742210.1016/j.jns.2021.11742233832773 [Google Scholar] [CrossRef] [PubMed]
[5]. Pascarella R, Antonenko K, Boulouis G, De Boysson H, Giannini C, Heldner MR, European Stroke Organisation (ESO) guidelines on Primary Angiitis of the Central Nervous System (PACNS)Eur Stroke J 2023 8(4):842-79.10.1177/2396987323119043137903069PMC10683718 [Google Scholar] [CrossRef] [PubMed]
[6]. Wilson MR, O’Donovan BD, Gelfand JM, Sample HA, Chow FC, Betjemann JP, Chronic meningitis investigated via metagenomic next-generation sequencingJAMA Neurol 2018 75(8):947-55.10.1001/jamaneurol.2018.046329710329PMC5933460 [Google Scholar] [CrossRef] [PubMed]
[7]. Deb-Chatterji M, Schuster S, Haeussler V, Gerloff C, Thomalla G, Magnus T, Primary angiitis of the central nervous system: New potential imaging techniques and biomarkers in blood and cerebrospinal fluidFront Neurol 2019 10:56810.3389/fneur.2019.0056831244749PMC6562270 [Google Scholar] [CrossRef] [PubMed]
[8]. McVerry F, McCluskey G, McCarron P, Muir KW, McCarron MO, Diagnostic test results in primary CNS vasculitisNeurol Clin Pract 2017 7(3):256-65.10.1212/CPJ.000000000000035930107009PMC6081966 [Google Scholar] [CrossRef] [PubMed]
[9]. Perillo T, Paolella C, Perrotta G, Serino A, Caranci F, Manto A, Reversible cerebral vasoconstriction syndrome: Review of neuroimaging findingsRadiol Med (Torino) 2022 127(9):981-90.10.1007/s11547-022-01532-235932443PMC9362037 [Google Scholar] [CrossRef] [PubMed]
[10]. Edjlali M, Qiao Y, Boulouis G, Menjot N, Saba L, Wasserman BA, Vessel wall MR imaging for the detection of intracranial inflammatory vasculopathiesCardiovasc Diagn Ther 2020 10(4):1108119-1119.10.21037/cdt-20-32432968663PMC7487407 [Google Scholar] [CrossRef] [PubMed]
[11]. Mitrović J, Golob M, Lazibat I, Primary angiitis of the central nervous system - a diagnostic challengeActa Clin Croat 2023 62(2):355-61.10.20471/acc.2023.62.02.1438549589PMC10969649 [Google Scholar] [CrossRef] [PubMed]
[12]. Salvarani C, Brown RD, Christianson TJH, Huston J, Giannini C, Miller DV, Adult primary central nervous system vasculitis treatment and course: Analysis of one hundred sixtythree patientsArthritis Rheumatol Hoboken NJ 2015 67(6):1637-45. [Google Scholar]