Most people in the world commonly experience renal stone disease, with prevalence gradually increasing. The lifetime risk of the disease observed in men is 12%, while in women, it is 7% [1,2]. Various factors impact the management of renal stone disease, such as the size of the calculus and its location. Before the endoscopy era, open surgical procedures were the only treatments available for renal calculi. Now, with newly developed technologies such as RIRS, ESWL, Percutaneous Nephrolithotomy (PCNL), and Endoscopic Combined Intra Renal Surgery (ECIRS), the management of stones has changed drastically [3]. ESWL emerged in the 1980s, offering a non invasive method to tackle renal calculi through the application of shock waves to the stones [4]. RIRS, on the other hand, provides better and more direct vision to fragment stones within the pelvicalyceal system using a flexible scope [5]. Literature mentions that similar studies have been performed in the past, but results were inconsistent, and there is still debate over which modality excels over the other [6,7].
Stone clearance varies between the two treatment modalities. ESWL, being a non invasive treatment, is influenced by various stone and patient factors, such as habitus [8]. Meanwhile, RIRS has better vision and direct accessibility to the calculus, which is responsible for greater stone clearance; however, it is an invasive procedure with anaesthesia risks and other complications [9].
Present study analysed and compared patient-related factors, including the safety and efficacy of ESWL and RIRS for the treatment of single kidney stones ranging from 10 to 20 mm in size. With evidence from the available literature, this study aimed to guide urologists and other healthcare professionals in providing better treatment options for patients.
Materials and Methods
A prospective interventional study was conducted in the Department of Urology at Dr. D. Y. Patil Medical College, Hospital and Research Centre, Pimpri, Pune, Maharashtra, India, from October 2022 to October 2024. Appropriate ethical committee approval was obtained (IESC/233/2022). All patients were included after providing written informed consent.
Inclusion criteria: Patients aged between 18 and 60 years with a single renal calculus measuring between 10 mm and 20 mm, proven by investigations such as Computed Tomography Kidneys, Ureters and Bladder (CT KUB) (plain or contrast), were included in the study. Patients underwent stenting for a minimum of three weeks before RIRS or ESWL.
Exclusion criteria:
Patients unwilling to participate in the study;
Age <18 years or >60 years;
Active urinary tract infection;
Ureteropelvic junction obstruction or other abnormal anatomy;
Pregnancy;
Bleeding disorders;
Patients on anticoagulants;
Patients with chronic kidney disease;
Obese patients;
Patients with co-morbid conditions;
Solitary kidney;
Urinary tract cancer;
Radiolucent calculus;
Calyceal diverticulum.
Considering the stone-free rates following ESWL and RIRS, which were 68% and 90.4%, respectively, from a study by Javanmard B et al., with a power of 80%, the sample size was calculated to be 20 patients in each group [10]. Simple randomisation was conducted using computerised random numbers. All necessary investigations, both pre- and postprocedure, were performed, and data was collected.
Group A: RIRS: N=20
Group B: ESWL: N=20
Basic history and examination were performed on each patient. Routine blood investigations and radiological investigations, such as X-ray KUB, USG KUB, and CT KUB, were obtained.
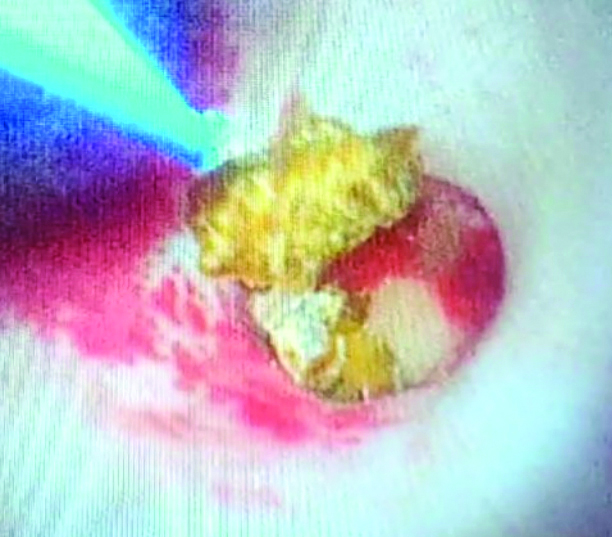
Group A: RIRS: Initially, patients in group A underwent stenting with a 5 Fr stent prior to RIRS. Using a flexible ureteroscope, RIRS was performed, and a ureteral access sheath was utilised. A Quanta 60 W holmium laser was used for lithotripsy [Table/Fig-1]. The laser power was set between 0.5 and 1 J, and the frequency used was between 20 and 40 Hz. After surgery, a 5 Fr Double-J stent was placed. The procedure could be immediately converted to a PCNL procedure with prior consent if incomplete stone clearance was observed. The removal of the Double-J stent was performed three weeks after the procedure.
Stone getting dusted with LASER.
Group B: ESWL: In group B, prestenting of all patients was done with a 5 Fr DJ stent. ESWL was performed using the Dornier Compact Sigma on patients as an outpatient procedure. Initially, an oral tablet of Diclofenac was given along with local anaesthesia in the form of lignocaine jelly at the site of the shock wave entrance. The shock wave was initially started at a rate of 60 impulses per minute, which was gradually increased to 100 pulses per minute depending on the patient’s tolerability. The maximum number of shocks given per session was 3000. Postprocedural discomfort, lithuria, and complications were explained to the patients. After one week of each session, X-ray KUB and USG KUB were used to check for clearance. Second and third sessions of ESWL were administered if required, with a maximum of three sessions offered to any patient. After one week following the third session of ESWL, radiological investigations such as USG KUB and X-ray KUB were performed to assess for residual calculus. In cases of incomplete stone clearance, the patient was admitted for further treatment. Any residual calculus of <4 mm in size or the absence of stones was considered complete stone clearance.
Various variables, including the duration of the procedure, complications, stone clearance, hospital stay, hospital visits, and the need for ancillary procedures, were compared.
Statistical Analysis
Data analysis was completed using Statistical Package for the Social Sciences (SPSS) software version 20.0. Continuous variables were expressed as means and standard deviations. Proportions and counts were used to express categorical variables. The Chi-square test was used to analyse categorical variables. Statistical significance was considered when the p-value was <0.05.
Results
Better stone clearance was achieved in the RIRS group compared to the ESWL group. The length of hospital stay between the two groups was significantly different, with 10 patients (50%) from the ESWL group not requiring admission. Additionally, 17 patients (85%) in the RIRS group did not require any ancillary procedures, while eight patients from the ESWL group required ancillary procedures. All patients in the RIRS group completed treatment with one hospital visit, whereas 16 patients in the ESWL group required multiple visits [Table/Fig-2,3].
Table comparing data of two groups.
| Parameters | Group-A (RIRS)
n (%) | Group-B (ESWL)
n (%) |
|---|
| Age (years) |
| <20 | 1 (5) | 0 |
| 21-30 | 5 (25) | 3 (15) |
| 31-40 | 6 (30) | 7 (35) |
| 41-50 | 5 (25) | 7 (35) |
| 51-60 | 3 (15) | 3 (15) |
| Chi-square, p-value | 1.91, 0.752 |
| Gender |
| Male | 9 (45) | 10 (50) |
| Female | 11 (55) | 10 (50) |
| Chi-square, p-value | 0.1, 0.752 |
| Size in mm |
| 10-15 | 13 (65) | 12 (60) |
| 16-20 | 7 (35) | 8 (40) |
| Chi-square, p-value | 0.107, 0.744 |
| Location |
| Upper calyx | 3 (15) | 3 (15) |
| Middle calyx | 5 (25) | 9 (45) |
| Lower calyx | 7 (35) | 4 (20) |
| Renal pelvis | 5 (25) | 4 (20) |
| Chi-square, p-value | 2.072, 0.558 |
| Duration in minutes |
| 30-60 | 8 (40) | 4 (20) |
| 60-90 | 9 (45) | 3 (15) |
| 90-120 | 3 (15) | 2 (10) |
| 120-150 | 0 | 2 (10) |
| 150-180 | 0 | 9 (45) |
| Chi-square, p-value | 15.533, 0.004 |
Table comparing complications and other outcomes.
| Parameters | Group-A (RIRS)
n (%) | Group-B (ESWL)
n (%) |
|---|
| Complications* |
| No | 15 (75) | 15 (75) |
| Sepsis | 1 (5) | 0 |
| Pain | 2 (10) | 5 (25) |
| Haematuria | 3 (15) | 4 (20) |
| Fever | 3 (15) | 0 |
| Clearance |
| Complete | 17 (85) | 12 (60) |
| Partial | 3 (15) | 8 (40) |
| Chi-square, p-value | 2.006, 0.156 |
| Days of hospital stay |
| 0 | 0 | 10 (50) |
| 1-2 | 1 (5) | 3 (15) |
| 3-4 | 16 (80) | 7 (35) |
| 5-6 | 2 (10) | 0 |
| 7-8 | 1 (5) | 0 |
| Chi-square, p-value | 11.633, 0.02 |
| Need of ancillary procedure |
| Nil | 17 (85) | 12 (60) |
| Mini PCNL | 0 | 2 (10) |
| PCNL | 3 (15) | 2 (10) |
| RIRS | 0 | 4 (20) |
| Chi-square, p-value | 7.062, 0.07 |
| Number of hospital visits |
| 1 | 20 (100) | 4 (20) |
| 2 | 0 | 5 (25) |
| 3 | 0 | 3 (15) |
| 4 | 0 | 8 (40) |
| Chi-square, p-value | 20.033, 0.00016 |
*multiple responses
Discussion
Multiple factors appear to be causative factors involving complex interactions between genetic, environmental, and dietary elements [11]. Over the decades, with evolving technologies, the management of renal stone disease has shown a significant paradigm shift from open surgical procedures to minimally invasive surgical techniques [3]. Present study indicated a gender distribution with a slight female predominance of 52.5%. In contrast, a study by Dhayal IR et al., reported male predominance at 69.3% [12]. Most stones in this study were in the size range of 10-15 mm (62.5%). Sarikaya S et al., reported similar findings, with a mean stone size of 16.3±7.5 mm in the RIRS group and 11±4 mm in the ESWL group [13].
The stone location distribution in the present study was as follows: upper calyx 15% for both RIRS and ESWL, middle calyx 25% for RIRS and 45% for ESWL, lower calyx 35% for RIRS and 20% for ESWL, and renal pelvis 25% for RIRS and 20% for ESWL. This was compared to Sarikaya S et al.’s study, which showed upper pole involvement at 2.2% in RIRS and 2% in ESWL, middle pole at 43.5% for RIRS and 18.4% for ESWL, lower pole at 34.8% for RIRS and 18.4% for ESWL, and pelvis at 10.9% for RIRS and 20.4% for ESWL [13].
RIRS demonstrated better stone clearance, achieving 85% compared to 60% for ESWL. Present study findings were consistent with those of Dhayal IR et al., in which RIRS showed 85% stone clearance and ESWL recorded 76.7% [12]. Setthawong V et al., noted a lower success rate for ESWL compared to RIRS, with a relative risk of 0.85 (95% CI 0.78 to 0.93) across 13 studies [14].
Various studies have reported differing opinions regarding procedural timings. In present study, 85% of RIRS surgeries were completed within 90 minutes, similar to Dhayal IR et al.’s findings of 51.2 minutes [12]. However, opposing results were reported in studies by Elal AMA et al., [15], where the RIRS procedure duration was 60±12 minutes and that for ESWL was 54±6 minutes [15]. Gyuler Y and Erbin A recorded a shorter time, with a mean of 43.5±12 minutes for the RIRS procedure, while the ESWL procedural time was 74.2±54.2 minutes [16]. Singh BP et al., compared both single-session and total procedural times, reporting a mean operative time for RIRS of 78.7±20.03 minutes, while the single session of ESWL was 42.25±6.34 minutes, and the total sessions of ESWL were 86.0±21.21 minutes [17]. The varying methods used to calculate procedural durations in these studies highlight the need for standardisation in time measurement.
In present study, 50% of ESWL patients did not required hospital admission at all. On the other hand, 80% of patients in the RIRS group required 3 to 4 days of admission. Dhayal IR et al., demonstrated approximately three days of hospitalisation in the RIRS group, while a minimal stay of 0.13 days was observed in the ESWL group [12]. Elal AMA et al., stated a four-hour stay for ESWL versus 30 hours for RIRS [15]. Setthawong V et al., concluded that the hospital stay was shorter for ESWL than for RIRS, with a mean difference of -1.69 days (95% CI -2.36 to -1.02) for ESWL [14].
Present study reported a complication rate of 25% in both groups, which was similar to broader literature, particularly the study by Zhang W et al., which concluded comparable overall complication rates [18]. A detailed Clavien-graded analysis was provided by Singh BP et al., in their study, where nine subjects in the RIRS group had grade one complications, while 13 in the ESWL group had grade one complications [17]. One patient from the RIRS group and two from the ESWL group had grade two complications. Additionally, one patient from the RIRS group and two from the ESWL group had grade three complications. Guler Y and Erbin A stated that Clavien-Dindo Grades 1-2 complications were predominant in both groups (5-23%) [16].
This collective evidence suggests that while overall complication rates may be similar, each procedure carries its distinct risk profile, emphasising the importance of considering patient-specific factors and stone characteristics in treatment selection. In present study, there was one patient with sepsis in the RIRS group. Sepsis is a significant concern in the case of RIRS. Maintaining low intra-pelvicalyceal pressure, ensuring adequate control of infection, and using appropriate antibiotics may reduce the risk of sepsis in RIRS.
The choice between RIRS and ESWL should be made while considering cost, treatment modality efficiency, and available resources [19]. A greater need for ancillary procedures was observed in the ESWL group compared to the RIRS group (40% vs. 15%). Dhayal IR et al., found a significant difference (p-value=0.031) in the need for ancillary procedures, with RIRS requiring 10% of cases and ESWL requiring 18.33% of cases [12]. Setthawong V et al., concluded that there was a greater need for ancillary procedures to achieve treatment goals, with a relative risk of 1.98 (95% CI 1.14 to 3.47) [14].
The strength of this study lies in establishing that both RIRS and ESWL are viable options for managing a single renal calculus of 1 to 2 cm. Based on the observations obtained, it can be concluded that a single renal calculus of 1 to 2 cm can be managed with RIRS, keeping in mind the need for a longer hospital stay but a better stone clearance rate compared to non invasive ESWL.
Limitation(s)
There is no standard technique for calculating the procedure duration for ESWL, which might have some effect on the study.
Conclusion(s)
The RIRS had better stone clearance and fewer ancillary procedures, but it was invasive and required admission with a longer hospital stay. In contrast, ESWL was non invasive and required multiple hospital visits, along with a greater number of ancillary procedures and, in some cases, a longer duration of treatment. The final treatment decision should consider multiple factors, such as patient preference, stone characteristics, and the availability of resources. Therefore, the procedure should be individualised for each patient.
*multiple responses