The PXF is characterised by extracellular fibril production and accumulation. In 1954, Dvorak-Theobald G coined the term “PXS” to describe the accumulation of pseudoexfoliative material on the zonules, lens capsule, ciliary body and angle of the anterior chamber. PXS is a prevalent age-related disorder of the extracellular matrix that affects 10% to 20% of people over the age of 60 worldwide [1].
The disease usually affects both eyes; however, it does so asymmetrically. PXS is the major cause of PXF glaucoma, a more severe and progressive form of glaucoma [2]. Patients with PXS often experience lens subluxation, cataract formation, zonular dialysis, inadequate pupillary dilation, impaired blood-aqueous barrier function, glaucoma and both intraoperative and postoperative complications related to cataract surgery. The primary ocular characteristic of PXS is the aberrant extracellular fibrillar and PXF material that is produced and gradually accumulates in the anterior segment of the eye [3].
Deposition of pigments across the anterior chamber of the eye is another feature of PXF syndrome. When the pupil border rubs against the anterior lens capsule, the pigmented epithelium of the peripupillary iris releases melanin granules. The circulation of aqueous humor carries this pigment, which is deposited on the corneal endothelium, anterior iris stroma, anterior lens capsule and, most importantly, the Trabecular Meshwork (TM) and iridocorneal angle [4]. Patients with PXF syndrome have a higher risk of intraoperative problems during cataract surgery [5]. It has also been reported that PXF patients experience late displacement of the intraocular lens several years after cataract surgery [6]. These complications are most likely due to pathological changes in the zonules. Early detection of PXF syndrome and an accurate diagnosis are essential for minimising the risk of operative complications.
The pathogenesis of PXF syndrome is presumably multifactorial. Deposition of abnormal fibrillar, extracellular flake-like material in ocular tissues and orbital vasculature are two features of the pathological traits associated with PXF. PXF is more common in areas with high UV exposure [7]. Studies have revealed that people who live at higher altitudes or latitudes, or who are engaged in outdoor occupations, have a higher risk of developing PXF [7,8]. Additional non genetic factors have also been found to contribute to the pathophysiology of PXF, such as dietary habits (including supplements), autoimmune diseases (including antibodies), trauma and infectious agents [9].
Gonioscopy is considered the definitive method for the subjective evaluation of the Anterior Chamber Angle (ACA) [10]. Anterior Segment Optical Coherence Tomography (AS-OCT) is widely used in routine practice for diagnosing ophthalmic disorders. It provides a quantitative, accurate and non invasive analysis of the iris configuration and ACA [11]. Assessment of the ACA aids in diagnosis and in understanding the pathophysiology of glaucoma in PXF [12]. The effect of PXF on the ACA has not been studied extensively in the past.
There are very few studies evaluating the Anterior Chamber Angle (ACA) in Pseudoexfoliation (PXF) syndrome in the South Indian population using AS-OCT, to the best of the author knowledge.
The aim of the present study was to assess the ACA parameters using AS-OCT in patients diagnosed with PXF.
The primary objective of the study was to determine the changes in the morphology of the anterior chamber angle in patients with PXF.
The secondary objective of the study was to compare the gonioscopy parameters and AS-OCT parameters in patients with PXF.
Materials and Methods
The present cross-sectional observational study was conducted involving patients with PXS who attended the Ophthalmology outpatient services of the Department of Ophthalmology, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India between January 2023 and July 2024. PXS was defined as the presence of Pseudoexfoliative (PXF) deposits on the edge of the pupil and/or the anterior lens capsule during a slit-lamp biomicroscopic examination, with Intraocular Pressure (IOP) less than 21 mmHg as measured by a Goldmann applanation tonometer and no evidence of glaucomatous optic nerve damage [13]. The nature of the study was explained to the patients in their own language and written informed consent was obtained. The study adhered to the tenets of the Declaration of Helsinki and ethical approval was obtained from the Institutional Human Ethics Committee (IHEC). IHEC No: MGMCRI/Res/01/2021/78/IHEC/126.
Inclusion criteria: Patients with clinically evident pseudoexfoliative material at the pupillary border or on the anterior lens capsule in one or both eyes were included in the study.
Exclusion criteria: Patients with prior intraocular surgeries or procedures, e.g., cataract surgery, laser trabeculoplasty, laser iridotomy, laser iridoplasty, ocular trauma and evidence of peripheral anterior synechiae were excluded from the study. Additionally, patients with opaque media, such as corneal opacity that precluded the view of angle structures in AS-OCT and those with a history of glaucoma or the use of antiglaucoma medications were also excluded from the study.
Sample size: Based on the results of a study by Zheng X et al., the sample size was calculated. According to this calculation, the minimum sample size needed for the study was 46 [14].
Study Procedure
A detailed medical and ocular history, including past ocular trauma, co-morbidities and medications for both ocular and systemic conditions, was obtained. All subjects underwent a comprehensive ophthalmic examination. Visual acuity with best correction was recorded using a Snellen chart and refraction was performed at the time of presentation. Intraocular Pressure (IOP) was measured with a Goldmann applanation tonometer (Topcon CT 800). Anterior segment examination was conducted with a slit-lamp biomicroscope (Appasamy) to determine the presence of pseudoexfoliative material on the pupillary margin or anterior lens capsule in one or both eyes. Posterior segment examination was carried out using an indirect ophthalmoscope or a slit-lamp biomicroscope with a +90D lens to rule out glaucoma.
Anterior Chamber Angle (ACA) characteristics were noted using gonioscopy with a Goldmann two-mirror gonioscope (Ocular gonioscope manufactured in New Delhi). The Shaffer grading system was employed in the present study for gonioscopic evaluation. Shaffer’s gonioscopic classification of the ACA is based on the extent of visible angle structures. Grade 4 (35°-45°) represents the widest angle where the ciliary body can be visualised. Grade 3 (20°-34°) indicates an open angle where the scleral spur is visible. Grade 2 (11°-19°) refers to an angle in which the trabeculum is visible, but not the scleral spur. Grade 1 (≤10°) indicates a very narrow angle in which only the Schwalbe line and perhaps the top of the trabeculum can be identified. Grade 0 (0°) signifies a closed angle due to iridocorneal contact [15].
The AS-OCT was performed in eyes with undilated pupils using a special anterior attachment on the 3D Topcon 3D OCT Maestro (SN 1012767) from Japan, for imaging the anterior chamber. There have been very few studies focusing on AS-OCT for angle parameters in the Indian population.
The standard values of AOD500, TISA500 and TIA500 were based on the results of these parameters in a normal population from a study conducted by Zheng X et al., [14].
Standard Values based on Zheng X et al., [14]:
AOD500=500 (μm)
TISA500=0.22 (mm2)
TIA500=37.5 (degrees)
The study of Anterior Chamber Angles (ACAs) using AS-OCT was conducted as described by Khan N et al., [16]. Images were captured by instructing the patients to look straight ahead with the assistance of external fixation lights. The nasal and temporal sides of the horizontal meridian at the angles were imaged. The right eye in bilaterally symmetrical cases, the affected eye in unilateral cases and the eye with more PXF material in asymmetric cases were selected for analysis. The quadrant with better scleral spur identification was examined in the study.
Image Analysis on AS-OCT:
The scleral spur was identified as the point where there was a change in curvature of the inner surface of the angle wall, appearing as an inward protrusion of the sclera (Point A) [Table/Fig-1] [16].
The image shows the measurement of each AS-OCT parameter using the transparent sheet [15].
*AOD 500 is defined as the distance from the corneal endothelium to the anterior iris surface perpendicular to a line drawn along the Trabecular Meshwork (TM) at 500 μm from the scleral spur
*TISA 500 is defined as the trapezoidal region that includes the iris surface inferiorly, the inner corneoscleral wall superiorly, the AOD anteriorly and the inner scleral wall posteriorly
*TIA 500 is defined as an angle measured with the apex in the iris recess and the arms of the angle passing through a point on the TM 500 μm from the scleral spur and the point
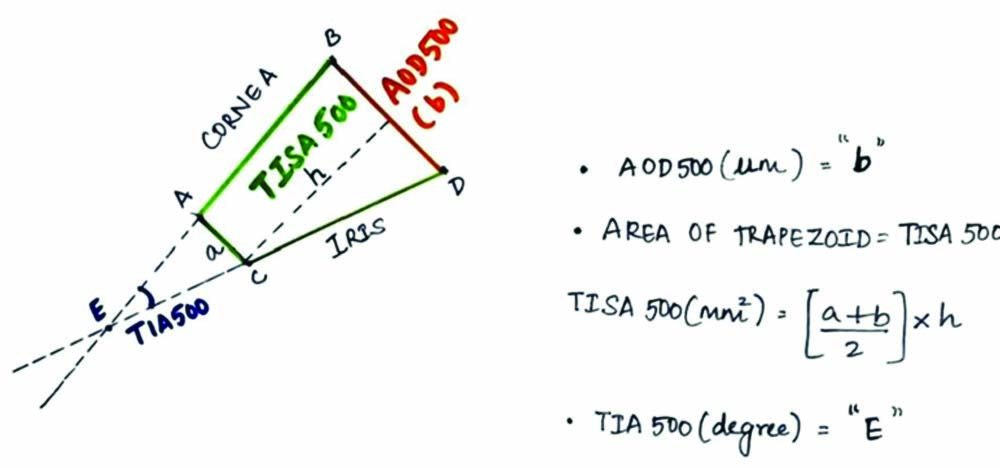
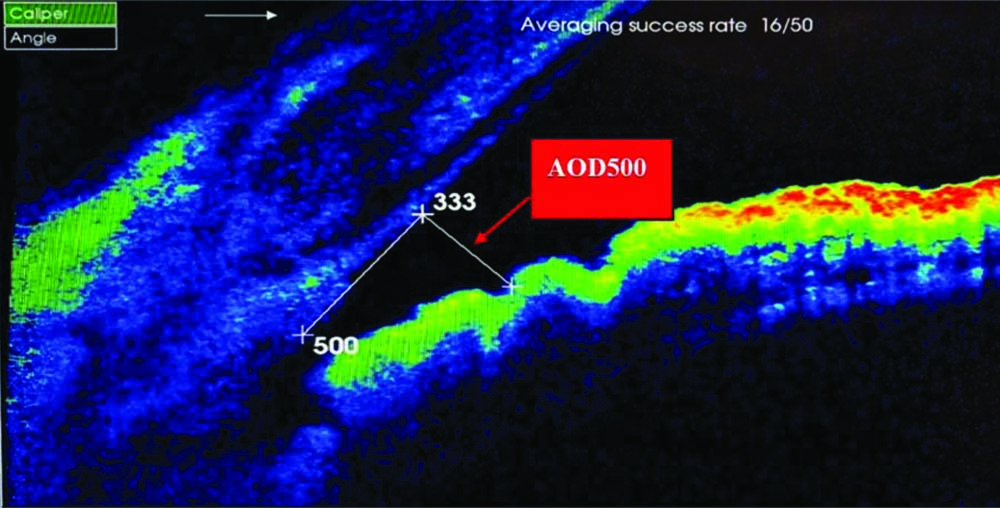
The inbuilt digital callipers of the Topcon OCT machine were used to mark a point on the posterior surface of the cornea 500 μm anterior to the scleral spur. A transparent plastic sheet was placed on the computer screen. The two points—one from the scleral spur (Point A) and another from the posterior surface of the cornea (Point B, 500 μm)—were marked on the sheet and a line was drawn to connect them [16]. Using a protractor, a perpendicular line was drawn from the second point, extending downward. The transparent sheet was placed over the screen, ensuring that the two marked points overlapped. The point where the perpendicular line intersected the surface of the iris was marked on the transparent sheet. This perpendicular line represents AOD 500 μm (line b) [Table/Fig-1,2].
AS-OCT showing the Angle Opening Distance (AOD) (AOD500) measurement in right eye of Pseudoexfoliation Syndrome (PXS) patient. AOD: Angle opening distance
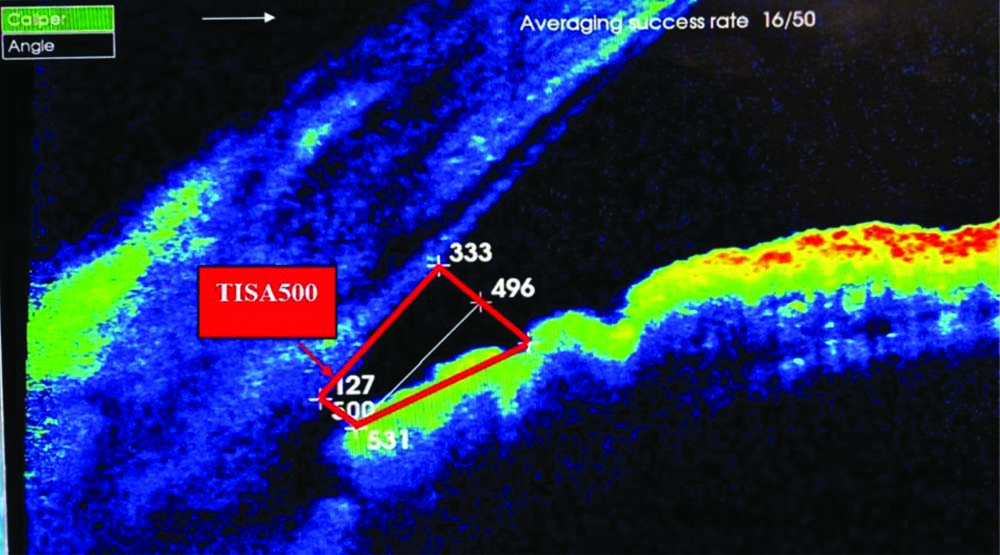
On the transparent sheet, another line parallel to AOD500 μm was drawn downward from the scleral spur (line a) [16]. The transparent sheet was placed on the screen, ensuring appropriate overlap and a point was marked where the second parallel line intersected the surface of the iris. A line was drawn connecting the two points (Point C and Point D) on the anterior iris surface as marked on the transparent sheet. This process resulted in a trapezoidal quadrilateral and the area of the trapezoid was calculated using the formula for the area of a trapezoid: area=(b1+b2)/2*h, where b1 is the height of the first base, b2 is the height of the second base and h is the height of the trapezoid. This represents TISA 500 (mm2) [Table/Fig-1,3] [16].
AS-OCT showing the Trabecular Iris Space Area (TISA500) measurement in right eye of Pseudoexfoliation Syndrome (PXS) patient.
TISA: Trabecular iris space
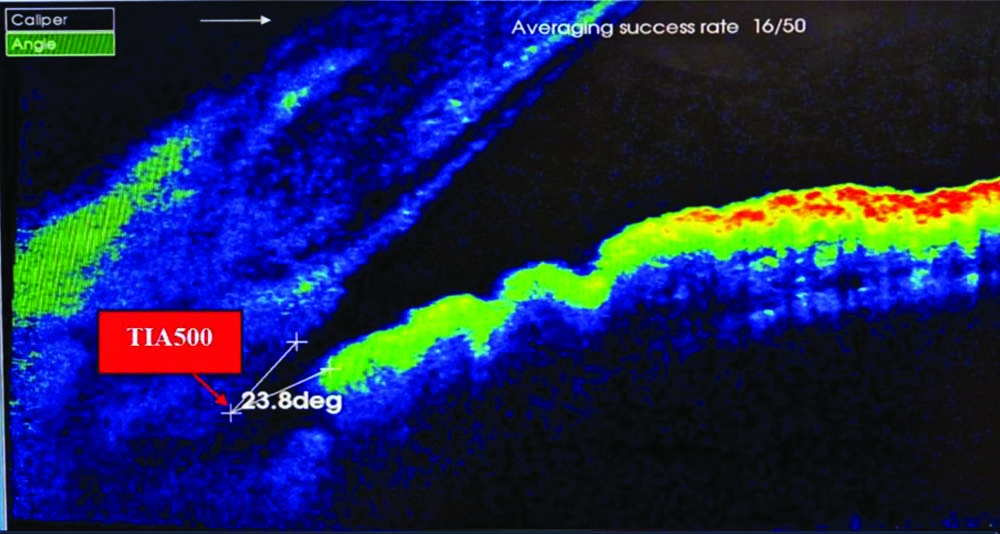
The non parallel lines of the trapezoid were extended to intersect and the point of intersection (Point E) was considered the apex of the ACA, i.e., TIA 500 (degrees) [Table/Fig-1,4] [16].
AS-OCT showing the Trabecular Iris Angle (TIA) (TIA500) measurement in right eye of Pseudoexfoliation Syndrome (PXS) patient.
TIA: Trabecular iris angle
Statistical Analysis
All statistical analysis were performed using Microsoft Excel software and the Statistical Package for Social Sciences (SPSS for Windows, Version 22.0, Chicago, SPSS Inc.). Parameters used for Anterior Chamber Angle (ACA) evaluation were described using mean and standard deviation. For descriptive analyses, mean and standard deviation were used to depict the distribution of continuous variables, while frequency (percentage) was used to represent the data distribution pertaining to categorical variables. Bonferroni correction was applied for multiple pairwise comparisons in Analysis of Variance (ANOVA). A p-value of <0.05 was considered statistically significant.
Results
A total of 60 patients fulfilling the study criteria were recruited for the study. Out of these, 9 patients (15%) were excluded due to poor imaging of the scleral spur, resulting in an analysis performed on 51 patients. Among these 51 patients, 32 right eyes and 19 left eyes were analysed. The mean age of the study group was 65.3±6.8 years. Of the participants, 26 (51%) were males, while 25 (49%) were females. The distribution of the baseline characteristics of the studied sample is shown in [Table/Fig-5].
Baseline characteristics of PXS patients.
| Baseline characterisitcs | Mean±SD |
|---|
| Age (in years) | 65.3±6.8 |
| Gender (Male:Female) | 26:25 |
Ocular Examination
The IOP measured using the Goldmann applanation tonometer in PXS eyes ranged from 10 mmHg to 18 mmHg, with a mean of 14.15±2.02 mmHg.
Gonioscopy parameters in Pseudoexfoliation Syndrome (PXS): Gonioscopy using a two-mirror gonioscope revealed that 30 patients (58.8%) had Grade 3 (open) angles, 15 patients (29.4%) had Grade 2 (narrow) angles and 6 patients (11.8%) had Grade 4 (wide open) angles. None of the patients had Grade 0 (extremely narrow) or Grade 1 (closed) angles. In addition, the presence of the Sampolesi line was observed in 18 patients (35.3%) with PXS. Highly pigmented TM was seen in 22 patients (43.1%) and Pseudoexfoliation (PXF) in the angle was noted in 8 patients (15.7%).
AS-OCT parameters in Pseudoexfoliation Syndrome (PXS): The parameters of the ACA in PXF syndrome using AS-OCT is represented in [Table/Fig-6] [14]. From the AS-OCT images, AOD500, TISA500 and TIA500 were calculated. The mean AOD500 in PXS eyes was 386.9±93.7 μm, ranging from 234 μm to 610 μm. The mean TISA500 in PXS eyes was 0.13±0.02 mm2, with a range from 0.09 mm2 to 0.21 mm2, while the mean TIA500 in PXS eyes was 29.2±5.2°, ranging from 20.8° to 40.5°.
Profile of AS-OCT parameters in Pseudoexfoliation Syndrome (PXS) eyes using One sample t-test was analysed. PXS eyes shows statistically significant reduction (p=0.001) in all three AS-OCT measured angle parameters [14].
| Study variables | Standard value (based on Zheng X et al.,) | PXS patients | Mean difference between PXS patients and standard value based on Zheng X et al., [14] | Significance (p-value) |
|---|
| AOD500 (μm) | 500 | 386.9±93.75 | -113.05 | 0.001* |
| TISA500 (mm2) | 0.22 | 0.13±0.02 | -0.08 | 0.001* |
| TIA500 (degree) | 37.5 | 29.2±5.21 | -8.24 | 0.001* |
PXS: Pseudoexfoliation syndrome; AOD: Angle opening distance; TISA: Trabecular iris space area; TIA: Trabecular iris angle; *p<0.05, statistically significant
Assuming standard values of AOD500, TISA500 and TIA500 as 500 μm, 0.22 mm2 and 37.5°, respectively [14], the PXS eyes in the present study demonstrated a statistically significant reduction in all three AS-OCT measured angle parameters.
Comparison between AS-OCT and gonioscopy parameters: The comparison between AS-OCT measured angle parameters and different grades of gonioscopy is represented in [Table/Fig-7]. The mean AOD500, TISA500 and TIA500 correlated well with the grading of angles observed by gonioscopy. A statistically significant difference was noted between the AS-OCT parameters and different grades of angles on gonioscopy.
AS-OCT parameters among different Gonioscopy grades in PXS eyes. Post-hoc analysis with the Dunn-Bonferroni test showed a statistically significant increase in all three AS-OCT parameters among different gonioscopy grades (p=0.001). All three AS-OCT parameters showed a linear correlation with grades of gonioscopy.
| Grades of gonioscopy (Shaffer grading) |
|---|
| AS-OCT parameters | Grade 2
(n=15) | Grade 3
(n=30) | Grade 4
(n=6) | p-value | Multiple comparisons (Bonferroni correction) |
|---|
| AOD500 (μm) | 301.26±42.6 | 403.53±64.5 | 518.16±119.6 | 0.001* | Grade 2 vs Grade 3*
Grade 3 vs Grade 4*
Grade 2 vs Grade 4* |
| TISA500 (mm2) | 0.11±0.01 | 0.14±0.02 | 0.17±0.03 | 0.001* | Grade 2 vs Grade 3*
Grade 3 vs Grade 4*
Grade 2 vs Grade 4* |
| TIA500 (degree) | 26.68±3.9 | 29.02±4.6 | 36.8±4.3 | 0.001* | Grade 2 vs Grade 4*
Grade 3 vs Grade 4*
Grade 2 vs Grade 3 |
PXS: Pseudoexfoliation syndrome; AOD: Angle opening distance; TISA: Trabecular iris space area; TIA: Trabecular iris angle; *p<0.05, statistically significant
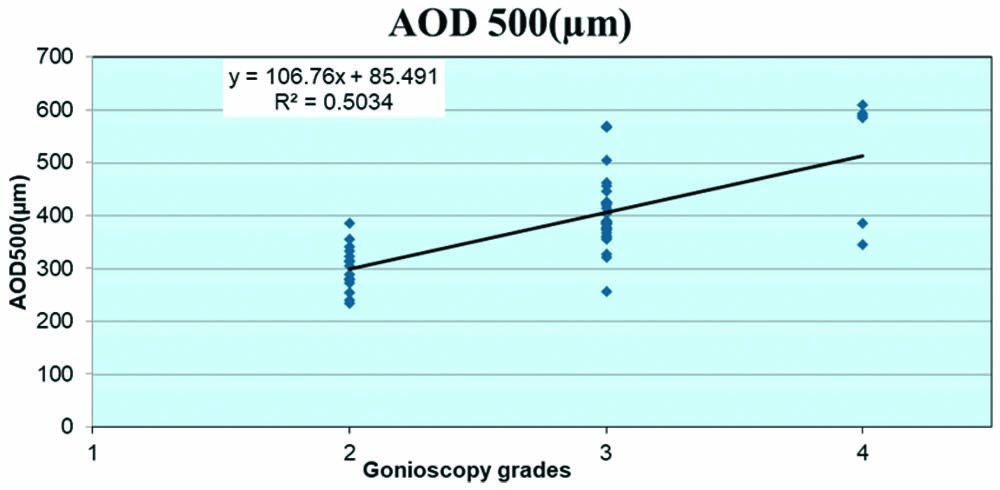
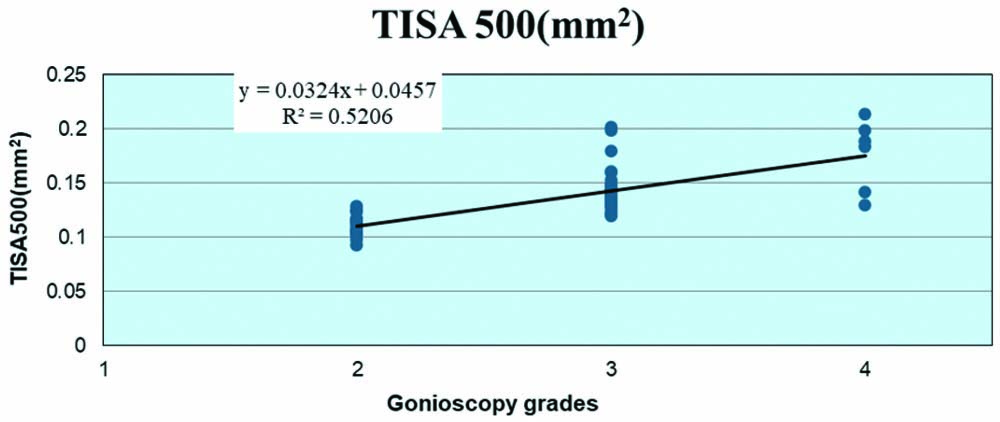
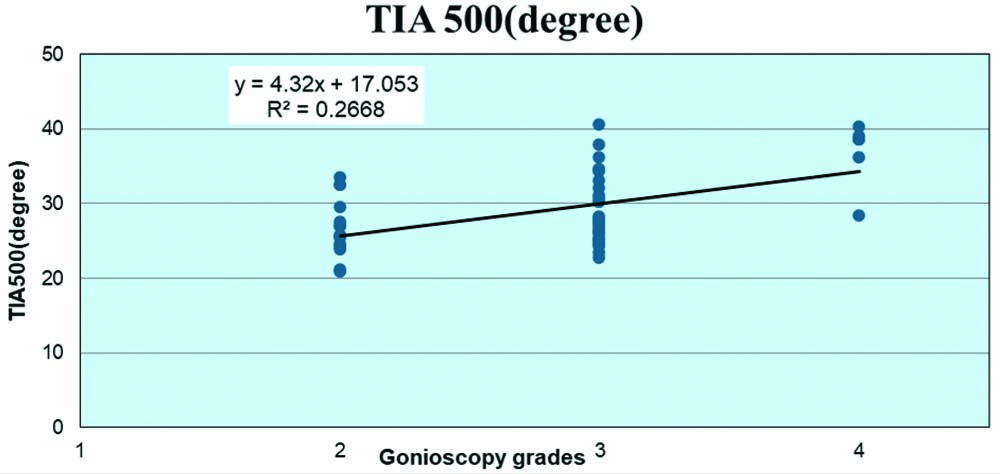
The grades of angles by gonioscopy and the values of AOD500, TISA500 and TIA500 all exhibited a linear correlation is demonstarted in [Table/Fig-8,9 and 10]. Of these, the correlation coefficients for AOD500 and TISA500 were R2=0.70 and R2=0.72, respectively, indicating a higher level of correlation with the grades of angles observed by gonioscopy compared to TIA500, which had a correlation coefficient of R2=0.50.
The scatterplot shows the linear correlation between AOD500 in different grades of angle by gonioscopy.
The correlation coefficients of AOD500 is R2=0.70.
AOD: Angle opening distance
The scatterplot shows the linear correlation between TISA500 in different grades of angle by gonioscopy.
The correlation coefficients of TISA500 is R2=0.72.
TISA: Trabecular iris space
The scatterplot shows the linear correlation between TIA500 in different grades of angle by gonioscopy.
The correlation coefficients of TIA500 is R2=0.50; TIA: Trabecular iris angle
Discussion
The present study on AS-OCT characteristics in patients with Pseudoexfoliation Syndrome (PXS) demonstrated reduced values in all three AS-OCT parameters: AOD500, TISA500 and TIA500. Among these parameters, AOD500 and TISA500 showed a good correlation with different grades of angles observed during gonioscopy.
Pseudoexfoliation (PXF) is more prevalent with increasing age. Similar to the observations made by Dvorak-Theobald G and Warjri GB et al., most of the patients in the present study were around the sixth decade of their lives, which may explain the higher number of patients with advanced age [1,17]. A study conducted by Vijaya L et al., found that increasing age had a significant association with PXF [18].
The sex distribution in the present study revealed a slight predilection toward the male sex, which aligns with the findings of Warjri GB et al., [17]. However, some studies have reported a female preponderance [18]. The higher percentage of PXF in men in the present study may relate to the fact that men in developing nations tend to seek medical attention more frequently than women, as well as the necessity for women to accompany men when seeking medical care.
Kozart DM and Yanoff M observed that 80% of PXF patients had normal IOP in the affected eye at the time of initial diagnosis [19]. In accordance with these observations, our study also noted that IOP was within the normal range.
Among the angle characteristics observed through gonioscopy, the authors found highly pigmented TM to be the most common. Roth M and Epstein DL, in a study of unilateral PXS patients, observed that TM in PXS eyes was more pigmented than in the fellow eye. In fact, TM pigmentation may occur before PXF appears in the anterior segment [9]. In patients with an asymmetrical presentation of PXS, the eye with more TM pigmentation was also more likely to have glaucoma [20].
The normative data for AS-OCT measured angle parameters for Indian eyes is currently not available in the literature; therefore, the basis for normality was derived from a study conducted by Zheng X et al., [14]. Comparing the present results to the normative data, the present study showed a decrease in AS-OCT measured angle parameters (AOD500, TISA500, TIA500) in PXS eyes. This finding is consistent with many other studies. According to these results, there may be potential weakening of zonular fibers and forward lens shifting in PXF eyes, which aligns with earlier UBM studies conducted by Damji KF et al., and Sbeity Z et al., [21,22].
Zheng X et al., demonstrated reduced angle parameters, such as TISA500 and TIA500, in PXF eyes in the light but did not find a significant difference between PXF and controls in the dark. Additionally, they reported that PXF eyes had a considerably lower mean dark-to-light transition on the AOD500 compared to their fellow eyes [14]. Mohammadi M et al., observed a narrowing of angle parameters by AS-OCT in PXS eyes compared to non PXS eyes in the Iranian population [23]. In the Polish population, among patients with senile cataracts, those with PXS had narrower angles than those without PXS [24]. Dembski M et al., noted a thicker iris, along with a smaller Anterior Chamber Depth (ACD) and lower angle parameters in patients with PXS. They suggested that all these parameters may contribute to the development of PXF glaucoma in PXS patients [25].
In the present study, all three AS-OCT parameters—AOD500, TISA500 and TIA500—showed a positive correlation with the clinical gonioscopic assessment of angles. AOD500 and TISA500 exhibited a strong positive correlation, while TIA500 showed a weak positive correlation [Table/Fig-8,9 and 10]. Since AOD is a point distance, it is possible that discrete changes in iris thickness or contour in the TM might affect the angle width. Such variations in the iris may have averaged out over the region, making the area measurement TISA500 less accurate than AOD500. A study by Narayanaswamy A indicated that AOD500 is the most accurate angle measurement for identifying individuals with narrow angles on gonioscopy in AS-OCT images [26]. This study implies that PXF syndrome is characterised by its significant impact on the anterior segment, which includes narrow angle parameters, as well as the presence of pigmented TM and the Sampolesi line in the angles. Anterior segment OCT can identify distinctive anterior segment characteristics of PXS, which may assist clinicians in managing the condition effectively.
Limitation(s)
The limitation of the present study is the absence of a comparison between PXS and non PXS eyes.
Conclusion(s)
Peripheral ACA parameters, as measured by AS-OCT, are reduced in eyes with PXS. The angles measured by AS-OCT correlate well with those assessed by gonioscopy.