Central Nervous System (CNS) infarction refers to the death of brain, spinal cord, or retinal cells attributable to ischaemia, based on pathological, imaging, or other objective evidence of cerebral, spinal cord, or retinal focal ischaemic injury in a defined vascular distribution. Alternatively, it can be identified through clinical evidence of cerebral, spinal cord, or retinal focal ischaemic injury based on symptoms persisting for atleast 24 hours or until death, with other aetiologies excluded [1].
Motor impairments are a common consequence of stroke, affecting approximately 80% of all cases and leading to permanent disability and reduced quality of life [2]. The prevalence of motor impairment post-stroke is notably high, with a reported rate of 77% in the upper limb and 72% in the lower limb. This indicates that a significant proportion of stroke survivors struggle with motor deficits, which can greatly impact their ability to carry out daily activities and lead to a diminished quality of life [3].
Approaches focusing on specific tasks or functional training are frequently employed to enhance motor control and functional abilities in the paretic lower limbs [4-6]. Functional training has been shown to enhance neuroplastic changes, leading to better motor recovery [7]. Weight-bearing in standing, gait training and sit-to-stand exercises are common functional training methods employed for the lower extremities [8-10]. The majority of these interventions have been tested in individuals in the late subacute or chronic phases of stroke. The implementation of functional training in the early subacute phase of stroke is scarce in research [11]. The initiation of early rehabilitation interventions has been reported to result in better motor recovery [12,13]. Profound muscle weakness in the early phases of stroke could be one of the major limitations in implementing functional activities similar to those used in the late subacute and chronic phases of stroke. Ramachandran S et al., [14] reported that even minimal attempts to hold the upper limb on an unstable surface, such as a therapy ball, can provoke contractions in the proximal muscles of the upper limb in early subacute stroke subjects. The authors assumed that activities like holding the limb on an unstable surface could be attempted by post-stroke individuals with minimal motor control. We sought to replicate a similar intervention in the lower extremity of subjects in the early subacute phase of stroke. We hypothesise that the inclusion of simple exercises like these is likely to improve adherence to exercise interventions post-stroke, where muscle weakness is one of the limiting factors for adherence to therapy [15]. The aim of the present study was to test the effect of training that involves holding the paretic lower extremity on an unstable surface on the motor control of the paretic lower extremity. We hypothesised that such training could improve the contractions of selected muscles in the paretic lower extremity, reflecting the improvement in motor control. To investigate this, we aimed to assess changes in muscle contractions using surface electromyography (SEMG).
Materials and Methods
The study is a randomised control trial in which subjects were recruited from an acute stroke care center associated with a university teaching hospital at Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India, from February 2024 to June 2024. It was approved by the Institutional Ethical Committee (REF: CSP/23/SEP/136/821). The present study was registered in the Clinical Trial Registry India with the reference number CTRI/2024/02/062808. Subjects meeting the inclusion criteria were included in the study after obtaining written informed consent from willing participants.
Inclusion and Exclusion criteria: Subjects with a first-time ischaemic stroke who can follow commands to perform the activities for the study, who exhibit motor recovery at Brunnstrom stage 2 or below in the lower extremity [16] and who have the ability to maintain unsupported sitting in bed were included in the study. Subjects with any other neurological or orthopaedic impairments that would limit their ability to undertake the activities, those with profound spasticity and those with a history of lower limb injury that could affect the outcome of the study were not included. Subjects with a profound proprioception deficit in the paretic lower extremity were also excluded.
Sample size calculation: The sample size was calculated based on an initial sample of 10 stroke survivors who met the inclusion criteria. They underwent training in a supine position, similar to the study protocol, to stimulate muscle contraction in the gluteus medius. Pre- and postintervention surface electromyographic measurements were taken according to the standard protocol. The difference was considered for sample size calculation, with an alpha error of 0.05, a power of 0.95 and an effect size of 0.9.
The sample size was calculated using the formula N={(r+1)(Zα/2+Z1-β)2 Sp2} / rd2, where r is the ratio of the sample size between the groups, Zα/2 is the Z value for alpha, Z1-β is the Z value for power, Sp is the pooled standard deviation of the groups obtained from the pilot study (3.61) and d is the difference between the means (4 μV) [17]. The calculated number was 25 subjects in each group. Considering a 10% attrition rate, the sample size was determined to be 28 per group.
Study Procedure
The SEMG recordings were taken from the paretic gluteus medius, tensor fasciae latae and quadriceps femoris muscles of all participants on the day of inclusion in the study. Baseline SEMG for the tensor fasciae latae and gluteus medius muscles was recorded with participants in a supine position, while participants were positioned in a high sitting position for the quadriceps femoris muscle. Electrode positioning for EMG was standardised based on the SEMG for the Non Invasive Assessment of Muscles (SENIAM) guidelines. The SENIAM guidelines were developed through a grant from the European Community as part of the BIOMED-2 program. Detailed information can be found at www.seniam.org [18].
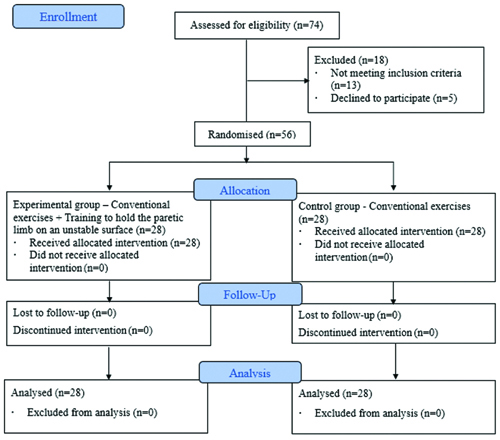
According to the guidelines, for the tensor fasciae latae, the active electrode was placed on the lateral aspect of the thigh, the reference electrode was placed on the anterior superior iliac spine and the ground electrode was placed on the lateral condyle of the femur. Participants were instructed to attempt to abduct their paretic limb. For the gluteus medius, the active electrode was placed on the posterolateral aspect of the muscle belly, the reference electrode was placed on the posterior superior iliac spine and the ground electrode was placed on the lateral condyle of the femur. Participants were similarly instructed to attempt to abduct their paretic limb. For the quadriceps femoris, the active electrode was placed at the muscle belly, the reference electrode was placed 5 cm below the anterior superior iliac spine and the ground electrode was placed above the patella. Participants were instructed to attempt to extend their paretic limb. SEMG was recorded using Neuro Trac Software 4.0 from VM (Verity Medical Ltd., United Kingdom) with silver chloride adhesive electrodes. Participants were randomly allocated using block randomisation of four into two groups [Table/Fig-1].
Consolidated Standards of Reporting Trials (CONSORT) flow diagram.
The control group received routine care, while the experimental group received routine care along with training to hold their paretic lower limb on unstable surfaces in both supine lying and high sitting positions. In routine care, participants in both groups received 45 minutes of physiotherapy, including facilitatory techniques for the upper extremity, lower extremity and trunk, as well as functional training based on the concept of the Motor Relearning Program [Table/Fig-2] [5]. Additionally, the participants in the experimental group were instructed to stabilise or hold their paretic limb on a ball, ensuring that the ball remained in place [Table/Fig-3,4 and 5]. The interventions were provided for 10 sessions over 10 days.
Conventional exercises [5].
In lying:
• Passive movements to the paretic upper limb and lower limb.
• Facilitating techniques by tapping on the muscle belly to improve muscle activity.
• Active assisted exercises to the upper limb and lower limb.
• Pelvic bridging exercise.
• Quadricep end range exercises in flexion and extension.
• Bed mobility exercises. |
High sitting:
• Sitting up from lying.
• Weight bearing to upper limb.
• Reaching activities with therapist by the side. |
Standing:
• Balance training in static and dynamic with therapist by the side.
• Weight bearing exercises.
• Weight shifting exercises. |
Training to hold paretic lower limb on unstable surface exercises.
| In lying: Patient lying on stable surface (bed) and trained to hold the paretic lower limb on the unstable surface. |
| High sitting: Patient in high sitting on stable surface (bed) and the paretic lower limb is placed on the unstable surface with hip and knee at 90°. |
Training to hold the paretic lower limb on unstable surface for Gluteus medius, Tensor fascia lata in supine lying.

Training to hold the paretic lower limb on unstable surface for Quadriceps femoris in high sitting.

Postintervention, the SEMG recordings from the gluteus medius, tensor fascia lata and quadriceps femoris muscles were taken six hours after the completion of ten sessions of therapy, following a procedure similar to that of the baseline recording. The postintervention measurement of EMG was taken six hours after the 10th session of therapy to avoid the immediate effects of training.
Statistical Analysis
The average SEMG values of each muscle were taken for data analysis. The maximum value among the three trials was considered for analysis. Within-group and between-group data were tested using paired and unpaired t-tests, with a significance level set at p≤0.05.
Results
A total of 74 subjects were screened for eligibility, and 56 subjects were included to meet the sample size. All 28 subjects enrolled in the control and experimental groups completed the study. The mean age of participants in the control group was 65.53±8.19 years, while the mean age of participants in the experimental group was 57.96±10.89 years. The number of individuals with a right cerebrovascular accident in the experimental group and control group were 13 and 12, respectively. The number of individuals with a left cerebrovascular accident in the experimental group and control group were 15 and 16, respectively.
The pre- and postintervention values of surface EMG obtained from both the experimental and control groups is shown in [Table/Fig-6]. Within-group testing demonstrated that the changes in the EMG recordings of the Quadriceps, Tensor Fascia Lata and Gluteus Medius were statistically significant at p-value <0.05. The increase in EMG activity indicates an increase in the contraction of all three muscles in both the control and experimental groups; however, it is noteworthy that the magnitude of increase in the EMG recordings was greater in the experimental group compared to the control group for all three muscles. The change in muscle activity was assessed using the difference between pre- and postintervention values. These values reveal that the change in quadriceps activity in the experimental group was marginally higher compared to the Tensor Fascia Lata and Gluteus Medius, whereas, in the control group, the changes in the Tensor Fascia Lata and Gluteus Medius activity were equal and marginally higher than that observed in the quadriceps [Table/Fig-6].
Average electromyography (μV) output for selected lower extremity. muscles in stroke patients.
| Mean μV±(SD)/Muscles | Within the group comparison | Between group comparison |
|---|
| Experimental group (n=28) | Control group (n=28) | Pre post difference | tb value | pb value |
|---|
| Pre | Post | ta value | pa value | Pre | Post | ta value | pa value | Experimental# | Control# |
|---|
| QF | 15.79 (6.04) | 26.18 (6.02) | 34.16 | 0.001 | 18.22 (7.43) | 21.19 (7.13) | 9.73 | 0.001 | 10.39 (1.61)b | 2.97 (1.61) | 17.2 | 0.001 |
| TFL | 13.51 (4.36) | 22.50 (5.64) | 17.74 | 0.001 | 15.29 (5.39) | 18.33 (4.90) | 11.25 | 0.001 | 8.98 (2.68)b | 3.04 (1.43) | 10.35 | 0.001 |
| GMed | 16.45 (5.94) | 25.93 (6.69) | 14.84 | 0.001 | 18.05 (5.87) | 21.07 (5.89) | 10.32 | 0.001 | 9.48 (3.38)b | 3.02 (1.55) | 9.19 | 0.001 |
QF: Quadriceps femoris; TFL: Tensor facia lata; GMed: Gluteus medius; SD:Standard deviation; *Significant <0.05; a- paired t test, b- unpaired t test; #Difference between pre and post value is used
Preintervention values were analysed to ascertain the comparability of the groups at the commencement of the intervention. The independent t-test indicated no significant difference for the mean surface EMG values of Quadriceps Femoris, t(54)=1.34, p=0.09; Tensor Fascia Lata, t(54)=1.35, p=0.09; and Gluteus Medius, t(54)=1.01, p=0.15, revealing that the groups were statistically identical before the initiation of the intervention. The pre- and postintervention difference within each group was used to test the difference between the experimental and control groups. It is evident that the difference in EMG values of all three muscles is higher in the experimental group compared to the control group, reaching statistical significance at p-value <0.05. As EMG represents muscle activity, the increase in Quadriceps contraction is higher in the experimental group compared to the control group, followed by Tensor Fascia Lata and Gluteus Medius [Table/Fig-6].
The effect size of the intervention was determined using Cohen’s d. The effect size was larger for all three recordings in the study. The Cohen’s d for Quadriceps Femoris, Tensor Fascia Lata and Gluteus Medius were 4.60, 2.76 and 2.45, respectively. This reveals that the intervention had a significant impact on the outcome.
Discussion
In the present study, it was observed that an attempt to hold the hemiparetic lower limb on an unstable surface stimulated muscle contractions in selected muscles in the paretic lower extremity. We limited the testing to the gluteus medius, tensor fasciae latae and quadriceps femoris and found that after training, the muscle contractions in both groups improved. The action of holding the paretic foot on an unstable surface, such as a ball, may be construed as a goal-directed activity. Neuroplasticity is said to be enhanced by goal-directed activities. Ramachandran S et al., tested the impact of attempts to hold the affected upper extremity on an unstable surface and reported that the training improved muscle contraction around the shoulder girdle [14].
Functional training, or goal-directed activity for the lower extremity, is frequently utilised to enhance functions such as sitting to standing [9,19] and standing and walking [20]. These interventions are predominantly applied in the late subacute and chronic phases of stroke [11]. There is a dearth of studies exploring the effects of functional training in the early subacute phase of stroke. Given the anticipated enhancement of neuroplasticity through functional training [7], its implementation in the early phases of stroke is presumed to offer greater benefits for motor recovery [12] and may be more appealing for patients’ engagement in rehabilitation. In the present study, the intervention has been tested in the early subacute phase of stroke.
A scoping review on functional training for the lower extremity reveals that stroke rehabilitation currently lacks a standard protocol for this type of training. As part of functional training, the review also suggests incorporating activities such as object manipulation with the lower extremity [11] and recommends controlling a ball with the affected lower extremity as a training component [21]. The present study revealed that efforts to hold the lower extremity on an unstable surface, such as a ball, could provoke muscle contractions in the paretic lower extremity. This form of exercise, which we assumed to require minimal motor activity and minimal caregiver assistance, would be suitable for patients in the early subacute phase of stroke with profound weakness. Additionally, adherence to these exercises may be better compared to traditional exercises that involve greater mobility, as patients can easily perform these exercises with less physical effort and minimal equipment [15].
Typically, involvement in therapy and engagement in therapy are expected to improve when training replicates everyday activities. Generally, the lower extremity is used to manipulate objects, such as adjusting footwear, picking up items from the ground, or moving and kicking objects to create space when the upper extremities are occupied. In the present study, the participants were instructed to hold the lower extremity on a ball; similarly, functional activities such as moving objects, kicking objects, sliding the foot into footwear and picking up objects from the floor could be integrated into functional training for the lower extremity.
Many stroke patients report difficulty adhering to exercises at home. A frequent yet significant obstacle in adhering to home-based rehabilitation is muscle weakness, along with the absence of necessary equipment and facilities for training, as well as the inability of family members to provide the same level of guidance and supervision that a therapist offers [15,22]. The exercise used to hold the hemiparetic lower limb on an unstable surface in order to provoke muscle contractions involves a ball and a slippery, rectangular board was applied in the present study. These exercises are easy for the patient to perform, as they require only a ball as an instrument, which is simple to acquire and demand less caregiver handling and less motor activity. This concept can be utilised to create a range of exercises that target various muscle groups and offer diverse training options.
The present study demonstrates that training to hold the paretic lower limb on an unstable surface is a successful technique for inducing muscle contraction in specific lower extremity muscles. As a result, this approach can be incorporated into training regimens to aid in the recovery of paretic lower limbs during the early subacute stage of stroke rehabilitation.
Limitation(s)
All participants had middle cerebral artery infarcts. Although it was not intentional, subjects with anterior cerebral artery infarcts were not included in the study group. The outcome may vary in subjects with anterior cerebral artery infarcts due to its predominant supply to cortical areas responsible for lower extremity control.
Conclusion(s)
An effort to hold the hemiparetic lower limb on an unstable surface provokes muscle contraction in selected muscles of the lower extremity. Adherence to these exercises may be better compared to traditional exercises that involve greater mobility, as patients can easily perform them with less physical effort and minimal equipment. This approach can be used as training with minimal movement to help elicit muscle contraction.
QF: Quadriceps femoris; TFL: Tensor facia lata; GMed: Gluteus medius; SD:Standard deviation; *Significant <0.05; a- paired t test, b- unpaired t test; #Difference between pre and post value is used