The NTI is an established airway management technique in patients undergoing oral and maxillofacial surgeries, as it permits the administration of anaesthetic gases without compromising surgical accessibility [1,2]. Despite recent advances in airway management techniques, NTI remains challenging. Several complications, such as epistaxis and nasopharyngeal mucosal trauma, may occur during NTI [3].
The conventional technique of NTI includes the blind passage of the ETT into the oropharynx through the nose, followed by direct laryngoscopy and guiding the ETT into the trachea aided by Magill forceps. Video Laryngoscopy (VLS) has been recently described for NTI [4,5]. However, a good glottic view with VLS does not guarantee either an easy intubation or an atraumatic one. The process of traversing the nasal passage without trauma still remains a conundrum.
There are two main anatomical pathways in the nostril through which the ETT may pass during NTI. The lower pathway lies along the floor of the nose underneath the inferior turbinate, while the upper pathway lies above the inferior turbinate. Traditional teaching emphasises the importance of advancing the ETT through the lower pathway to avoid injury to the turbinates and cribriform plate [6-8]. However, Anaesthesiologists often experience difficulty in passing the ETT through the lower pathway, resulting in trauma and bleeding [9].
Railroading the ETT over an AEC, bougie, or Ryle’s tube is less traumatic and more easily navigable through the lower nasal pathway compared to blind nasal insertion. Despite multiple attempts at conventional NTI, occasionally the tube cannot be directed into the trachea but instead courses posteriorly into the oesophagus, or it could become lodged between the vocal cords or fail to pass through the subglottis due to anatomical reasons. In these cases, the AEC or the Gum Elastic Bougie (GEB) can be used as intubating aids, allowing for rapid and successful tracheal intubation [10-12]. The AEC has the added advantage of supporting oxygenation and ventilation during the process of intubation [9].
To date, there are no studies comparing conventional and AEC-guided NTI. Thus, the present study aimed to fill that gap by comparing these two techniques. The potential benefits of AEC-guided NTI in resource-limited areas of low-income countries highlight the importance of this research. The primary objectives were to assess the ease of insertion of the ETT into the oropharynx, as well as the number of attempts and total time required for insertion of the ETT into the trachea. The secondary objectives were to compare the severity of bleeding, cuff rupture, and any other complications that may arise.
Materials and Methods
This prospective interventional study was conducted in the main operation theatre complex of a tertiary care teaching hospital, Government Medical College, Kozhikode, Kerala, India from January 2020 to August 2021. Approval from the Institutional Research and Ethical Committee (IEC) was obtained prior to starting the study, with the corresponding IEC number: GMCKKD/RP2020/IEC/413.
Inclusion and Exclusion criteria: Total 70 patients with American Society of Anaesthesiologists Physical Status (ASA PS) 1 or 2, aged 18 to 65 years, with a height ranging from 150 cm to 180 cm and weighing between 40 kg and 80 kg, who were undergoing oral, maxillofacial, or neck surgeries requiring NTI, were enrolled in the study. Patients with a base of skull fracture, nasal trauma, coagulopathies, ASA PS 3 or 4, anticipated difficult airway, or those at risk of aspiration were excluded from the study.
Sample size calculation: Sample size was calculated using the formula:
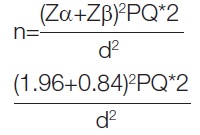
Substituting the values of P and Q from the parent study by Vadhanan P and Tripaty DK, where ‘P’ is the prevalence of successful intubation in the first group of the parent study (95%), and ‘Q’ is the prevalence of unsuccessful intubation in the first group (5%). The degree of freedom, d, was taken as 15 [11]. Substituting the values into the above equation, the sample size calculated for each group was 33.7. Total 35 patients were included in each group after obtaining written informed consent (group C conventional NTI group, n=35; group G, AEC-guided group, n=35).
Study Procedure
Before anaesthesia and surgery, patients were advised to fast for eight hours for solids and two hours for clear fluids. All patients received 150 mg of ranitidine and 10 mg of metoclopramide the night before and at 6 AM on the morning of surgery, and 0.5 mg of alprazolam was given the night before surgery. During the pre-anaesthetic check-up, the patency of the nostril was assessed using a cold spatula test. Both nostrils were prepared by instilling 0.1% w/v oxymetazoline drops one hour before the proposed surgery. An injection of glycopyrrolate (0.04 mg/kg) and dexamethasone (0.2 mg/kg) was administered intravenously 30 minutes before induction.
After preparing the theatre with the anaesthesia machine, airway equipment, emergency drugs, and drugs for the induction and maintenance of anaesthesia, the patients were shifted to the theatre. Monitors, including five-lead electrocardiograms, pulse oximeters, non invasive blood pressure monitors, and EtCO2 monitors, were attached. Patients were premedicated with an injection of morphine (0.1 mg/kg), ondansetron (0.1 mg/kg), and midazolam (0.02 mg/kg) intravenously. Anaesthesia was induced with an injection of propofol (2 mg/kg), and vecuronium (0.1 mg/kg) was administered to facilitate endotracheal intubation after confirming the adequacy of facemask ventilation. After three minutes, preservative-free lignocaine (1.5 mg/kg) was given intravenously, and NTI was performed by a qualified anaesthesiologist after 90 seconds. Cuffed nasal Ring-Adair-Elwyn (RAE) type Endotracheal Tubes (ETTs) with an internal diameter of 8 mm were selected for males and 7 mm for females.
Group C included patients in whom the conventional technique of NTI, with blind insertion of the ETT into the nasal cavity, was performed. Once the tube reached the oropharynx, direct laryngoscopy was conducted, and Magill forceps were used to guide the ETT into the larynx. Group G included patients in whom the AEC was used for intubation. A COOK AEC (11 Fr, 83 cm) was utilised. The ETT was railroaded over the lubricated AEC before insertion in such a way that the tip of the AEC protruded approximately 4 to 5 cm beyond the tip of the tube, making it easy to maneuver the AEC. The AEC with the ETT was inserted through the nose into the oropharynx, with the AEC passing through the lower nasal pathway first, followed by the ETT. Once the oropharynx was reached, direct laryngoscopy was performed, and Magill forceps were used to guide the AEC into the larynx. The ETT was then railroaded into the larynx over the AEC. External laryngeal manipulation was used if required in both groups.
The ease of insertion of the ETT into the oropharynx through the nose was assessed by the number of attempts at insertion and by navigability. Navigability was described as either smooth (grade 1), with slight resistance (grade 2), or impinged, requiring reinsertion through the same or another nostril or downsizing of the ETT (grade 3) [13]. For the purpose of present study, while performing direct laryngoscopy, the severity of bleeding was assessed using a three-point scale. No bleeding was classified as grade 1, mild bleeding, such as the presence of blood on the tracheal tube, was classified as grade 2, and severe bleeding, such as blood pooling in the pharynx requiring suction, was classified as grade 3 [14]. The number of attempts required for insertion into the trachea and the total time taken for intubation were also noted. The total time taken for intubation is defined as the time from the insertion of either the ETT or the AEC through the nose until the successful intubation of the trachea in groups C and G, respectively [15]. The incidence of complications, such as cuff rupture, was also noted.
Statistical Analysis
The data were coded in a Microsoft Excel spreadsheet. Statistical analysis was conducted using the Statistical Package for the Social Sciences (SPSS), version 18.0. Quantitative variables were expressed as means and standard deviations, while qualitative variables were expressed as frequencies and percentages. Statistical comparisons between the two groups were performed using the Student’s t-test for continuous variables and the Chi-square test for categorical variables.
Results
The demographic data of both groups were comparable. The average age of patients in group G was 57.51±5.6 years, while in group C, it was 59.66±5.8 years. Most patients in group G belonged to ASA PS 2, whereas 60% of patients in group C belonged to ASA PS 1 [Table/Fig-1].
Comparison of demographic data between the groups.
| Variables | Group-G (35) | Group-C (35) | p-value |
|---|
| Age (years), Mean±SD | 57.51±5.6 | 59.66±5.8 | 0.124* |
| Gender (male:female), n (%) | 17:18 (50:50) | 17:18 (50:50) | 1† |
| ASA PS‡ (1:2), n (%) | 13:22±37.1:62.9 | 21:14±60:40 | 0.056† |
| BMI (kg/m2) Mean±SD | 23.29±1.6 | 22.69±2.8 | 0.284* |
*Student t test; †Chi square; ‡American society of anaesthesiologists physical status
Intubation parameters were statistically significant across the groups [Table/Fig-2]. Thirty patients (85.7%) in group G were successful on the first attempt for ETT insertion into the oropharynx, while in group C, only 14 were successful on the first attempt. Similarly, for ETT insertion into the trachea, 27 patients in group G were successful on the first attempt, while two were successful on the third attempt. In group C, only 16 patients were successful on the first attempt, and six patients were successful on the third attempt. This difference was statistically significant between the groups (p<0.001). Regarding navigability, 22 (62.9%) of patients in group G experienced smooth navigability, while it was smooth only for 22.9% of patients in group C (17:18, 48.6:51.4).
Comparison of intubation parameters between the groups.
| Variables | Group | 1 | 2 | 3 | p-value† |
|---|
| Number of attempts for insertion to oropharynx | G | 30 (85.7) | 5 (14.3) | | | <0.001 |
| C | 14 (40) | 21 (60) | |
| Navigability | G | 22 (62.9) | 8 (22.9) | 5 (14.2) | <0.001 |
| C | 8 (22.9) | 6 (17.1) | 21 (60) |
| Number of attempts for insertion into trachea | G | 27 (77.1) | 6 (17.1) | 2 (5.8) | <0.001 |
| C | 13 (37.1) | 16 (45.7) | 6 (17.2) |
| Severity of bleeding | G | 26 (74.3) | 6 (17.1) | 3 (8.6) | <0.001 |
| C | 9 (25.7) | 16 (45.7) | 10 (28.6) |
†Fischer’s-exact test; Values are presented as n%
The total time taken for intubation was longer in group C (mean±SD; 107.85±64.52 seconds) compared to group G (mean±SD; 76±52.58) [Table/Fig-3]. There was a statistically significant difference in the incidence of cuff rupture, with a p-value of <0.001. Out of the 35 patients, five had ruptured cuffs in group C, whereas the incidence was zero in group G. Severe bleeding (grade 3) requiring suction was present in 10 patients in group C and only three in group G.
Comparison of total time taken for Nasotracheal Intubation (NTI) between the groups.
| Parameter | Group-G | Group-C | p-value |
|---|
| Total time taken for intubation (seconds) (mean±SD) | 76±52.58 | 107.85±64.52 | <0.01 |
Discussion
The NTI is routinely performed for oral and maxillofacial surgeries and in intensive care units where long-term ventilation is planned, as it reduces patient discomfort [16,17]. NTI under Video Laryngoscopic (VLS) guidance has recently achieved high overall and first-attempt success rates compared to flexible Fibreoptic Bronchoscopy (FOB), which is considered the gold standard for NTI. VLS-assisted NTI is highly recommended in scenarios like Coronavirus Disease-2019 (COVID-19), where Bio-aerosolisation associated with FOB is dangerous [17]. NTI under VLS guidance is easier to master than FOB. Additionally, the hemodynamic stability is greater with the former technique. The requirement for expertise and expensive equipment makes FOB a less preferred technique in low-income countries with more resource-limited settings.
The present study showed a high first-attempt success rate (85.7%) and less total intubation time in the AEC-guided group. While assessing navigability and the severity of bleeding, it was found that the AEC-guided group had better navigability (p<0.001) and less severe bleeding (p<0.001) compared to the conventional group. The incidence of cuff rupture was also lower in the guided group.
An anaesthesiologist needs to master both conventional and advanced techniques of NTI, starting from blind nasal intubation to the most recent hybrid techniques incorporating both VLS and FOB. Knowledge of anatomy is the most crucial aspect of all techniques [18]. VLS improves the Cormack-Lehane grading and the first-attempt success rate of NTI. However, the process of traversing the nasal passage atraumatically with the ETT remains a conundrum. Blind insertion of the ETT through the nose can result in injury to the turbinates, catastrophic bleeding, and often necessitates downsizing of the ETT. Although less common, avulsion of structures within the nasal cavity, dissection of retropharyngeal mucosa, and bacteremia can also occur as complications. Numerous other techniques, such as telescoping of the ETT, serial dilation of the nasal cavities, warming and softening of the ETT, and the use of vasoconstrictors, have been tried to overcome these problems, especially bleeding [19-21]. This highlights the importance of bougie or AEC-assisted intubations, which can be used with direct or VLS techniques. Bougie or AEC can be easily inserted through the lower nasal pathway without injuring the turbinates, and the ETT can be railroaded over it without any adverse sequelae. Downsizing of the ETT is seldom required [22].
The present study was conducted with 70 patients, of whom 35 underwent the conventional technique (group C) and the other 35 underwent the AEC-guided technique (group G) for NTI. The demographic features were comparable in both groups. The first attempt success rate for insertion into the oropharynx was 85.7% in group G, whereas it was only 40% in the conventional group. Abrons RO et al., conducted a randomised study comparing NTI using a bougie versus non bougie intubation with VLS, which showed a lower incidence of nasopharyngeal bleeding: 55% in the bougie group versus 68% in the non bougie group (p-value=0.033) at 60 to 90 seconds and 51% versus 70% (p-value=0.002) at five minutes [23]. They also demonstrated that the use of Magill forceps for intubation assistance was lower with the bougie technique (9% versus 28%, p-value=0.0001), and there was no significant difference in the rates of first attempt and overall success rates between the two techniques (p-value=0.133 and p-value=0.750, respectively). In a study conducted by Vadhanan P and Tripaty DK, a lesser incidence of bleeding (p-value=0.02) and better ease of insertion were reported in bougie-guided NTI, but the time taken for intubation was longer in the bougie group [11]. The results of both studies align with the present study, where an AEC was used in place of a bougie. The incidence of bleeding was lower, and the ease of insertion was better compared to the conventional technique. The first attempt success rate for NTI was significantly higher for group G (77.1% versus 37.1%). The total time taken for intubation was also significantly less in the AEC-guided group (76±52.58 seconds versus 107.85±64.52; p-value=0.01) in the present study, which is contrary to the findings of the aforementioned studies [11,23].
A literature review by Lera S. et al., regarding safer techniques for nasal intubation conducted in 2017, reveals that the use of a catheter-guided technique for nasal intubation is associated with significantly lower rates of epistaxis and airway trauma, as well as a decreased rate of morbidity and mortality in patients during the perioperative period, compared to the conventional method [24].
In a Randomised Controlled Trial (RCT) conducted by Pourfakhr P. et al., using a Glidescope with or without a bougie for nasal intubation found that the incidence of bleeding and the use of Magill’s forceps to advance the ETT was lower in the bougie-guided group compared to the conventional group (p<0.001) [12]. The mean time taken for intubation was also significantly less in comparison to the conventional group (48.63±8.53 vs. 55.9±10.76 seconds, p<0.001). These results correlate with the findings of the present study.
Additionally, directing the ETT into the trachea using Magill’s forceps has the disadvantage of cuff rupture. In the guided technique, Magill’s forceps can be used to guide the AEC, allowing the ETT to be passed over it so that the cuff remains untouched, resulting in a practically nil incidence of cuff rupture, as evidenced by the findings of the present study. In this context, AEC or bougie guidance for nasal intubation with direct visualisation or VLS becomes essential, although the literature regarding this is insufficient.
Limitation(s)
The need for an experienced and skilled anaesthetist adds to the limitations of our study, but NTI demands it. Using VLS instead of a direct laryngoscope could have made the technique simpler; however, the process of traversing the nasal passage is the same for both methods. Therefore, the results may be extrapolated. Thus, AEC-guided NTI should become routine practice alongside direct laryngoscopy or VLS.
Conclusion(s)
The AEC-guided technique of NTI has a higher first-attempt success rate and requires less time for endotracheal intubation compared to the conventional technique. The severity of bleeding and the incidence of other complications are lower with AEC-guided techniques. As this interventional study is not randomised, more randomised trials are needed to reach a definitive conclusion. Similarly, further studies with larger sample sizes are necessary to establish a more statistically significant difference between the two techniques of NTI to demonstrate that the AEC-guided method is superior to the conventional technique.
*Student t test; †Chi square; ‡American society of anaesthesiologists physical status
†Fischer’s-exact test; Values are presented as n%