Case Report
A 31-year-old male weighing 50 kg presented with a three-year history of dry cough and progressively worsening difficulty in breathing, which had aggravated in the last month. He was initially diagnosed with interstitial lung disease, for which immunotherapy was given; however, his symptoms persisted with low oxygen levels, leading to his admission to the hospital for further evaluation. His bronchoscopy and PAS stain of Bronchoalveolar Lavage (BAL) confirmed a diagnosis of PAP. A Whole Left Lung lavage (WLL) under general anaesthesia was then planned.
He had no significant history of allergy, asthma, tuberculosis, or chronic lung infections, nor any haematological or immunodeficiency disorders. The patient was conscious, oriented, dyspnoeic and tachypnoeic, with a SpO2 of 82% on room air, improving to 92% with three litres per minute of oxygen. His blood pressure was 118/84 mmHg, heart rate was 98 beats per minute and he was afebrile. He exhibited no pallor, cyanosis, icterus, clubbing, or pedal oedema. Lymph nodes were not palpable and jugular venous pressure was normal. The preprocedural blood test results were noted in [Table/Fig-1].
Preprocedural blood test.
| Test | Results | Normal range |
|---|
| Hb (gm/dL) | 16.5 | 12-15 |
| TLC (/μL) | 8.5×103 | 4-10 |
| DLC (N/L/M/E)% | 75/19/02/04 | 40-60/20-40/2-8/1-4 |
| Platelets (/μL) | 450×103 | 150×103-450×103 |
| ESR (mm/hr) | 28 | less than 15 |
| PT/APTT (secs)/INR | 20.6/12.2/1.01 | 9-14/25-35 |
| CRP (mg/dL) | 0.940 | less than 10 |
| ICTC | Non reactive | |
| HBsAG/HCV | Negative | |
| PCT (ng/mL) | 0.029 | less than 0.05 |
| Glucose (mg/dL) random | 86 | 70-140 |
| Urea/Creatinine (mg/dL) | 7/1.0 | 6-20/0.50-0.90 |
| Na/K/Cl (mmol/dL) | 140/3.46/100.2 | 135-145/3.5-5.5/95-108 |
| TBil/DBil/IBil (mg/dL) | 1.5/0.3/1.2 | upto 1.0/0-0.2/less than 0.8 |
| AST/ALT/ALP (U/L) | 63/22/60 | 10-35/10-35/35-104 |
| TP/Alb/Glob (g/dL) | 7.7/4.4/3.3 | 5.5-8/3.5-5.5/2.0-3.5 |
| A/G | 1.3 | 1-2.2 |
| Serum IL-6 (pg/mL) | 25.04 | less than 5 |
Hb: Haemoglobin; TLC: Total leukocyte count; DLC: Differential leukocyte count; ESR: Erythrocyte sedimentation rate; PT: Prothrombin time; APTT: Activated partial thromboplastin time; CRP: C reactive protein; ICTC: Integrated counselling and testing centres; HBsAg: Hepatitis B surface antigen; HCV: Hepatitis C virus; PCT: Procalcitonin; Na: Sodium; K: Potassium; Cl: Chloride; TBil: Total bilirubin; DBil: Direct bilirubin; IBil: Indirect bilirubin; AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; ALP: Alkaline phosphatase; TP: Total protein; Alb: Albumin; Glob: Globulin; A/G: Albumin-globulin ratio; Serum IL-6: Serum interleukin 6
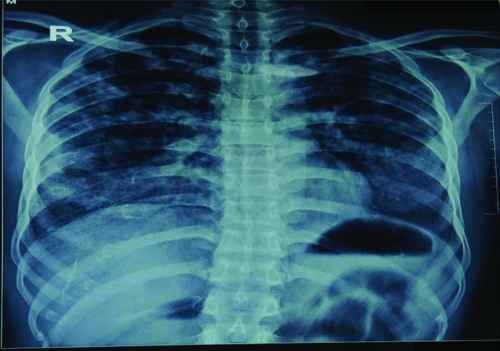
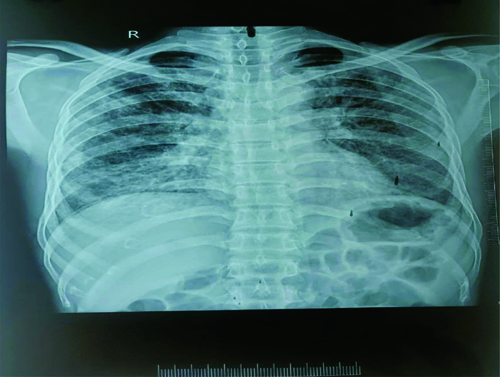
Respiratory examination on auscultation revealed bilateral air entry with fine crackles at the lung bases. A chest X-ray showed multifocal nodular opacities scattered throughout both lungs [Table/Fig-2].
Preprocedural chest X-ray.
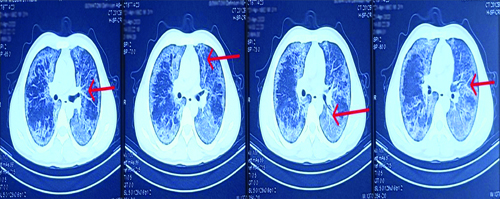
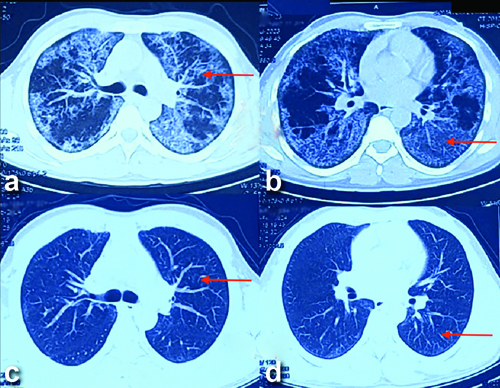
A HRCT thorax was also performed, which revealed a “crazy paving” pattern [1], as indicated in [Table/Fig-3], in the bilateral lung parenchyma, suggestive of PAP. A Pulmonary Function Test (PFT) was advised, which showed Forced Vital Capacity (FVC) at 34%, FEV1/FVC at 100% and Forced Expiratory Volume in one second (FEV1) at 35%, indicating severe restriction and suggesting a non obstructive lung pathology.
Preprocedural HRCT thorax.
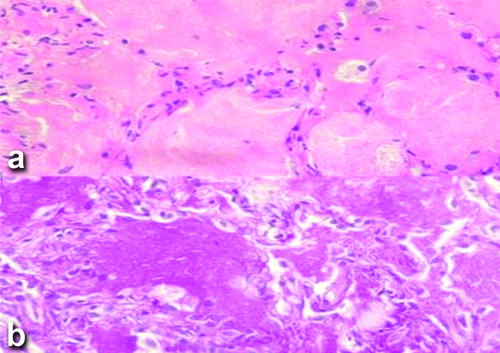
Histopathological examination was carried out, with the results highlighted in [Table/Fig-4], which assisted in the diagnosis of PAP.
a) Histopathological examination-Alveoli consisting of type II pneumocytes containing eosinophilic, amorphous, (H&E,200x); b) Periodic Acid-Schiff (PAS) positive material and occasional alveolar macrophages. (PAS, 200x).
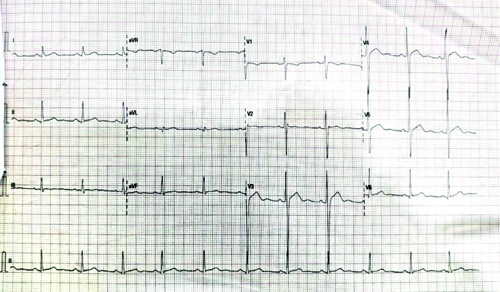
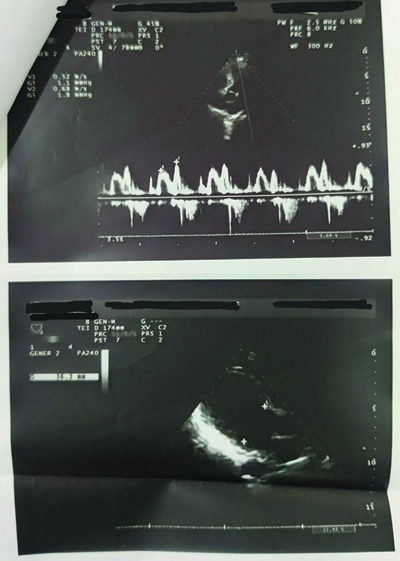
The cardiovascular examination revealed normal S1 and S2 heart sounds, with no abnormal auscultatory findings. The Electrocardiogram (ECG) was unremarkable and 2D echocardiography showed a normal ejection fraction of 60% [Table/Fig-5,6].
ECG showing normal sinus rhythm.
A 2D echocardiography suggests all cardiac chambers are of normal size with normal LV function.
The abdomen was soft, non tender, with audible bowel sounds and the central nervous system exam was normal.
On the day of the procedure, the patient was taken to the operating theatre with an 18G IV cannula in the left hand. American Society of Anaesthesiologists (ASA) II standard monitors were applied and baseline vitals were recorded: BP 125/95 mmHg, HR 100/min and SpO2 100% on five litres of oxygen via a face mask. Under aseptic precautions, the left radial artery was cannulated with a 5 Fr leader catheter and its position was confirmed by visualising the arterial waveform. The patient was preoxygenated with 100% oxygen for 3 minutes. GA was induced using injection fentanyl 100 μg, injection lignocaine 2% 42 mg and injection propofol 100 mg, while muscle relaxation was achieved with injection rocuronium 40 mg. He was intubated with a left-sided DLT of 37 Fr. After confirmation of the proper placement by auscultation, capnography and fibreoptic bronchoscopy, the DLT was fixed at 29 cm; the One-lung Ventilation (OLV) was planned for the left lung as it was more affected than the right side.
The patient was kept on the ventilator with pressure control settings, generating a tidal volume of 7 mL/kg and a Peak End-Expiratory Pressure (PEEP) of 5 cm/H2O. An infusion of injection rocuronium at 0.4 mg/kg/hr was started along with Total Intravenous Anaesthesia (TIVA) using an infusion of injection propofol at 100 μg/kg/min (30 mL/hr) and an infusion of injection fentanyl at 0.1 μg/kg/min (30 μg/hr) for the maintenance of anaesthesia. Under the ultrasound guidance, a central venous line was also secured in the right internal jugular vein for haemodynamic monitoring. A nasal temperature probe was inserted to monitor the core body temperature.
A Y-connector was attached to the circuit for the lavage procedure, with one limb connected to the irrigation fluid and the other for drainage. A fluid warmer was used to assist with the douching of the left lung [Table/Fig-7]. The procedure was performed in the supine position, with a tidal volume of 5 mL/kg and PEEP of 5 cm/H2O. During irrigation, the outflow tubing was clamped and the patient was positioned in Trendelenburg with a slight left lateral tilt. For drainage, the inflow was clamped and the outflow was opened to allow fluid to drain by gravity, aided by regular left chest percussion.
DLT placement and positioning.

On serial Arterial Blood Gases (ABG) workup, there was a definite increase in the partial pressure of oxygen (PaO2) and the Arterial-alveolar (A-a) gradient from the time of admission, during induction and during OLV [Table/Fig-8].
ABG readings through the procedure.
| Parameters | Room air on admission | During induction | During the OLV | Normal range |
|---|
| Fio2 | 21% | 100% | 100% | |
| pH | 7.46 | 7.342 | 7.31 | 7.35-7.45 |
| pCO2 (mmHg) | 34 | 41.2 | 44.5 | 35-45 |
| pO2 (mmHg) | 54 | 210 | 116 | 83-108 |
| HCO3 (mmol/L) | 24.2 | 21.7 | 21.2 | 22-26 |
| SO2 (%) | 89 | 99 | 97.7 | greater than 95 |
| A-a (mmHg) | 53 | 336.5 | 427.3 | 5-10 |
FiO2: Fraction of inspired oxygen; pCO2: Partial pressure of carbon dioxide; pO2: Partial pressure of oxygen; HCO3: Bicarbonate; sO2: Oxygen saturation; A-a- Arterial alveolar gradient
The left lung was lavaged with eight litres of normal saline and seven litres were aspirated until clear. The initial aspirate was milky white with thick sediments [Table/Fig-9]. Intraoperatively, 20 mg of furosemide and 100 mg of hydrocortisone were administered. After the procedure, the DLT was replaced with a cuffed single-lumen tube and manual recruitment was performed to prevent atelectasis. The post procedural A-a gradient improved from 53 to 29 mmHg.
Milky white lavaged fluid serially numbered showing progressive clearing.

The patient was moved to the ICU and the follow-up chest X-ray demonstrated improvement, with a reduction in the previously noted scattered nodular opacities [Table/Fig-10]. The patient was extubated after 24 hours and observed for 36 hours before discharge. He returned to the hospital 10 days later with fever and loss of appetite. His vitals were BP 132/100 mmHg, HR 96/min and a SpO2 98% on room air. He was treated with injection Meropenem one gram twice daily and injection Clindamycin 600 mg twice daily and was discharged after seven days.
Postprocedural chest X-ray.
The patient was regularly followed-up and reported no new complaints. Six months postprocedure, an HRCT thorax showed no new changes in the left lung and also no evidence of a crazy paving pattern in the right lung, as shown in [Table/Fig-11].
Axial CT scan: a,b) Preprocedural HRCT scan depicting the “crazy paving” pattern, left side affected more than right. c,d) Done six months after the procedure showing improvement in the lung parenchyma.
Discussion
The PAP is a rare disorder caused by the accumulation of lipid-rich surfactants in the alveoli, leading to impaired gas exchange. It results from disrupted Granulocyte-Macrophage Colony-Stimulating Factor (GM-CSF) signalling, reduced alveolar macrophage function, or abnormal surfactant production. PAP is classified into three types: primary (autoimmune [2] or hereditary), secondary (due to conditions like haematological disorders, dust inhalation, or chronic infections) and congenital (due to mutations in surfactant proteins). Symptoms include shortness of breath, cough and sputum, with fever and haemoptysis occurring in secondary infections. Diagnosis involves clinical symptoms, radiology and BAL, which typically has a characteristic milky appearance. Treatment involves sequential WLL, which removes excess surfactant [3]. GM-CSF therapy has also been explored to enhance macrophage function [4]. WLL utilises aliquots of 500-1,000 mL of warm saline at 37° Celsius to irrigate the affected lung, followed by drainage, while balanced anaesthesia using TIVA and a muscle relaxant maintains lung function. Challenges include airway trauma, tube dislodgement, oxygenation issues and the risk of hypoxaemia, atelectasis, hypothermia and pneumonia [5]. After WLL, the double-lumen tube is replaced with a single-lumen tube to restore ventilation and careful monitoring is essential to avoid complications.
In the present case, the patient presented with shortness of breath and continuously low saturation, with no other co-morbidities. After the available tests were completed, a diagnosis of PAP was made and the procedure of WLL was planned. In the studies conducted by Pandit A et al., and by Tan Z et al., an additional test of transbronchial biopsy was performed to enhance the diagnosis of PAP [6,7]. Additionally, the anti-GM-CSF antibody titre was measured in the study by Pandit A et al., which further reinforced the classification of the case as primary PAP [6].
In the present case, patient was preoxygenated with 100% oxygen before the induction process, whereas Pradhan R et al., utilised Continuous Positive Airway Pressure (CPAP) at 10 cm H2O for 5 minutes in a propped-up position, along with 100% oxygen, to help maintain saturation during induction [8]. Since the left lung was affected more than the right, the intervention was planned only for the left lung in the first setting using a 37Fr DLT whereas in the first case carried out by Tan Z et al., an Arndt endobronchial blocker was placed using the loop technique, alongside a 35Fr left-sided DLT [7]. A fiberoptic bronchoscope was inserted through the bronchial lumen into the distal loop of the endobronchial blocker. The blocker was then manoeuvred to selectively isolate the posterior and lateral segments of the left lower lobe. The bronchial lumen was subsequently advanced into the left main bronchus for lung isolation.
A total of 8 liters of normal saline, administered in aliquots, was used for irrigation. The procedure was conducted in the supine position, with low tidal volume and a PEEP of 5 cm H2O. During irrigation, the patient was positioned in Trendelenburg with a slight left lateral tilt. Drainage involved clamping inflow and opening outflow tubing, supported by chest percussions. Gaiwal S et al., also kept their patient in the Trendelenburg position during the inflow and in a reverse Trendelenburg position during the outflow. Right and left tilts were also performed to ensure uniform distribution of fluids across the different parts of the irrigated lungs [9]. Index patient remained well-oxygenated throughout, with no haemodynamic instability observed intraoperatively.
In the case reported by Manohar M and Bansal P [10], during the left lung lavage procedure, the patient experienced episodes of desaturation. Double-lung ventilation was temporarily resumed and lung recruitment was performed at the end of the procedure. The lavage of the right lung was conducted the following day after the patient had been stabilised. In the study performed by Tan Z et al., [7], the first cycle lavage of the right lung resulted in decreased oxygen saturation. To address this, the patient was placed on 100% oxygen and manually ventilated to restore saturation. Additionally, the patient was positioned in the left lateral decubitus position and CPAP ventilation was applied to the non ventilated lung between lavage cycles to improve SpO2 levels. The lavage of the left lung was performed one month later.
In the case conducted by Das PK et al., the left lung was lavaged first, during which the patient experienced multiple episodes of desaturation accompanied by haemodynamic instability. Vasopressors such as noradrenaline infusion at 0.05 μg/kg/min and dobutamine infusion at 3 μg/kg/min were initiated to maintain vital signs. Furthermore, fluid leakage into the lungs was suspected due to an increase in airway pressures accompanied by a decrease in tidal volume. The team promptly responded by employing a fibreoptic bronchoscope and performing suction, which led to an improvement in saturation levels shortly afterward [11].
Postprocedure, present case patient was shifted to the ICU and extubated after 24 hours, being discharged on the third day. In contrast, in the case studied by Varun R et al., [12], the patient was extubated after 48 hours onto a CPAP mask and was gradually weaned off over two days to nasal oxygen, being sent to the ward with 2 L/min of oxygen. This patient was discharged on the sixth postoperative day.
During the regular follow-up of the index patient, a repeat HRCT thorax revealed no opacities in either lung. This finding suggests the possibility of spontaneous regression in the previously affected right lung. The similar studies mentioned provide access to different approaches to the diagnosis and management of PAP.
Most cases of PAP are attributed to the presence of autoimmune antibodies (anti-GM-CSF antibodies). Seth M et al., proposed a treatment strategy beginning with WLL, followed by the continuation of steroids in the postoperative period, with GM-CSF therapy also being considered [13]. However, due to gaps in the availability of testing for these antibodies in different parts of the country, present case was classified as primary idiopathic PAP. Present study also highlights the discussion of spontaneous regression of the disease, as the right lung showed no radiological findings after six months postprocedure on the left lung. This case not only complements the existing literature but also fills critical gaps, particularly in resource-constrained contexts.
Conclusion(s)
The PAP is a rare condition with distinct diagnostic and management challenges, particularly in resource-constrained settings. This case highlights the effective use of clinical presentation, imaging and histopathology for diagnosis in the absence of advanced tests, such as anti-GM-CSF antibody assays. Sequential WLL proved effective, with the unique observation of spontaneous regression in the untreated lung, suggesting the potential for self-resolution in some cases. Present case findings underscore the need for increased awareness, improved diagnostic access and tailored management strategies for PAP, especially in regions with limited healthcare resources.
Hb: Haemoglobin; TLC: Total leukocyte count; DLC: Differential leukocyte count; ESR: Erythrocyte sedimentation rate; PT: Prothrombin time; APTT: Activated partial thromboplastin time; CRP: C reactive protein; ICTC: Integrated counselling and testing centres; HBsAg: Hepatitis B surface antigen; HCV: Hepatitis C virus; PCT: Procalcitonin; Na: Sodium; K: Potassium; Cl: Chloride; TBil: Total bilirubin; DBil: Direct bilirubin; IBil: Indirect bilirubin; AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; ALP: Alkaline phosphatase; TP: Total protein; Alb: Albumin; Glob: Globulin; A/G: Albumin-globulin ratio; Serum IL-6: Serum interleukin 6
FiO
2: Fraction of inspired oxygen; pCO
2: Partial pressure of carbon dioxide; pO
2: Partial pressure of oxygen; HCO
3: Bicarbonate; sO
2: Oxygen saturation; A-a- Arterial alveolar gradient
[1]. Holbert JM, Costello P, Li W, Hoffman RM, Rogers RM, CT features of pulmonary alveolar proteinosisAJR Am J Roentgenol 2001 176(5):1287-94.10.2214/ajr.176.5.176128711312196 [Google Scholar] [CrossRef] [PubMed]
[2]. Inoue Y, Trapnell BC, Tazawa R, Arai T, Takada T, Hizawa N, Japanese Center of the Rare Lung Diseases Consortium. Characteristics of a large cohort of patients with autoimmune pulmonary alveolar proteinosis in JapanAm J Respir Crit Care Med 2008 177(7):752-62.10.1164/rccm.200708-1271OC18202348PMC2720118 [Google Scholar] [CrossRef] [PubMed]
[3]. Cheng SL, Chang HT, Lau HP, Lee LN, Yang PC, Pulmonary alveolar proteinosis: Treatment by bronchofiberscopic lobar lavageChest 2002 122(4):1480-85.10.1378/chest.122.4.148012377884 [Google Scholar] [CrossRef] [PubMed]
[4]. Sheng G, Chen P, Wei Y, Chu J, Cao X, Zhang HL, Better approach for autoimmune pulmonary alveolar proteinosis treatment: Inhaled or subcutaneous granulocyte-macrophage colony-stimulating factor: A meta-analysesRespir Res 2018 19(1):16310.1186/s12931-018-0862-430165864PMC6117963 [Google Scholar] [CrossRef] [PubMed]
[5]. Awab A, Khan MS, Youness HA, Whole lung lavage-technical details, challenges and management of complicationsJ Thorac Dis 2017 9(6):1697-1706.10.21037/jtd.2017.04.1028740686PMC5506114 [Google Scholar] [CrossRef] [PubMed]
[6]. Pandit A, Gupta N, Madan K, Bharti SJ, Kumar V, Anaesthetic considerations for whole lung lavage for pulmonary alveolar proteinosisGhana Med J 2019 53(3):248-51.10.4314/gmj.v53i3.931741497PMC6842735 [Google Scholar] [CrossRef] [PubMed]
[7]. Tan Z, Tan KT, Poopalalingam R, Anesthetic management for whole lung lavage in patients with pulmonary alveolar proteinosisA A Case Rep 2016 6(8):234-47.10.1213/XAA.000000000000028326795910 [Google Scholar] [CrossRef] [PubMed]
[8]. Pradhan R, Shrestha RR, Bhusal S, Anaesthetic management for whole lunglavage in pulmonary alveolar proteinosis: A case reportPMJN 2023 23((1):65-67.10.56974/pmjn.133 [Google Scholar] [CrossRef]
[9]. Gaiwal S, Sarvesh SPSA, Prasad N, Anesthetic management of broncho- alveolar lavage in pulmonary alveolar proteinosis: A case reportIndian J Clin Anaesth 2024 11(2):251-54.10.18231/j.ijca.2024.047 [Google Scholar] [CrossRef]
[10]. Manohar M, Bansal P, Whole lung lavage in pulmonary alveolar proteinosis: Anesthetic management and challengesAin-Shams J Anesthesiol 2022 14:1510.1186/s42077-022-00213-6 [Google Scholar] [CrossRef]
[11]. Das PK, Yadavilli KP, Correction: Anesthetic challenges during whole lung lavage: A case reportCureus 2023 15(2):c10210.7759/cureus.c102 [Google Scholar] [CrossRef]
[12]. Varun R, Dhammika KAP, Jayathilaka R, Pakeerathan S, Anaesthetic management of whole lung lavage in a resource-limited setting: Case reportSri Lankan Journal of Anaesthesiology 2024 32(1):85-90.10.4038/slja.v31i2.9119 [Google Scholar] [CrossRef]
[13]. Seth M, Kachru N, Kohli S, Balakrishnan I, Chauhan R, Kumar R, Anesthetic management of a case of pulmonary alveolar proteinosis for whole lung lavageThe Egyptian Journal of Chest Diseases and Tuberculosis 2023 72(4):579-83.10.4103/ecdt.ecdt_48_23 [Google Scholar] [CrossRef]