Cutaneous Metastasis of Squamous Cell Carcinoma of the Tongue as Bilateral Neck Nodules: A Case Report
Sheeja Sainulabdeen1, CK Anju2, Suraj Madhavan Nair3, TV Murali4
1 Professor, Department of Pathology, Government Medical College, Kottayam, Kerala, India.
2 Assistant Professor, Department of Pathology, Government Medical College, Kottayam, Kerala, India.
3 Junior Resident, Department of Gastroenterology, Bharath Hospital, Kottayam, Kerala, India.
4 Assistant Professor, Department of Surgical Oncology, Government Medical College, Kottayam, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Suraj Madhavan Nair, Lakshminivas, Kottayam-686532, Kerala, India.
E-mail: surajmadhu50@gmail.com
Squamous Cell Carcinoma (SCC) of the oral cavity is one of the most common malignancies in the head and neck region. Although lymphatic spread is the most common mode of metastasis, it can also metastasise via the haematogenous route to internal organs such as the lungs, liver and bones. While cutaneous metastasis has been reported in SCC of the oral cavity, metastasis presenting as subcutaneous nodules on both sides of the neck is extremely uncommon. Hereby, authors present a 66-year-old male with a history of smoking and diabetes, diagnosed with well-differentiated SCC of the tongue. He underwent wide local excision, selective neck dissection and adjuvant radiation therapy. He developed a recurrence in the level V cervical lymph nodes after one year, which was surgically excised. Histopathology confirmed metastasis in all the nodes, with two showing extranodal extension. A few weeks later, patient presented with painful, umbilicated skin nodules on both sides of the neck. A biopsy confirmed these as cutaneous metastasis from SCC. This case details a unique presentation of SCC of the tongue, which relapsed as painful subcutaneous nodules on both sides of the neck, highlighting the varied clinical presentation, diagnostic approach and pathological findings.
Metastasise, Ulceroproliferative, Umbilicated nodules
Case Report
A 66-year-old male patient, known to be diabetic and a former smoker, presented with an ulceroproliferative lesion measuring 2.2×1.5×0.7 cm on the anterior two-thirds of the tongue at the left lateral border. A biopsy confirmed a tissue diagnosis of well-differentiated SCC. A clinicoradiological stage of cT2N0M0 was confirmed with a metastatic work-up. As per the multidisciplinary tumour board’s decision, he underwent wide local excision with primary closure and selective neck dissection of the same side, levels I-IV. Histopathology confirmed the diagnosis of SCC (grade 1). All resected margins were free of neoplasm, but perineural and lymphovascular invasions were present. One out of 14 dissected lymph nodes showed metastasis. The pathological stage was pT2N1Mx. Adjuvant radiation of 60 Gy in 30 fractions was administered for the primary site and neck.
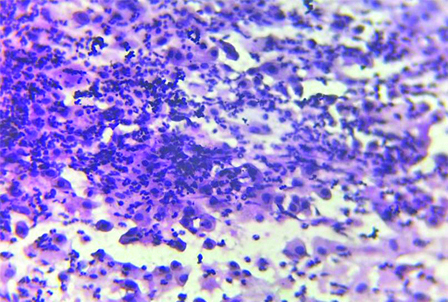
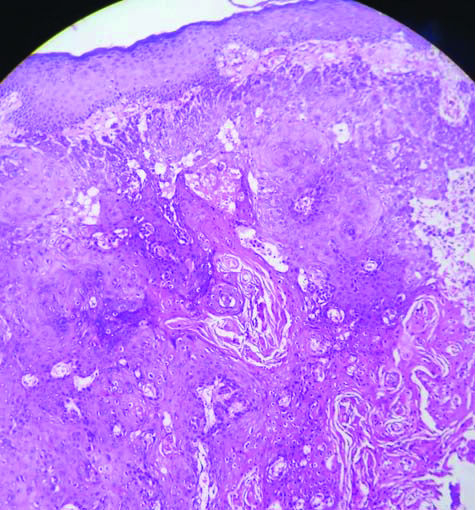
After a year of disease-free interval, he presented with enlarged left level V cervical neck nodes. An Fluorodeoxyglucose Positron Emission Tomography Contrast-enhanced Computed Tomography (FDG PET CECT) scan revealed this as the only site of disease; hence, he underwent completion radical neck dissection and was found to have infiltration of the sternocleidomastoid muscle, internal jugular vein, spinal accessory nerve, and surrounding muscles by the neck nodal mass. Histopathological review confirmed an SCC recurrence with extranodal extension. After four weeks, he presented with multiple umbilicated and tender skin nodules on the anterior aspect of the neck [Table/Fig-1]. Fine Needle Aspiration Cytology (FNAC) aspirated a light brown fluid of less than 0.5 mL. Smears revealed predominantly atypical squamous cells in a background of suppuration, favoring a diagnosis of SCC [Table/Fig-2]. An incisional biopsy was performed to confirm the diagnosis of SCC and to exclude the possibility of other primary cutaneous or appendage tumours and keratoacanthoma. Microscopy confirmed infiltrating SCC [Table/Fig-3]. He was started on palliative chemotherapy; however, the patient developed many similar nodules on the anterior and lateral sides of the neck [Table/Fig-4]. His general condition continues to deteriorate.
Umbilicated nodules on either side of neck.

FNAC from the nodules showing atypical squamous cells with suppuration (Pap stain, 400x).
Skin with an infiltrating neoplasm composed of polygonal cells and areas of keratin pearls (H&E,100x).
Evolving new lesions on the neck.

Discussion
Oral cavity cancer, which includes carcinoma of the tongue, floor of the mouth, gums and lips, is the most common cancer in the head and neck region [1]. SCC is the most common histological variant. Direct extension and invasion of adjacent structures (80-90%) and lymphatic spread (50-70%) are the common modes of spread for this tumour. In advanced cases of SCC, haematogenous dissemination occurs, with common sites being the lungs, liver, bones, brain, kidneys, adrenal glands, pancreas and skin, in decreasing order of frequency [2]. Metastatic subcutaneous nodules are reported in approximately 2-5% of cases of SCC of the tongue [3]. The present patient presented with multiple dome-shaped skin nodules in the neck after a span of one year following the diagnosis and treatment. Fine Needle Aspiration Cytology (FNAC) and biopsy from the nodules confirmed metastatic deposits. Radiological evaluation excluded other metastatic foci.
Cutaneous metastasis is a significant marker of advanced disease and poor prognosis. The morphological spectrum of skin metastases includes asymptomatic papulonodules, erysipeloid, sclerodermoid and zosteriform lesions. Rarely, they may present with a keratoacanthoma-like morphology, as observed in the present case. Keratoacanthoma and SCC have strong clinical and histological similarities. Keratoacanthoma appears as a slowly growing single lesion in sun-exposed areas, is not painful, and can spontaneously resolve [4]. In the present case, the lesions were multiple, painful, and new lesions appeared continuously. Post-irradiation nodules were also listed in the differential diagnosis; however, they can be distinguished by histology.
This unusual form of cutaneous metastasis raised suspicion of Carcinoma Encrasse (CeC) [5]. Differentiating metastatic bilateral nodules from CeC is a diagnostic challenge in most cases. CeC is an abnormal skin metastasis that can present in varying forms, such as nodular, sclerodermatiform, or papular, which develops following radiation or chemotherapy. In contrast, metastatic bilateral nodules are smaller, often less than 2 cm, and are symmetrically distributed on both sides of the neck [5]. The clinicomorphological features favoured the diagnosis of bilateral synchronous metastasis in the present case. CeC is most commonly reported in association with breast and lung carcinoma, with other sites including the colorectum, kidney, ovary, and head and neck.
Lymph node metastasis is a critical prognostic indicator for oral and oropharyngeal carcinomas [6]. The most common site for carcinoma metastasis is the cervical lymph nodes, and this can reduce the survival rate by 50%. Cancer cells usually spread to the lymph nodes on the same side as the primary tumour; however, contralateral or bilateral lymph node metastasis is rare. In histopathology, tumour cell dissemination outside the lymph node capsule worsens the prognosis and reduces patient survival rates.
Early nodal metastasis, multiple lymphovascular emboli, and extranodal extension might have led to an early recurrence in the present case patient, although all the surgical margins were clear. Marked perineural invasion explains the excruciating pain that the patient experienced.
Cutaneous metastasis is associated with a poor prognosis, with an average survival time of less than a year [7]. Treatment for most of these patients is palliative, and although chemotherapy and radiotherapy are often used, they have a limited impact on survival in many cases [8].
Conclusion(s)
The present case highlights the significance of certain unusual patterns of cutaneous metastasis, with CeC being one of them. Any unexplained skin lesion should, therefore, be evaluated carefully and promptly biopsied, as timely diagnosis significantly improves patient prognosis. Awareness of such rare metastatic patterns is crucial for accurate diagnosis, appropriate management and prognosis prediction. Further studies are warranted to understand the mechanisms and clinical implications of cutaneous metastases in SCC.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 03, 2024
Manual Googling: Nov 21, 2024
iThenticate Software: Dec 04, 2024 (5%)
[1]. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countriesCA Cancer J Clin 2021 71(3):209-49.10.3322/caac.2166033538338 [Google Scholar] [CrossRef] [PubMed]
[2]. Tan Y, Wang Z, Xu M, Li B, Huang Z, Qin S, Oral squamous cell carcinomas: State of the field and emerging directionsInt J Oral Sci 2023 15(1):44Available from: https://doi.org/10.1038/s41368-023-00249-w10.1038/s41368-023-00249-w37736748PMC10517027 [Google Scholar] [CrossRef] [PubMed]
[3]. Chaitanya SA, Kumar AA, Dalakoti P, Basude M, Kumar S, Jonathan GT, Dermal metastases in oral cancer after curative treatment: A single institution cohort studyBr J Oral Maxillofac Surg 2021 59(7):814-19.10.1016/j.bjoms.2021.02.02634325947 [Google Scholar] [CrossRef] [PubMed]
[4]. Tisack A, Fotouhi A, Fidai C, Friedman BJ, Ozog D, Veenstra J, A clinical and biological review of keratoacanthomaBr J Dermatol 2021 185(3):487-98.Epub 2021 Jun 1410.1111/bjd.2038933864244 [Google Scholar] [CrossRef] [PubMed]
[5]. Culver AL, Metter DM, Pippen JE Jr, Carcinoma en cuirasseProc (Bayl Univ Med Cent) 2019 32(2):263-65.10.1080/08998280.2018.156496631191149 [Google Scholar] [CrossRef] [PubMed]
[6]. Koyfman SA, Ismaila N, Crook D, D’Cruz A, Rodriguez CP, Sher DJ, Management of the neck in squamous cell carcinoma of the oral cavity and oropharynx: ASCO clinical practice guidelineJ Clin Oncol 2019 37(20):1753-74.Epub 2019 Feb 2710.1200/JCO.18.0192130811281PMC7098829 [Google Scholar] [CrossRef] [PubMed]
[7]. Iancu D, Fulga A, Vesa D, Zenovia A, Fulga I, Sarbu MI, Metastatic patterns and treatment options for head and neck cutaneous squamous cell carcinoma (Review)Mol Clin Oncol 2024 20(6):4010.3892/mco.2024.273938756868PMC11097132 [Google Scholar] [CrossRef] [PubMed]
[8]. Mohamad I, Glaun MDE, Prabhash K, Busheri A, Lai SY, Noronha V, Current Treatment strategies and risk stratification for oral carcinomaAm Soc Clin Oncol Educ Book 2023 43:e38981010.1200/EDBK_38981037200591 [Google Scholar] [CrossRef] [PubMed]