The elderly are defined as individuals aged 65 years and older, with the age group of 65 to 74 years classified as early elderly and those aged 75 and above categorised as late elderly [1-4]. Older individuals are more susceptible to various systemic problems, including neurological, musculoskeletal, gastrointestinal and cardiorespiratory issues. Falls and imbalances in the elderly represent significant multisystem functional impairments that can lead to severe depression and dependency [5-9]. The fear of falls due to loss of balance is a notable predictor of impairment in the elderly population. Motor skill performance declines as age increases [10-13]. The risk of falling or losing balance in older adults is typically related to a combination of factors, which include fall history, the use of assistive devices, multiple health conditions, muscle weakness, vertigo, hearing disorders, cognitive and sensory deficiencies, orthostatic hypertension, diabetes mellitus and osteoporosis [14-17].
Rhythmic Auditory Stimulation (RAS) enhances motor performance. Auditory stimulation, or auditory cueing, has been found to be more beneficial compared to visual or tactile cueing [8]. RAS directly influences the gait kinematics of individuals. The timing mechanism of RAS is effective in promoting the forecasting of motor judgement and gait regularity [9].
There are various modes of treatment available to manage patients at risk of falling. Some of these include the use of wobble boards, Swiss balls, exercises to improve proprioception and training strategies to maintain the center of gravity within the base of support. The combined effects of RAS and VF are recent techniques that have not been adequately explored. Available evidence suggests that RAS has a significant influence on improving functional performance in patients with Parkinson’s disease and hemiplegia [6]. On the other hand, VF has strong evidence supporting its usefulness in improving motor networks, simplifying movement re-education and enhancing cognitive perception required to assess depth [7].
The loss of balance or fear of falling accounts for moderate to severe activity limitations. Elderly individuals face a nine-fold greater risk of falling [1]. The risk of falling in older adults over the age of 65 is 33% over the course of one year [3]. Balance is one of the most important fundamental motor activities used by individuals in their daily lives. A study has shown that RAS has the potential to influence functional performance in patients with Parkinson’s disease and hemiplegia [9]. However, there is very little evidence regarding the combined effects of RAS and VF on balance and the prevention of falls in the elderly population [11]. Thus, this study aims to examine the effect of metronome-guided balance training on falls in the elderly using both RAS and VF.
Materials and Methods
The present randomised controlled trial was conducted at a tertiary care hospital, specifically in the Department of Physiotherapy, Dr. D. Y. Patil College of Physiotherapy, Pune, Maharashtra, India, from June 2023 to July 2024. The study was initiated after receiving approval from the Institutional Ethics Committee (IEC), DYPCPT/ISEC/70/20222. Written informed consent for voluntary participation was obtained from all participants. The assessor who evaluated the patients was blinded.
Inclusion criteria: The study involved elderly individuals diagnosed with a moderate risk of falls, indicated by a FES score of less than 24 [5]. This assessment was made by a physician from the Department of Geriatric Medicine. The participants included were aged 65 to 74 years, had little or no use of walking aids, were able to follow simple commands and could see the screen. Additionally, visually able patients, those without any hearing disorders and individuals capable of understanding and following commands were included in the study.
Exclusion criteria: Patients diagnosed with neurological conditions, musculoskeletal conditions, amputations and other neurodegenerative conditions were excluded from the study.
Sample size calculation: The sample size estimation was based on the effect size of a previously published study by Gonzalez-Hoelling S et al., [12]. The calculated sample size was 60, using WINPEPI software version 11.38. The final sample size obtained was 53 participants. Considering a 10% attrition rate of the study participants, the final total sample size was rounded off to 60.
Study Procedure
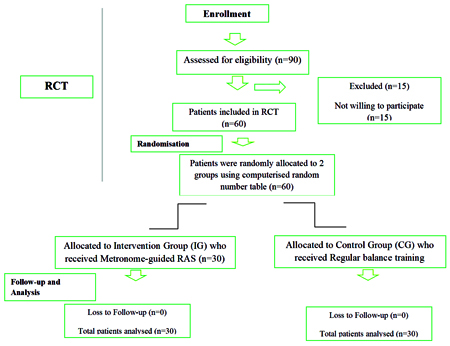
A total of 60 patients were divided into two groups through simple random sampling using a computer-generated sequence method. A total of 30 subjects were allocated to the IG [Table/Fig-1], who received balance training using a mirror. They were instructed to perform exercises while looking in the mirror and to execute the movements after listening to the metronome beat, with added RAS provided by metronome beats. The frequency of the metronome was set at four beats per minute [6]. The patients were instructed to perform exercises while listening to the metronome beats. The remaining 30 participants formed the CG. The CG received regular balance training, which included walking in parallel bars, changes in cadence and Frenkel’s exercises. The intervention was administered for four weeks, five days per week, with 30-minute sessions each day. After four weeks, the assessment was repeated using all three outcome measures [Table/Fig-1].
Consolidated Standards of Reporting Trials (CONSORT) flow diagram.
Intervention:
• Week I:
Standing with feet together, using the support of a chair, table, or wall.
Tandem stance with the support of a chair, table, or wall.
Standing on one leg with the support of a chair, table, or wall.
Functional reach in a semi-tandem position with the support of a chair, table, or wall.
Stepping up onto a higher surface with the support of a chair, table, or wall.
• Week II:
Standing with feet together and hands wide apart.
Progressing to a semi-tandem stance.
Standing on one leg with hands on the pelvis.
Functional reach test with feet together.
Stepping up onto a higher surface without support.
• Week III:
Standing with feet together and hands across the chest.
Tandem stance with arms across the chest.
Standing on one leg with hands across the chest.
• Week IV:
Ankle strategy on a wobble board.
Transferring body weight from one leg to another.
Tandem walking with hands raised to 90 degrees.
Outcome measures: A pre- and post-assessment was conducted during the first session and at the end of the fourth week. The assessment was divided into three domains: dynamic balance, static balance and fear of falling.
Dynamic balance was assessed using the Berg Balance Scale (BBS). The capacity (or inability) of a patient to safely balance during a series of specified tasks is objectively evaluated using the BBS. It takes about 20 minutes to complete and consists of 14 items, each of which uses a five-point ordinal scale from 0 to 4, where 0 represents the lowest level of function and 4 represents the highest. The scale does not evaluate gait [18].
Static balance was assessed using the Tinetti Performance-oriented Mobility Assessment (POMA) Scale. This scale evaluates a person’s fear of falling as well as their sense of stability and balance when performing daily tasks [1,2]. It is an excellent predictor of a person’s risk of falling.
The test consists of two brief sections: one assesses static balancing skills while standing and subsequently sitting, while the other evaluates gait. Compared to other tests, such as the Timed Up and Go (TUG) test, one-leg stand and functional reach tests, it has superior test-retest, discriminative and predictive validity regarding fall risk [3].
In the present study, the patient was instructed to get up and remain upright while seated in an armless chair. The patient was then instructed to sit back down after completing a full 360-degree spin [5]. This was done to assess the patient’s equilibrium. To evaluate this, the authors examined several important factors, such as the patient’s ability to get in and out of the chair, whether the patient remained upright when standing or sitting and what occurred when the patient’s eyes were closed or when the patient felt slight pressure on the sternum [1].
The Tinetti test includes a gait score and a balance score. It uses a 3-point ordinal scale of 0, 1 and 2. Gait is scored out of 12 and balance is scored out of 16, with a total possible score of 28 [5].
Fear of falling was examined using the Falls Efficacy Scale (FES). This scale measures fear of falling and concerns about falling and was developed as part of the Prevention of Falls Network Europe (ProFaNE) project from 2003 to 2006 by Todd et al., It is a 16-item questionnaire useful for researchers and clinicians interested in the fear of falling, with a score ranging from a minimum of 16 (no concern about falling) to a maximum of 64 (severe concern about falling) [18].
Statistical Analysis
Statistical analysis was performed using WINPEPI Software Version 11.38. The Confidence Interval was set at 95% (CI) and the level of significance was defined as p<0.05. A paired t-test was applied for intragroup analysis, while an unpaired t-test was used for intergroup analysis.
Results
The mean age of participants included in the study was 70.5±2.5 years. Out of 60 samples, 32 were males and 28 were females [Table/Fig-2]. The baseline characteristics of the selected patients included a Berg Balance Score (BBS) of 34±2, a Tinetti POMA score of 16±2.8 and a Falls Efficacy Scale (FES) score of 30±2.5.
Demographic distribution.
| Demographic parameters | Intervention Group (IG) | Control Group (CG) | p-value |
|---|
| Mean age | 70.5±2.5 years | 71.6±1.5 years | 0.01 |
| Gender distribution | Male: 14
Female: 16 | Male: 15
Female: 15 | 0.999 |
In the Intervention Group (IG), the BBS score improved from 37.37±7.015 to 46.67±7.08, with a p-value of 0.01. In the Control Group (CG), the scores improved from 33.63±7.95 to 36.07±7.84, with a p-value of 0.02 [Table/Fig-3]. However, in the intergroup analysis, the mean difference in the IG was greater than that in the CG, with a p-value of 0.01. Therefore, there was a statistically significant improvement in scores on the BBS in patients receiving balance training with RAS.
Intergroup analysis of Berg Balance Scale (BBS) score.
| Berg balance scale | Pre-scoring
Mean±SD | Post-scoring
Mean±SD | Paired test
p-value |
|---|
| Intervention Group (IG) | 37.37±7.01 | 46.67±7.08 | 0.01 |
| Control Group (CG) | 33.63±7.95 | 36.07±7.84 | 0.02 |
Similarly, there was an increase in the score on the POMA scale from 18.07±4.08 to 27.4±4.03, with a p-value of 0.03 in the IG. In the CG, there was an improvement; however, it was not statistically significant [Table/Fig-4].
Intergroup analysis of Tinetti Performance-Oriented Mobility Assessment (POMA) scale score.
| Tinetti-POMA scale | Pre-scoring
Mean±SD | Post-scoring
Mean±SD | Paired t-test
p-value |
|---|
| Intervention Group (IG) | 18.07±4.08 | 27.4±4.03 | 0.03 |
| Control Group (CG) | 15.53±4.15 | 16.03±4.74 | 0.22 |
On the FES, the score improved in the IG from 28.87±8.9 to 26.93±8.7, with a p-value of 0.01. In the CG, improvement was seen from 35±7.09 to 27.47±7.291, with a p-value of 0.02 [Table/Fig-5].
Intergroup analysis of the Falls Efficacy Scale (FES) score.
| Falls Efficacy Scale (FES) | Pre-scoring
Mean±SD | Post-scoring
Mean±SD | Paired t-test
p-value |
|---|
| Intervention Group (IG) | 28.87±8.997 | 26.93±8.729 | 0.01 |
| Control Group (CG) | 35±27.091 | 27.47±7.291 | 0.02 |
In the intergroup comparison, the IG receiving metronome-guided RAS showed statistically significant improvements in T-POMA and BBS scores compared to the CG (p<0.05). However, the CG showed better results on the FES score than the IG (p=0.04) [Table/Fig-6].
Intergroup comparison of all outcome measures.
| Outcome measure | Mean difference | p-value |
|---|
| Intervention Group (IG) | Control Group (CG) |
|---|
| Berg balance scale score | 9.3±2.01 | 6.01±0.38 | 0.01 |
| Tinetti Performance-oriented Mobility Assessment (POMA) scale score | 9.33±0.22 | 0.5±0.88 | 0.02 |
| Falls Efficacy Scale (FES) score | 1.94±2.3 | 7.8±2.1 | 0.04 |
Unpaired t-test
Discussion
In the present study, although improvement was observed in both groups after four weeks of treatment, patients receiving metronome-guided RAS balance training showed better outcomes than those undergoing traditional balance training.
According to a study conducted by Seidler-Dobrin RD and Stelmach GE, the incidence of falls in Indian older adults ranges from 14% to 53%, resulting in significant morbidity and mortality [6]. In this study, normal healthy elderly individuals were recruited and screened using three different fall-related outcome measures, exhibiting a range of medium to high fall risk scores before the intervention. The post-intervention score of the BBS showed improvements in both the IG and the CG; however, the IG demonstrated better results. The possible reason for this improvement is that Vestibular Function (VF) enhances sensory organisation for postural control rather than just strategy enhancement [18]. Additionally, this study considered functional and environmental aspects, such as residential ergonomics, as every subject would be exposed to different environmental challenges. Therefore, the authors recommend that dynamic balance training would be more effective when practiced in an actual home or workplace environment.
The Tinetti-POMA gait and balance subscales are highly predictive of falls and fall-related injuries in community-dwelling elderly individuals and residents of intermediate care facilities. Research conducted by Ganea R et al., on assessing the elderly for fall risk estimation found significant improvements in the Tinetti POMA scale scores [25]. They provided a structured balance training program using a metronome as auditory feedback. The present study is consistent with previous research; although both groups showed improvements on the Tinetti POMA scale, the IG demonstrated statistically significant improvements. This was made possible by the structured exercise program with auditory stimulation [7]. The reason for this improvement is that auditory stimulation controls the temporal variable of the movement, thereby increasing movement control. The fear of falls among healthy elderly individuals improved due to adaptive visual cueing, which enhanced their motor stability. This is related to the repeated facilitation of the archaeocerebellum, which has primary links with the vestibular nuclei, resulting in motor improvements [26].
The Falls Efficacy Scale (FES) measures concern regarding the fear of falling in elderly individuals, where a lower score indicates fewer chances of falling and any score greater than 70 indicates a high fear of falling risk. According to a study conducted by Li Z et al., where the FES was used as an outcome measure in a six-month follow-up study, it was revealed that the IG receiving balance training exercises exhibited fewer concerns regarding the fear of falling post the six-month training and follow-up [18]. Similarly, in the present study, the FES significantly reduced in both groups post-intervention. This improvement was attributed to the intensive training over four weeks, which included five days per week, along with the sensory orientation of the individual toward VF for inputs regarding body sway control and postural instabilities. However, the reduction in the FES score was greater in the CG during the four-week training. This implies that balance training conducted without auditory and vestibular function was also effective in reducing the fear of falling.
Limitation(s)
The time constraints of the study did not allow for follow-up assessments of fall risk using a fall diary after six months. Additionally, the study was not conducted with double blinding, which would have enhanced the inter-rater reliability of the outcome measures.
Conclusion(s)
The study concludes that Rhythmic Auditory Stimulation (RAS), using a metronome with Visual Feedback (VF), led to significant improvements in balance and a reduction in the fear of falling among healthy elderly individuals. This controlled trial also effectively demonstrated clinically significant improvements in the maintenance of balance in individuals’ familiar environments. Virtual Reality (VR) and enhanced effects, along with group therapy and the additional impact of peers, can be utilised in a similar study. Further research could include an ergonomic assessment of the subjects’ environments and interventions could be designed based on those assessments.
Unpaired t-test