Stanford Type A Acute Aortic Dissection with Left Coronary Artery Involvement: Computed Tomography Angiography Findings
Nishant Narendra Kumar1, Revathi Rajagopal2, Deepthi Arunkumar3, Senthil Kumar Aiyappan4, Jayaselin Praveena Joseph5
1 Junior Resident, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRM IST, Kattankulathur, Chengalpattu, Tamil Nadu, India.
2 Junior Resident, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRM IST, Kattankulathur, Chengalpattu, Tamil Nadu, India.
3 Junior Resident, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRM IST, Kattankulathur, Chengalpattu, Tamil Nadu, India.
4 Professor and Head, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRM IST, Kattankulathur, Chengalpattu, Tamil Nadu, India.
5 Junior Resident, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRM IST, Kattankulathur, Chengalpattu, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Senthil Kumar Aiyappan, Professor and Head, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRM IST, Kattankulathur, Chengalpattu-603203, Tamil Nadu, India.
E-mail: asenthilkumarpgi@gmail.com
Breath sounds, Chest pain, Pleural effusion, Tachycardia
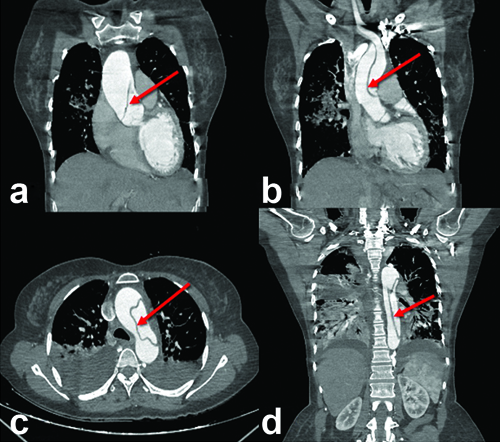
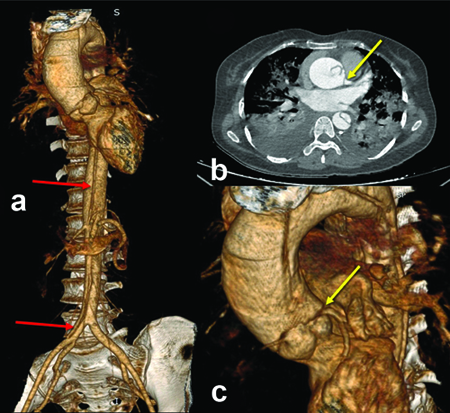
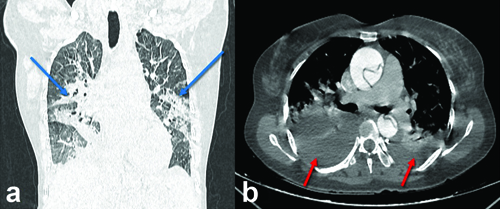
A 48-year-old female presented to the emergency department with complaints of acute onset chest pain radiating to the back and breathlessness for the past 24 hours. The patient reported no significant past medical history but had a family history of hypertension. On examination, her blood pressure was markedly elevated at 200/160 mmHg and she appeared distressed and diaphoretic. Auscultation revealed diminished breath sounds in the left lung base. An Electrocardiogram (ECG) revealed sinus tachycardia. Given the clinical suspicion of aortic dissection, urgent imaging studies were performed. A Computed Tomography Angiography (CTA) of the chest was conducted, revealing a Stanford Type A aortic dissection extending from the ascending aorta to the abdominal aorta. A thin, oblique intimal flap was noted, extending from the aortic root just above the right sinus of Valsalva through the entire course of the ascending aorta, arch of the aorta, descending thoracic aorta and abdominal aorta, up to the common iliac artery [Table/Fig-1a-d]. An extension of the flap transversely into the left sinus of Valsalva, involving the osteoproximal segment of the left main coronary artery, was observed [Table/Fig-2]. Diffuse consolidations involving bilateral perihilar regions of both lung fields suggested pulmonary oedema [Table/Fig-3a]. Bilateral pleural effusions were also noted [Table/Fig-3b]. Despite the immediate initiation of antihypertensive therapy and arrangements for surgical consultation, the patient’s condition rapidly deteriorated. She developed profound hypotension and loss of consciousness within two hours of admission. Despite aggressive resuscitative measures, including fluid resuscitation and vasopressor support, the patient could not be stabilised. Cardiopulmonary resuscitation was initiated, but unfortunately, the patient succumbed to cardiac arrest.
a-d) CT angiography images: A thin, oblique intimal flap was noted extending from the aortic root just above the right sinus of Valsalva, through the entire course of ascending aorta, arch of aorta, descending thoracic aorta and abdominal aorta (red arrows).
a) 3D volume rendered image showing flap extension into the right common iliac artery from abdominal aorta (red arrows); b,c) Extension of the flap into osteoproximal segment of left main coronary artery (yellow arrows).
a,b) CT chest images showing diffuse consolidations involving bilateral perihilar regions of bilateral lung fields suggesting pulmonary oedema (blue arrows) and bilateral pleural effusion (red arrows).
Aortic dissection presents a significant diagnostic and therapeutic challenge due to its potentially fatal consequences [1,2]. It typically manifests with abrupt onset severe chest pain, often described as tearing or ripping, which can radiate to the back. Although in present case, patient presented with classic symptoms, the clinical presentation can vary widely [3,4]. Diagnostic imaging modalities, particularly CTA, are important diagnostic tools that help determine the diagnosis and the extent of the dissection [5].
Aortic dissection with coronary artery involvement is relatively rare. In a study by Saito Y et al., patients with left coronary artery involvement had an augmented risk of death compared to those with right coronary artery involvement (54.3% vs. 31.3%, p-value <0.001) [6]. This finding was similar to present case. Sen G et al., described a case of Stanford type A aortic dissection with intramural haematoma extending into the left main coronary artery and left anterior descending artery, which is comparable to the present case [7]. However, there was no intramural haematoma in the current case and the left anterior descending artery was not involved. Huang LC et al., described a case of Stanford type A acute aortic dissection with right coronary artery involvement; however, in the present case, the left main coronary artery was involved [8].
The prognosis of aortic dissection depends on various factors, including the extent of the dissection, the presence of complications and the timeliness of intervention [7]. Unfortunately, the patient succumbed to the condition within hours of admission due to the extent of the aortic dissection extending into the osteoproximal segment of the left coronary artery. Left coronary artery involvement in aortic dissection is critical due to its role in supplying oxygen-rich blood to a large portion of the myocardium [6]. This involvement can lead to myocardial ischaemia and infarction, posing a significant threat to the patient’s cardiac function and overall prognosis [6].
Involvement of the left coronary artery increases the risk of cardiogenic shock, emphasising the need for prompt diagnosis and aggressive management to prevent life-threatening complications [6]. This case underscores the critical importance of early recognition and management of aortic dissection to prevent catastrophic outcomes. Despite aggressive medical intervention and timely diagnostic imaging, the patient’s condition rapidly deteriorated, highlighting the formidable challenges in treating this condition.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 09, 2025
Manual Googling: Jan 18, 2025
iThenticate Software: Jan 20, 2025 (6%)
[1]. Pape LA, Awais M, Woznicki EM, Suzuki T, Trimarchi S, Evangelista A, Presentation, diagnosis, and outcomes of acute aortic dissection: 17-year trends from the International Registry of Acute Aortic DissectionJ Am Coll Cardiol 2015 66(4):350-58.10.1016/j.jacc.2015.05.02926205591 [Google Scholar] [CrossRef] [PubMed]
[2]. Evangelista A, Isselbacher EM, Bossone E, Gleason TG, Eusanio MD, Sechtem U, Insights from the International Registry of Acute Aortic Dissection: A 20-year experience of collaborative clinical researchCirculation 2018 137(17):1846-60.10.1161/CIRCULATIONAHA.117.03126429685932 [Google Scholar] [CrossRef] [PubMed]
[3]. Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, ESC Committee for Practice Guidelines2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC)Eur Heart J 2014 35(41):2873-926.10.1093/eurheartj/ehu28125173340 [Google Scholar] [CrossRef] [PubMed]
[4]. Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, The International Registry of Acute Aortic Dissection (IRAD): New insights into an old diseaseJAMA 2000 283(7):897-903.10.1001/jama.283.7.89710685714 [Google Scholar] [CrossRef] [PubMed]
[5]. Howard DP, Banerjee A, Fairhead JF, Perkins J, Silver LE, Rothwell PM, Oxford Vascular StudyPopulation-based study of incidence and outcome of acute aortic dissection and premorbid risk factor control: 10-year results from the oxford vascular studyCirculation 2013 127(20):2031-37.10.1161/CIRCULATIONAHA.112.00048323599348PMC6016737 [Google Scholar] [CrossRef] [PubMed]
[6]. Saito Y, Hashimoto O, Nakayama T, Sasaki H, Yumoto K, Oshima S, Right versus left coronary artery involvement in patients with type A acute aortic dissectionInt J Cardiol 2023 371:49-53.10.1016/j.ijcard.2022.10.02136257475 [Google Scholar] [CrossRef] [PubMed]
[7]. Sen G, Veitch A, Nabais S, Anterior STEMI complicating acute aortic syndrome: Mechanistic insight and bridge to surgery with intravascular ultrasound-guided primary PCIBMJ Case Rep 2022 15(3):e24805510.1136/bcr-2021-24805535260406PMC8905978 [Google Scholar] [CrossRef] [PubMed]
[8]. Huang LC, Feng ZB, Guo HW, Uncommon presentation of acute type A aortic dissection: Sleeve-severed and everted proximal right coronary artery intima without myocardial ischaemiaJ Cardiothorac Surg 2024 19(1):53810.1186/s13019-024-03040-y39304873PMC11414251 [Google Scholar] [CrossRef] [PubMed]