Case Report
A 53-year-old male patient came to the Outpatient Department (OPD) with the complaint of swelling in the mid-lower back (lumbar) region, measuring 2×3 cm. The swelling has been slowly increasing in size over the last few months and is associated with moderate pain. The swelling is localised and occurs intermittently, worsening when touched. It has become progressively larger and uncomfortable for the patient.
The patient reported that he had undergone several sessions of treatment at different private hospitals, which involved conservative management; however, he did not notice any marked improvement. The patient has no history of fever, night sweats, or sudden weight loss at any time in the past. He did not report any other complaints that could be related to the case.
A well-defined swelling discovered during a physical examination was located in the lumbar region of the patient’s body. The swelling was firm and non fluctuant, moderately painful to the touch, without any overlying changes in skin colour or erythema. Considering the anatomic site and clinical characteristics, an initial differential diagnosis of a lipoma or an infected sebaceous cyst was proposed. Clinically, the patient was otherwise stable and did not exhibit features suggestive of a systemic infection. Additional assessment was performed using ultrasound.
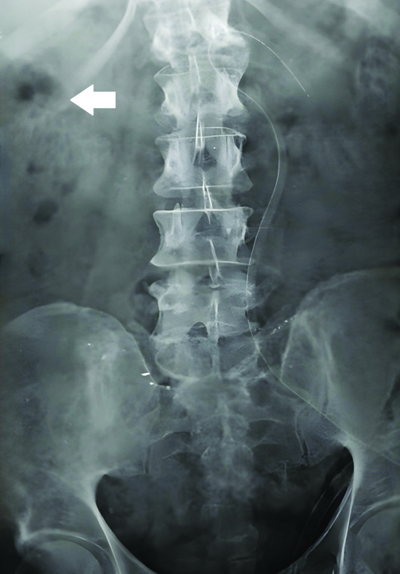
On ultrasound, a well-defined, oval, heterogeneously hypoechoic collection with internal echogenic fat lobules was observed. This finding did not correlate with a lipoma (which is typically homogeneously hypoechoic) or a sebaceous cyst (which is usually anechoic with posterior enhancement). The lack of prominent vascularity on Doppler examination diminished any signs of an active infectious process or vascular lesion. When a lumbar hernia was considered as a possibility, the discontinuity with abdominal contents ruled this option out. An X-ray of the lumbosacral spine revealed a hypodense translucent lesion, as seen in [Table/Fig-1].
X-ray of lumbosacral spine shows a hypodense translucent lesion.
The size of the collection material was 4×2.3 cm, with a calculated volume of approximately 28 cc. It extended superior and lateral to the superficial muscular fascia; superficial vascularity was not identified on Doppler examination. Based on these findings, the possibility of a lumbar hernia with fat necrosis was considered as a differential diagnosis. However, further diagnostic work-up was necessary for the present case.
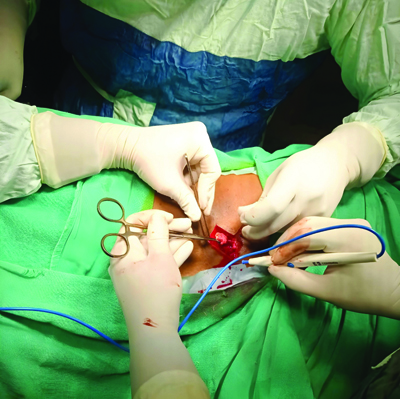
While early investigations suggested the potential for a lumbar hernia, the findings during surgery did not support this opinion. No gross evidence of a hernia was observed during the intraoperative procedure. The surgical process began after placing the patient in the prone position, thereby allowing access to the swelling over the mid-lower back region. A 5 cm long incision was made following the intubation of the patient, with adherence to aseptic measures. The incision was made in the middle of the medial aspect, precisely over the swollen mass. This incision site was chosen because it provided direct access to the mass without invading other nearby major structures. The incision was deepened through the skin and subcutaneous tissues and no injury was inflicted on any neighbouring structures, as seen in [Table/Fig-2].
The incision deep to the skin and subcutaneous tissues.

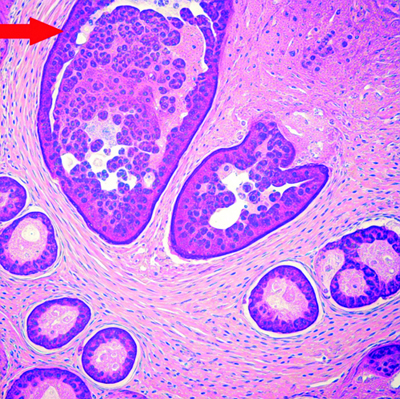
As the dissection advanced deeper into the subcutaneous layer, the initial impression of a hernia sac and/or herniated abdominal contents was not identified, contrary to observations from preoperative imaging studies. As dissection progressed, an abscess cavity was identified within the intramuscular plane, lying between the muscle fibers, as seen in [Table/Fig-3].
Abscess cavity was identified within the intramuscular plane.
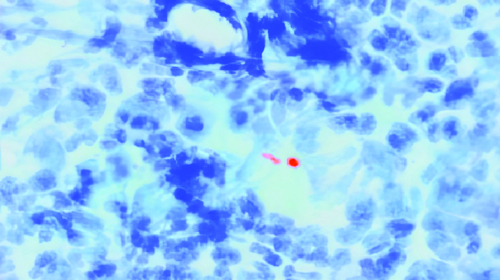
The abscess was an encapsulated collection of pus, enclosed in deeply red-coloured inflamed skin tissue. Special attention was paid to the use of a surgical retractor to gain access to the site while the abscess cavity was being opened. Thick, purulent material was drained from the cavity and a sample of the pus was used for the detection of the causative agent in the microbiological and cytological examination. The cytology report on the pus fluid sample was labelled as originating from the right infraclavicular region. A sample of less than 0.5 mL of reddish, blood-tinged, turbid fluid was taken. The cytological examination revealed a haemorrhagic background in which polymorphonuclear cells, lymphocytes and macrophages were present. These cells were arranged in small clusters as well as diffusely distributed to varying extents in the smears, suggestive of inflammation. At this stage, the precise nature of the underlying condition remained unclear, although an infectious process was suspected. The cytological examination and histopathology are shown in [Table/Fig-4].
Cytological examination histopathology {Haematoxylin and Eosin (H&E) stain, 10x power}.
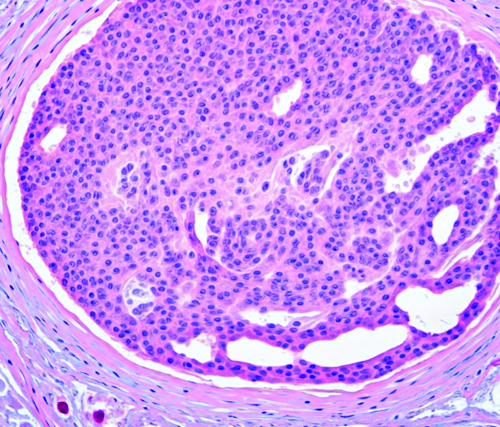
Histopathological examination was performed on a sample that was removed from the left infrascapular region. The specimen consisted of several variously sized blackish tissue fragments, which measured a total of 7×4×1 cm. Examination under the microscope further confirmed tubercular changes, characterised by caseous necrosis, epithelioid granulomas, Langhans giant cells, chronic inflammatory cells and extensive fibrosis. These findings supported the clinical diagnosis of tubercular inflammation, indicating the possibility of a tuberculous abscess over a hernial or fat necrotic aetiology. The histopathological examination of the left infrascapular region sample confirming tubercular changes is shown in [Table/Fig-5].
Histopathological examination of left infra-scapular region sample confirming tubercular changes {Haematoxylin and Eosin (H&E) stain, 10x power}.
In the microbiological examination, the specimen received from the pus intraoperatively was positive for Mycobacterium Tuberculosis (MTB) through Ziehl-Neelsen staining, implying a tubercular origin. There was no other bacterial growth isolated on aerobic or anaerobic culture. The histopathology of the microbiological examination of the intraoperative pus is seen in [Table/Fig-6].
Histopathological examination of abscess cavity intraoperative pus sample with presence of Mycobacterium Tuberculosis (MTB) bacteria (Red coloured). {Ziehl-Neelsen (ZN) stain, 100x power}.
Once the abscess had been adequately drained, the cavity was washed with saline to minimise the possibility of harbouring infectious material. Nonetheless, there was engorgement of the surrounding soft tissue; otherwise, no signs of active bleeding or other complications were noted. The abscess cavity was then left open to granulate and any remaining infection was allowed to discharge freely. A sterile dressing was placed over the wound and a small drain was sutured to help control postoperative effusion or pus. There were no complications recorded during the surgery and the patient did not complain of any discomfort throughout the process of the tubercular intramuscular abscess operation. After the operation, the patient was observed for any signs of infection, such as fever or complications in the operated region. The patient had a favourable outcome following the initiation of ATT after surgery, based on histopathological evidence of TB.
As the first few weeks went by, he reported relief from localised pain and no soreness in his hands. Subsequent visits demonstrated continued granulation tissue formation and skin healing, as well as the absence of further evidence of infection, including reinfection with MTB, or other TB-related complaints such as fever, weight loss, or night sweats.
Regarding the treatment, the patient continued the ATT regimen he was on, which included first-line anti-TB medications (isoniazid, rifampicin, pyrazinamide and ethambutol). To monitor safety and compliance and to prevent the mentioned side-effects, liver function tests and other side-effects were constantly evaluated. Eventually, the abscess cavity was closed and imaging studies conducted afterward did not reveal evidence of residual or recurrent disease. After the surgery, the patient experienced no complications and over the next several days, his condition gradually stabilised. He had no complaints, so he was discharged with wound care instructions and a plan for follow-up visits.
In a one-year follow-up, the symptoms had resolved, there were no new lesions and, more importantly, there was no systemic involvement, suggesting a favourable outcome. The issue of discontinuing ATT was discussed with the patient and he was informed of the consequences of stopping the medication before completing the prescribed dosage; a relapse would be inevitable.
Discussion
Lumbar swelling is an abnormal protrusion that may occur around the lumbar spine, which includes the L1-L5 vertebrae [1]. This can be related to infection, haematoma, tumour, disc herniation, cyst, or soft-tissue lesion, which might present with localised pain, tenderness, or limited range of motion [1]. An oval, heterogeneously hypoechoic collection with internal echogenicity of fat lobules is an X-ray finding of an oval-shaped mass that is darker (hypoechoic) compared to the surrounding tissue; it has less dense material [2].
A lumbar hernia with fat necrosis is a condition where tissue (which may include fat) protrudes through a weakened area in the lower back (lumbar region), related to the muscular and fascial floor of the abdominal wall [3]. A tuberculous abscess is a localised collection of pus due to an infection with MTB, commonly known as TB. These abscesses may occur if TB bacteria extend beyond the lungs and affect other tissues, which is common in extrapulmonary TB, including lymph nodes, bones, muscles, or organs [4].
Pott’s spine, or tubercular spondylitis, is a TB condition that predominately affects the vertebrae of the spine. It can only be suspected clinically and then confirmed by imaging of the spine {Magnetic Resonance Imaging (MRI) or Computed Tomography (CT)} and microbiological examination; its treatment traditionally involves anti-TB therapy [5]. This condition occurs when MTB extends to the spine, typically affecting the vertebral column near the intervertebral disc, causing destruction of the bone and the surrounding soft tissues. Pott’s spine may lead to severe lower back pain, spinal deformities such as kyphosis or “hunchback,” and in worse cases, may result in neurological problems, including spinal nerve complications like weakness or even complete paralysis due to spinal stenosis [6,7].
Extrapulmonary TB accounts for approximately 15-20% of all TB patients and musculoskeletal involvement particularly affects the spine [1,2]. Tuberculous abscesses are common in high-burden TB countries, including India, sub-Saharan Africa and Southeast Asia. Patients often experience complications such as spinal deformity, neurological dysfunction and unbearable pain [1,6]. In developed countries, the incidence is considerably lower due to better healthcare access and TB control; however, the illness can still manifest, particularly in patients with immunocompromised status, including those with Human Immunodeficiency Virus (HIV)/Acquired Immunodeficiency Syndrome (AIDS), diabetes and other immunosuppressive diseases [5,6].
Soft-tissue tumours like liposarcomas or myxomas should always be considered because these are painless, gradually growing masses that should be biopsied to determine histological variations [2,3]. Similarly, abscesses may be confused with epidermoid or dermoid cysts, but the differences can be discerned through imaging and histopathological examination [2]. Other notable differentials include hydatid cysts, where serological examinations along with imaging studies reveal the classic feature of daughter cysts and vascular lesions like lymphangiomas or hemangiomas, where Doppler and MRI studies play a crucial role [4,5].
A case involving a 77-year-old male patient, as described by Panigrahi S et al., with a history of diabetes, chronic renal disease on haemodialysis and previous surgery for right lung carcinoma, presented to the outpatient department with acute low back pain and generalised weakness [8]. On physical examination, mild tenderness at the L5 vertebra was noted. An MRI of the lumbosacral spine revealed an epidural abscess at the L4-5 level causing spinal compression [8]. The patient underwent surgery and a laminectomy with abscess drainage was performed [8]. Microscopic examination of the pus revealed budding yeast cells and cultures confirmed the presence of Candida tropicalis [8]. The patient was treated with intravenous amphotericin B followed by oral fluconazole [8].
In a case discussed by Singh J et al., a 30-year-old male with a cervical abscess secondary to Pott’s disease, which is a form of extrapulmonary TB affecting the spine, was treated [9]. The histopathological findings following surgery confirmed a tubercular aetiology and after surgical decompression and anti-tuberculous treatment, the patient demonstrated marked improvement in his condition [9]. The present case highlights the serious nature of spinal abscesses in the context of Pott’s disease, emphasising the risk of neurological impairment if not addressed promptly [9].
In a case described by Özdoğan S et al., a 59-year-old female with a history of significant back pain and recurrent spinal surgeries ultimately presented with spondylodiscitis, evidenced by MRI findings of abscess formation in the lumbar disc [10]. The presence of inflammatory markers, alongside the surgical findings of an abscess, indicated an ongoing infection necessitating the use of antibiotics, including vancomycin [10]. In a case reported by Hurtado Caballero E et al., a 29-year-old female patient from India presented with a retroperitoneal abscess secondary to tuberculous spondylodiscitis [11]. She was initially misdiagnosed with an incarcerated inguinal hernia based on clinical and ultrasound findings [11]. Postoperative imaging demonstrated bilateral retroperitoneal abscesses associated with osteolysis of the lumbar spine, suggestive of tuberculous involvement, which necessitated broad-spectrum antibiotics and anti-TB therapy [11].
The case reported by Pandita A et al., describes a 26-year-old Indian female diagnosed with spinal TB after a prolonged diagnostic journey that included symptoms of back pain and radicular symptoms, ultimately leading to the discovery of a Schmorl’s node associated with MTB infection [12]. The prolonged time to diagnosis, marked by initial treatments for presumed mechanical back pain and inflammatory arthropathy, exemplifies the challenge of recognising spinal TB, particularly in a patient with recent immigration from an endemic region [12].
A 25-year-old Indian male reported by Meena S et al., presented with abdominal pain, weight loss and subsequent back pain, which were suggestive of Pott’s spine, based on MRI findings that revealed perivertebral collection and radiographic signs in favour of TB [13]. Although several conservative measures were applied, the patient had a favourable response to ATT and all imaging studies revealed complete resolution of the abscess [13].
These cases call attention to the necessity of a thorough diagnostic work-up in instances of atypical symptoms and the role of an appropriate surgical approach in managing TB-associated abscesses [13]. A comparative table summarising similar cases from the literature is presented in [Table/Fig-7] [8-13].
Similar cases from the literature [8-13].
| Case | Age (years)/Gender | Presentation | Investigations | Diagnosis | Management | Outcome |
|---|
| Panigrahi S et al., [8], 2023 | 77/Male | Acute low back pain, limp, mild tenderness at L5 | Elevated WBC, CRP, ESR; MRI: epidural abscess | Candida epidural abscess | Laminectomy, abscess drainage, i.v. amphotericin B, oral fluconazole | Smooth recovery, no postoperative issues |
| Singh J et al., [9], 2023 | 30/Male | Cervical abscess, neurological deficits, cord compression | MRI: peripherally enhancing collection | Cervical Pott’s disease | Anterior cervical discectomy, fusion, ATT | Significant neurological improvement |
| Özdoğan S et al., [10], 2018 | 59/Female | Back pain, recurrent surgeries, night sweats | MRI: abscess formation, elevated CRP and ESR | Tuberculous spondylodiscitis | Surgical debridement, anti-TB therapy | Recovery following necrotic tissue removal |
| Hurtado Caballero E et al., [11], 2015 | 29/Female | Retroperitoneal swelling, initially misdiagnosed as hernia | Imaging: abscess without hernia; osteolysis | Retroperitoneal abscess (TB-related) | Abscess drainage, broad-spectrum antibiotics, ATT | Successful resolution of abscess and TB |
| Pandita A et al., [12], 2017 | 26/Female | Back pain, radicular symptoms, neurological deficits | MRI: schmorl node, epidural abscess | Spinal TB (Pott’s disease) | Adjusted ATT regimen; surgical intervention declined | Neurological improvement with tailored ATT regimen |
| Meena S et al., [13], 2014 | 25/Male | Abdominal pain, weight loss, back pain | MRI: perivertebral collection, radiographs | Pott’s spine | ATT | Complete resolution of abscess |
| Current case | 53/Male | Lumbar swelling, no systemic symptoms | Sonography: encapsulated abscess; biopsy: caseous necrosis | Tuberculous abscess | Abscess drainage, ATT | Symptoms resolved, no relapse after 1 year follow-up |
WBC: White blood cell; ESR: Erythrocyte sedimentation rate; CRP: C-reactive protein
Conclusion(s)
The present case emphasises the difficult diagnostic scenario and the increased challenges when generalised lumbar swellings are encountered in clinical practice. In such cases, one should consider an infectious process such as a tuberculous abscess or Pott’s spine, particularly in regions where tuberculosis is endemic. The initial histopathological assessment is essential for diagnosis and effective treatment. The present case highlights the importance of an early start on ATT to avoid adverse effects and enhance prognosis. Improving knowledge and subsequent exploration of the complexity of the clinical spectrum of tuberculosis, particularly in low-resource settings, is crucial for the development of more effective diagnostic strategies and better management of patients.
WBC: White blood cell; ESR: Erythrocyte sedimentation rate; CRP: C-reactive protein
[1]. Zhang AS, Xu A, Ansari K, Hardacker K, Anderson G, Alsoof D, Lumbar disc herniation: Diagnosis and managementAm J Med 2023 136(7):645-51.10.1016/j.amjmed.2023.03.02437072094 [Google Scholar] [CrossRef] [PubMed]
[2]. Yildiz S, Aralasmak A, Kadioglu H, Toprak H, Yetis H, Gucin Z, Radiologic findings of idiopathic granulomatous mastitisMed Ultrason 2015 17(1):39-44.10.11152/mu.2013.2066.171.rfm25745656 [Google Scholar] [CrossRef] [PubMed]
[3]. Goubert D, Oosterwijck JV, Meeus M, Danneels L, Structural changes of lumbar muscles in non-specific low back pain: A systematic reviewPain Physician 2016 19(7):E985-1000.10.36076/ppj/2016.19.E985 [Google Scholar] [CrossRef]
[4]. Khanna K, Sabharwal S, Spinal tuberculosis: A comprehensive review for the modern spine surgeonSpine J 2019 19(11):1858-70.10.1016/j.spinee.2019.05.00231102727 [Google Scholar] [CrossRef] [PubMed]
[5]. Kumaran SP, Thippeswamy PB, Reddy BN, Neelakantan S, Viswamitra S, An institutional review of tuberculosis spine mimics on MR imaging: Cases of mistaken identityNeurol India 2019 67(6):1408-18.10.4103/0028-3886.27363031857525 [Google Scholar] [CrossRef] [PubMed]
[6]. Zhang Y, Yu YS, Tang ZH, Zang GQ, Pott’s kyphosisQJM Mon J Assoc Physicians 2015 108(6):50710.1093/qjmed/hcu22925413798 [Google Scholar] [CrossRef] [PubMed]
[7]. Ansari S, Amanullah MF, Ahmad K, Rauniyar RK, Pott’s spine: Diagnostic imaging modalities and technology advancementsNorth Am J Med Sci 2013 5(7):404-11.10.4103/1947-2714.11577524020048PMC3759066 [Google Scholar] [CrossRef] [PubMed]
[8]. Panigrahi S, Acharya A, Otta S, Puppala S, Spinal fungal abscess mimicking as Pott’s spineInt J Mycobacteriol 2023 12(3):364-66.10.4103/ijmy.ijmy_115_2337721246 [Google Scholar] [CrossRef] [PubMed]
[9]. Singh J, Gupta P, Singh A, Singh A, Atypical cervical Pott’s spine with multiple level epidural collection: A case series of three patientsJ Orthop Case Rep 2023 13(10):115-20.10.13107/jocr.2023.v13.i10.395837885646PMC10599390 [Google Scholar] [CrossRef] [PubMed]
[10]. Özdoğan S, Yaltırık CK, Düzkalır AH, Demirel N, Kaya M, Atalay B, Spinal tuberculosis mimicking failed back surgeryAm J Case Rep 2018 19:249-53.10.12659/AJCR.90740929507280PMC5850844 [Google Scholar] [CrossRef] [PubMed]
[11]. Hurtado Caballero E, Mercader Cidoncha E, Ruiz de la Hermosa A, Amunategui Prats I, Maldonado Valdivieso P, Muñoz-Calero Peregrín A, Absceso retroperitoneal secundario a espondilodiscitis tuberculosa simulando una hernia inguinal incarceradaActa Gastroenterol Latinoam 2015 45(4):316-9.Spanish28590102 [Google Scholar] [PubMed]
[12]. Pandita A, Madhuripan N, Hurtado RM, Dhamoon A, Back pain and oedematous Schmorl node: A diagnostic dilemmaBMJ Case Rep 2017 2017:bcr201721990410.1136/bcr-2017-21990428536227PMC5753748 [Google Scholar] [CrossRef] [PubMed]
[13]. Meena S, Barwar N, Gupta T, Chowdhury B, Spinal tuberculosis presenting as abdominal pain: Rare presentation of a common diseaseOman Med J [Internet] 2014 29(2)[cited 2025 Jan 3]. Available from: http://www.omjournal.org/fultext_PDF.aspx?DetailsID=513&type=fultext10.5001/omj.2014.4030838098PMC6389666 [Google Scholar] [CrossRef] [PubMed]