Circumcision is one of the oldest and most common surgical procedures performed in the world, with an estimated one in three males circumscribed globally [1-3]. It is performed on males primarily for cultural and religious reasons, usually during the neonatal period. Various personnel are involved in circumcision, including doctors, nurses, and traditional circumcisionists [4,5]. Although circumcision is generally considered to be a simple and quick procedure, it can lead to undesirable complications, which can range from mild, self-limiting events such as oedema to more severe complications like haemorrhage, UCF, infections and penile amputations [6]. Several complications following circumcision in children have been reported; however, UCF is not commonly noted as a complication [7,8].
While postcircumcision UCF is rare, it is frequently associated with procedures performed by untrained personnel. UCF is a severe, non lethal, avoidable complication that has a substantial psychological impact on the child and family, as well as economic hardships [9]. Additionally, the repair of UCF poses significant challenges for the surgeon due to high rates of recurrence, often requiring multiple surgical procedures. Many techniques for repairing UCF exist, and the choice of technique is determined by factors such as the size and location of the fistula, availability of tissues and the surgeon’s expertise [10]. The aim of this study was to examine the clinical profile of patients with UCF and the outcomes of various surgical repair techniques.
Materials and Methods
A retrospective descriptive study was conducted in the Department of General Surgery, Government Medical College, Jammu, Jammu and Kashmir, India from January 2016 to January 2023. The study was approved by the Institutional Ethics Committee (IEC/GMCJ/2023/1475).
Inclusion criteria: All patients who developed UCF after circumcision during the study period were included in the study.
Exclusion criteria: Patients with recurrent UCF, fistulae secondary to hypospadias repair, and those unfit for surgery or not consenting to surgical procedures were excluded from the study.
Data for the study was collected from institutional medical records. The category of circumcisionist, site and size of fistulae, type of repair and associated complications were recorded. After all baseline investigations and anaesthesia fitness were completed, patients were scheduled for surgery. All patients were prepared and draped before being placed under general anaesthesia in the supine position. The fistulous tract was delineated and confirmed by injecting methylene blue from the terminal portion of the urethra. At the same time, a tourniquet was applied at the base of the penis to occlude the proximal urethra.
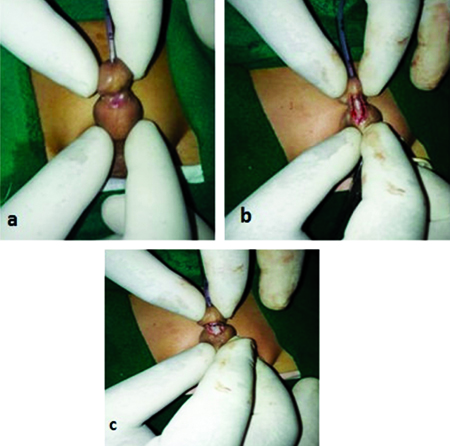
Repair of the fistula was performed according to its size and site. Fistulas smaller than 5 mm were repaired by simple closure in two layers. After inserting a 9 Fr feeding tube, a circular incision was made around the fistula following its localisation. The fistula was separated from the skin, and the margins were freshened and closed with 5-0 polyglactin interrupted sutures. The second layer of dartos fascial covering was performed, and the overlying skin was closed.
In patients with fistulas larger than 5 mm, TIP urethroplasty was performed. After localisation of the fistula and insertion of the feeding tube, the tissue ridge between the fistula and meatus was excised. A U-shaped incision was made around the fistula starting from the meatus. Skin flaps were raised on both sides, and a longitudinal incision was made in the center of the urethra to widen the urethral plate. Urethral plate tubularisation was performed using 5-0 polyglactin with interrupted sutures. A second layer of fascial covering was completed, followed by skin closure.
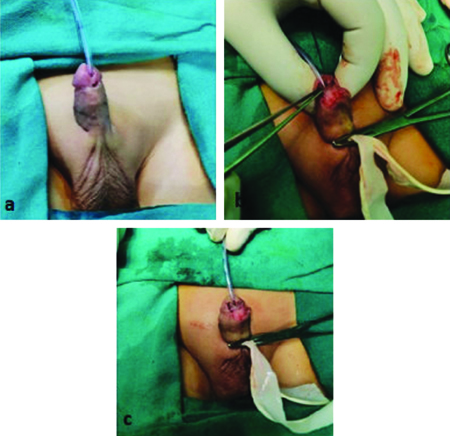
In patients with wider fistulas, where scarred tissue and little or no urethral plate were present, Mathieu flip-flap urethroplasty was performed. In this technique, a skin flap was raised from the skin proximal to the fistula ventrally after inserting the feeding tube. The flap was made 2 mm larger in both length and width than the actual size of the fistula. The flap was then mobilised from below upwards, and the skin was turned inside out. Suturing was done on both sides of the flap for tubularisation. Skin coverage was provided to complete the procedure. The feeding tube was left in place for 8-10 days. Patients were monitored for one year for any recurrence and observed for urinary stream to rule out meatal stenosis.
Statistical Analysis
The data was tabulated in an Excel sheet, and statistical analysis was conducted using Statistical Package for the Social Sciences (SPSS) version 22.0. The results were expressed in terms of frequencies and percentages.
Results
The age of the patients varied from nine months to eight years, with a mean age of 3.8 years. Most commonly, circumcision was performed traditionally (73.3%), followed by the development of UCF [Table/Fig-1]. The most common location in present study was coronal, seen in 60% of the patients, followed by subcoronal, seen in 40% [Table/Fig-2]. The size of the defect varied from 2 to 9 mm, with a mean defect of 4.93±1.31 mm. In 20 patients, the size of the fistula was less than 5 mm, while in 10 patients, it was more than 5 mm. All the patients had a single UCF. The size and location of the fistula determined the repair technique. Simple closure [Table/Fig-3] was performed in 20 patients with a fistula size <5 mm. In comparison, in eight patients, TIP repair was performed, and in two patients, Mathieu flip-flap urethroplasty [Table/Fig-4] was done for those with a fistula size of >5 mm [Table/Fig-5]. The most common complication was refistulisation, observed in four patients, followed by meatal stenosis, seen in two patients [Table/Fig-6]. Follow-up of patients was conducted from six months to two years to check for complications.
Category of circumcisionist.
| Circumcisionist | n (%) |
|---|
| Doctors | 2 (6.7) |
| Nurses | 6 (20) |
| Traditional circumcisionist | 22 (73.3) |
Location of Urethro-Cutaneous Fistula (UCF).
| Location | n (%) |
|---|
| Coronal | 18 (60) |
| Subcoronal | 12 (40) |
Simple closure of UCF: a) Fistula on ventral aspect of penis; b) Mobilisation of urethra proximally and distally; c) End to end anastomosis of proximal and distal urethra using polygalactin 5-0 followed by fascial and skin coverage.
Mathieu’s Flip-Flap repair: a) Fistula on ventral aspect of penis and catheterisation with 9fr feeding tube; b) Mathieu’s flap raised; c) Anastomosis done followed skin coverage.
| Techniques of repair | n (%) |
|---|
| Simple closure | 20 (66.7) |
| Tubularised Incised Plate (TIP) | 8 (26.7) |
| Mathieu flip flap urethroplasty | 2 (6.7) |
Complications following repair.
| Complications | n (%) |
|---|
| Refistulisation | 4 (13.3) |
| Meatal stenosis | 2 (6.7) |
| Reoperation | 1 (3.3) |
Discussion
The UCF is a significant and distressing complication following circumcision, which seems to be a simple procedure. It poses a substantial psychological and financial burden on the parents, as this complication requires multiple reconstructive surgeries [9,11]. In present study, a total of 30 patients underwent repair of UCF following circumcision over a seven-year period. In the study by Ugwu JO et al., 22 patients were operated on in eight years, and in the study by Takure AO et al., 25 patients were operated on in 10 years [12,13]. The rate was much lower than the figure reported by Ikuerowo SO et al., who had operated on 31 cases in three years [6]. The regional differences in circumcision practices and population densities could be the reason for such discrepancies.
The majority of the cases in present study were from circumcisions performed by traditionalists, followed by nurses. This is because all the circumcisions by traditionalists were done without anaesthesia, and patients might have been uncooperative during the procedure. This was contrary to the findings of Osuigwe AN et al., and Ugwu JO et al., in which the occurrence of fistula was more common when circumcision was performed by nurses [11,12]. Okeke LI et al., reported more complications in circumcisions performed by nurses than by doctors [14]. Osifo OD and Oriaifo IA also stated that complications are more common in circumcisions performed by untrained paramedics, followed by nurses and then doctors [7].
Late complications, other than fistula, can also occur with circumcision, such as meatal stenosis, granuloma formation, excessive removal of the foreskin, penile rotation, and chordee secondary to circumcision. These complications were common in patients operated on by traditional circumcisers [3].
In present study, the most common fistula location was coronal, seen in 60% of the patients, consistent with the studies by Ikuerowo SO et al., and Ekenze SO and Ezomike UO. This is expected in this region, as the urethra is more superficial and more prone to injury [6,9]. Most of the patients with UCF had a delayed presentation due to delayed recognition by the parents, as most of them in their neonatal period were in diapers. Parents usually recognised these conditions in late infancy. The size of the fistula in present study varied from 2 to 9 mm. In the study by Ikuerowo SO et al., the defect ranged from 1.5 to 12 mm, while in the study by Ugwu JO et al., the defect varied from 1 to 10 mm [6,12].
The choice of repair technique depends on the number of fistulae, their location, size, and the availability of soft tissue to reinforce the repair [15]. The most common technique used for repair in present study was simple repair. In patients with a fistula size greater than 5 mm, TIP urethroplasty and Mathieu flip flap urethroplasty were performed. In the study by Ugwu JO et al., small UCFs were repaired using primary closure [12]. In contrast, wide fistulas were repaired using TIP urethroplasty, the Thiersch-Duplay technique, or Modified Mathieu’s flap repair [8].
Even with meticulous repair of the UCF, there were instances of refistulisation. The reasons for refistulisation included poor vascularity, perifistulous scarring, large fistula size, and wound infection. This was primarily observed in patients with large fistulas >5 mm. When these recurred, they were usually smaller and amenable to simple closure in a second-stage repair. The rates of refistulisation were 18.2% in the study by Ugwu JO et al., and 16% in the study by Takure AO et al., [12,13].
Limitation(s)
The study had a retrospective design. Another limitation was the limited sample size, as most of the patients in our region reside in rural areas. This is why many patients are either neglected or present late with complications; those who are presenting to us are just the tip of the iceberg.
Conclusion(s)
The prevention of postcircumcision fistula can be achieved through meticulous surgical techniques, proper tissue handling, and adequate postoperative care. Since most circumcisions are performed by traditional practitioners, public education and awareness regarding the procedure and its complications are critical. Furthermore, the selection of appropriate repair techniques and postoperative care is necessary to prevent refistulisation.