The number of caesarean deliveries has risen globally, particularly in Asia, leading to a greater demand for enhanced healthcare for women undergoing these procedures [1]. Insufficient pain management causes maternal distress, which can impact mother-infant bonding and breastfeeding [2,3]. Improving postoperative analgesia not only enhances patient satisfaction but also shortens hospital stays, reduces pulmonary complications, supports early mobilisation and decreases the risk of thromboembolism [4,5]. Various analgesic options are available to mothers, including oral and intravenous medications, epidural analgesia and peripheral nerve blocks. Although epidural analgesia is widely used during labour, it is discontinued after caesarean delivery, as its effects last no more than 24 hours [6]. Conventionally, intravenous opioids, primarily fentanyl, are administered to provide effective pain relief, but they are associated with numerous dose-related side-effects such as nausea, vomiting, sedation, pruritus, respiratory depression and delayed breastfeeding [2,7].
Regional nerve block techniques offer a significant degree of postoperative pain relief and avoid complications associated with opioids [8]. Various regional anaesthetic techniques have been tried, including incision site infiltration, TAP block, II-IH nerve blocks, fascia transversalis block and quadratus lumborum block, among others [9,10]. Pain following caesarean delivery has two primary components: somatic and visceral. A significant portion of the patient’s pain is generated from the abdominal wall incision and the TAP block is reported to provide analgesia by blocking the somatic component of this pain [11]. The TAP block provides analgesia to the parietal peritoneum, skin and muscles of the anterior abdominal wall following abdominal surgery. Its relative simplicity and efficacy have made this technique widely favoured globally [12]. The somatic pain arising from the incision site is transmitted by the II-IH nerves, which innervate the L1 and L2 dermatome regions. Therefore, blocking these nerves can also alleviate the pain associated with the Pfannenstiel incision. The II-IH nerve block is an alternative approach to provide postoperative analgesia for lower abdominal surgeries [13,14]. Although the TAP and II-IH nerve blocks are effective in managing the somatic pain associated with surgical trauma to the anterior abdominal wall, they do not address the visceral pain resulting from peritoneal trauma and irritation following the surgery [15].
Abdominal field blocks, such as the TAP block and the II-IH nerve block, are considered significant components for the treatment regimen for postcaesarean pain, irrespective of the incision type (midline or Pfannenstiel). This is attributed to their opioid-sparing effects, enhanced pain relief and the technical ease of administration, which also eliminates the need for repeated injections to maintain adequate analgesia [10,13]. TAP and II-IH nerve blocks are well known and easy to perform. There are few studies related to the efficacy of TAP versus II-IH nerve blocks in the management of postoperative pain in parturients undergoing caesarean sections, but data is limited [10,16,17]. Therefore, present study aimed to compare the efficacy of bilateral TAP block and II-IH block for post-LSCS pain relief.
Materials and Methods
This randomised, clinical, double-blinded study was conducted at Dhiraj Hospital, Piparia, Vadodara, Gujarat, India from March 2021 to February 2022. Ethical clearance was obtained from the institutional review board (SVIEC/ON/MEDI/RP/21010). Written informed consent was obtained from each participant.
Inclusion criteria: American Society of Anaesthesiologists (ASA) II pregnant women, aged between 18 to 45 years who were posted for elective LSCS and willing to participate were included in the study.
Exclusion criteria: Pregnant women belonging to ASA grade III to V, those aged under 18 or over 45 years, those allergic to local anaesthetics, those with infections at the spinal anaesthesia or block site, those posted for emergency LSCS, and those undergoing LSCS under general anaesthesia were excluded from the study.
Sample size calculation: The sample size calculation was based on a previous study by Abiy S et al., [16]. Using the cumulative median tramadol consumption over 48 hours of 100 mg for the TAP group and 150 mg for the II/IH group, it was estimated that 28 patients would be needed per group to achieve a result with 80% power and a 5% probability of a Type I error for two-sided testing. Considering a 10% margin for dropouts, 30 patients were recruited per group.
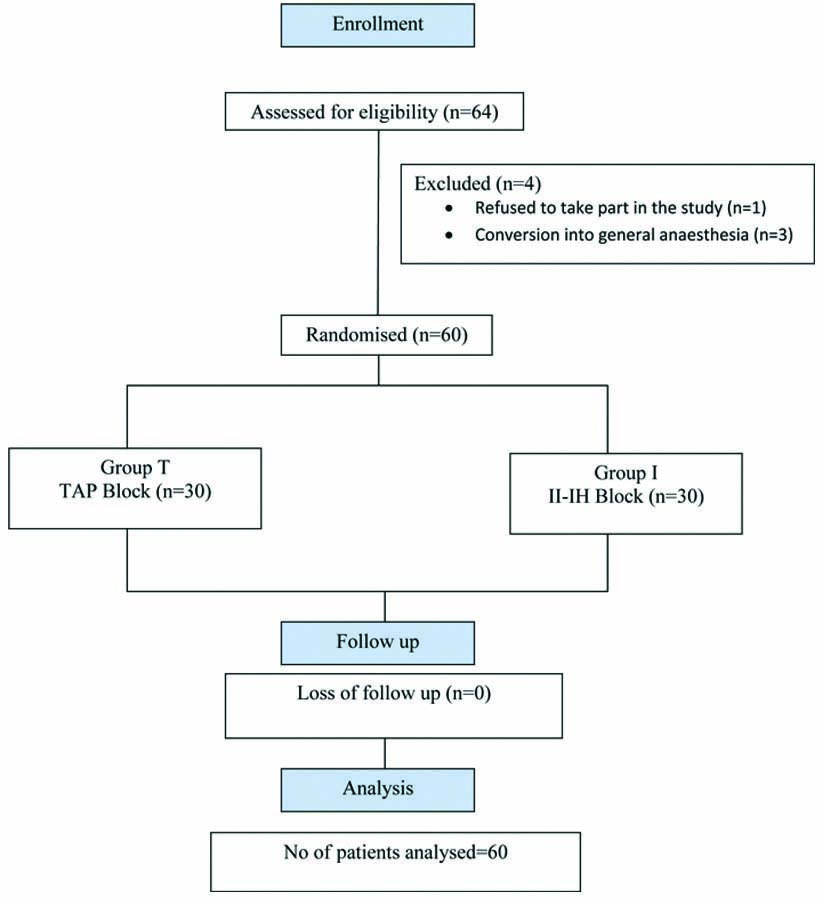
A total of 64 pregnant women were assessed for their eligibility to participate in the study, of which one pregnant woman refused to take part, and three were excluded because of failed spinal anaesthesia and conversion to general anaesthesia. Randomisation was performed using a computer-generated random number table from StatTrek. Even numbers were allocated to Group T, and odd numbers were allocated to Group I. Sealed envelopes were prepared, which were opened just before the block by the consultant anaesthesiologist who was going to perform the procedure. Assessment of the parameters was conducted by another anaesthesiologist who was unaware of which block was administered. Study was double-blinded as patient and anaesthesiologist assessing the parameters, both were unaware about the block given.
The Consolidated Standards of Reporting Trials (CONSORT) diagram is presented in [Table/Fig-1].
Study Procedure
All patients were kept nil by mouth for eight hours for solid food and two hours for clear fluids. All the patients included were premedicated with 4 mg i.v. ondansetron, 10 mg i.v. metoclopramide, and 50 mg i.v. ranitidine, administered 10 minutes before the LSCS. Non invasive monitors like electrocardiogram leads, a blood pressure cuff, and a pulse oximetry probe were attached to the patients. Baseline Heart Rate (HR) and baseline Mean Blood Pressure (MBP) were recorded. All the patients were preloaded with 10 mL/kg of Ringer’s lactate solution.
Spinal anaesthesia was administered in the left lateral position under all aseptic and antiseptic precautions using a 25 G Quinke’s spinal needle with 10 mg of 0.5% heavy bupivacaine. The level of the block was assessed (using an alcohol swab for autonomic, pinprick sensation for sensory and the modified Bromage scale for motor) and an incision was permitted when a sensory level of T6 was achieved. Only parturients with a successful spinal block (sensory block of T6) were included in this study. The duration of surgery was noted. At the end of the surgery, patients were administered either a TAP block or an II-IH nerve block, depending on the group to which they had been randomised. All blocks were performed by the principal investigator, and the assessment of the efficacy of the block was conducted by another investigator who was unaware of the type of block given to the patient.
Group T patients received a bilateral TAP block under aseptic precautions. The needle entry point was located midway between the lower costal margin and the highest margin of the iliac crest at the level of the mid-axillary line. Using a 23 G 1.5 inch blunted needle, 20 mL of 0.25% bupivacaine was administered on each side after feeling two pop sensations (loss of resistance) as the needle passed through the external oblique and internal oblique muscles, which signified the correct location of the needle.
Group I patients received the II-IH block. The needle entry point was 5 cm superior and 5 cm lateral to the Anterior Superior Iliac Spine (ASIS). Similar to Group T, using a 23 G 1.5 inch blunted needle, 20 mL of 0.25% bupivacaine was administered on each side after feeling two pop sensations.
The approach to the II-IH nerve block we followed was based on a study by Eichenberger U et al., [18]. Both the II-IH nerves lie between the internal oblique and transverse abdominal muscles, approximately 5 cm cranial and posterior to the ASIS. This has been confirmed by cadaveric studies conducted as far back as 1952 and more recently in 2008 [19-21].
To avoid intravascular injections, aspiration of the syringe for blood was performed after every 5 mL injection of the local anaesthetic. Assessment of the block’s function was conducted after confirming spinal regression below the L2 dermatome.
The investigator assessed the patients at 1, 2, 4, 6, 8, 10, 12 and 24 hours postoperatively. The primary outcomes measured were VAS (0-10), duration of analgesia and total analgesic consumption in 24 hours. The VAS score was labeled as 0 if there was no pain, and 10 was considered the worst pain ever experienced. Rescue analgesia was given if the VAS was >3, in the form of 75 mg i.v. diclofenac. The duration of analgesia was considered from the time of the block to the time of the first rescue analgesia.
The secondary outcomes measured were pulse rate, blood pressure, oxygen saturation and complications. Complications of the procedure include haematoma, infection, local anaesthetic systemic toxicity, nerve injury, peritoneal puncture, bowel haematoma, transient femoral nerve palsy and injury to the spleen, kidney, or liver, among others.
Statistical Analysis
All the data were recorded in the case record form and the master chart was created in Microsoft. The data were analysed using the standard statistical software Statistical Package for the Social Sciences (SPSS) version 18.0. A sample t-test was used for normally distributed continuous variables, while a repeated measures ANOVA test was used for intragroup VAS score comparisons. A p-value of <0.05 was considered significant, and a p-value of <0.001 was considered highly significant.
Results
Both groups were comparable in terms of demographic data (age, weight, height, BMI), baseline HR, baseline MBP and duration of surgery [Table/Fig-2].
Patients’ characteristics, baseline parameters and duration of surgery.
| Variables | Group T (Mean±SD) | Group I (Mean±SD) | p-value |
|---|
| Age (years) | 24.93±3.29 | 25.53±3.49 | 0.56 |
| Weight (kg) | 64.00±4.84 | 63.77±5.70 | 0.86 |
| Height (cm) | 153.63±7.95 | 153.93±5.73 | 0.87 |
| BMI (kg/m2) | 27.38±3.95 | 27.04±3.32 | 0.70 |
| Baseline heart rate (beats/min) | 78.97±6.54 | 79.3±6.60 | 0.80 |
| Baseline MBP (mmHg) | 83.44±10.08 | 83.76±7.37 | 0.86 |
| Duration of surgery (min) | 52.17±7.75 | 52.33±7.51 | 0.93 |
Sample t-test
VAS Score
The intergroup VAS score was not statistically significant for 24 hours postoperatively between the two groups, with p>0.05 at each time point, as shown in [Table/Fig-3]. The intragroup VAS score was statistically significant in both groups, with a p-value of 0.02 in Group T and <0.001 in Group I, as shown in [Table/Fig-4].
Intergroup compression of VAS scores between two groups (Mean±SD).
| Group | 1st hour | 2nd hour | 4th hour | 6th hour | 8th hour | 10th hour | 12th hour | 24 hour |
|---|
| Group T | 0.73±0.78 | 1.3±0.75 | 2±0.64 | 2.6±0.67 | 2.7±0.84 | 3.43±1.19 | 2.3±1.09 | 1.77±1.10 |
| Group I | 0.8±0.76 | 1.5±0.63 | 1.9±0.76 | 2.37±0.72 | 2.63±1.13 | 2.73±0.74 | 2.8±0.85 | 1.5±0.57 |
| p-value | 0.76 | 0.28 | 0.54 | 0.17 | 0.78 | 0.24 | 0.07 | 0.22 |
Sample t-test
Intragroup compression of VAS scores.
| Group | Sum of Square (SS) | Mean Square (MS) | F Statistic (df1, df2) | p-value |
|---|
| Group T | 36.77 | 1.27 | 1.67 | 0.02* |
| Group I | 37.17 | 1.28 | 2.46 | <0.001* |
Repeated measures ANOVA test
Duration of analgesia was statistically significant (p-value=0.04) between the two groups and total analgesic consumption was also statistically significant (p-value=0.01) between the two groups [Table/Fig-5].
Compression of duration of analgesia and total analgesic consumption between two groups (Mean±SD).
| Variables | Group T | Group I | p-value |
|---|
| Duration of analgesia (min) | 606±35.24 | 702±40.86 | 0.04 |
| Total analgesic consumption (mg) | 105±62.07 | 75±45.49 | 0.014 |
Sample t-test
Postoperative heart rate: The heart rate was not statistically significant at any time point. The heart rate was comparatively lower in Group I than in Group T, as shown in [Table/Fig-6].
Compression of pulse rate per minute between two groups (Mean±SD).
| Time | Group T | Group I | p-value |
|---|
| 1st hour | 88.27±8.46 | 86.93±7.52 | 0.53 |
| 2nd hour | 85.86±6.79 | 85.53±6.64 | 0.84 |
| 4th hour | 87.53±7.02 | 87.67±6.22 | 0.94 |
| 6th hour | 88.13±7.98 | 85.23±5.53 | 0.11 |
| 8th hour | 88.43±7.65 | 86.03±6.91 | 0.24 |
| 10th hour | 88.2±5.66 | 85.67±4.03 | 0.06 |
| 12th hour | 86.30±6.02 | 84.4±2.67 | 0.12 |
| 24 hour | 85.07±5.27 | 83.13±4.42 | 0.17 |
Sample t-test
Postoperative Mean Blood Pressure (MBP): There was no statistically significant difference in MBP between the two groups at any time point, as shown in [Table/Fig-7].
Compression of Mean Blood Pressure (MBP) in mmHg between two groups (Mean±SD).
| Time | Group T | Group I | p-value |
|---|
| 1st hour | 86.71±5.10 | 86.2±4.50 | 0.72 |
| 2nd hour | 86.29±4.40 | 86.93±7.46 | 0.69 |
| 4th hour | 85.02±4.33 | 85.13±3.79 | 0.91 |
| 6th hour | 86.11±4.50 | 85.68±3.31 | 0.64 |
| 8th hour | 84.20±3.90 | 84.11±3.83 | 0.92 |
| 10th hour | 84.51±4.49 | 83.89±4.81 | 0.61 |
| 12th hour | 82.96±4.48 | 83.13±3.80 | 0.87 |
| 24 hour | 82.60±3.11 | 83.00±3.43 | 0.61 |
Sample t-test
Postoperative oxygen saturation: There was no statistically significant difference in oxygen saturation between the two groups at any time point, as shown in [Table/Fig-8].
Compression of oxygen saturation in % between two groups (Mean±SD).
| Time | Group T | Group I | p-value |
|---|
| 1st hour | 99.1±0.66 | 98.83±0.65 | 0.12 |
| 2nd hour | 99.13±0.68 | 98.97±0.56 | 0.31 |
| 4th hour | 99.1±0.76 | 98.9±0.66 | 0.30 |
| 6th hour | 99.03±0.85 | 98.97±0.81 | 0.09 |
| 8th hour | 99.2±0.66 | 98.97±0.67 | 0.21 |
| 10th hour | 99.07±0.74 | 98.73±0.64 | 0.11 |
| 12th hour | 99.1±0.66 | 99.03±0.72 | 0.75 |
| 24 hour | 99.13±0.62 | 99.03±0.72 | 0.61 |
Samplet-test
Complications: None of the patients in either group developed any complications.
Discussion
The most common complaint after a caesarean section is pain. Pain is defined as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage” [22]. The postoperative pain after a caesarean section is of mild to moderate intensity, lasting for up to 72 hours. An ideal method of postcaesarean pain management should be cost-effective, safe for both the mother and the baby, require less monitoring, and use drugs that are not secreted into breast milk. Additionally, the mother should not be sedated in a way that prevents her from moving freely and caring for her newborn baby [10]. Both the TAP block and the II-IH block are cost-effective and safe, and both require less monitoring.
The use of ultrasound is considered the gold standard now-a-days; however, it is not available in every setting and is costly. Both blocks can be administered using a landmark-guided technique, making them safe and cost-effective. Present study aimed to identify the most effective and safe block in resource-limited areas for providing good analgesia to mothers. Present study showed that there was no statistically significant difference in the VAS score between the two groups for a 24-hour period postoperatively, with a p-value >0.05 at each time point. Present study results were comparable to the study conducted by Ahemed SA et al., [10] who showed that 24 hours after surgery, the NRS score at rest was (0.90±0.80) versus (0.67±0.58) (p-value=0.95), and at movement (1.2±1.07) versus (0.88±0.76) (p-value=0.09) for the TAP and II-IH groups, respectively. Similar results were obtained by Abiy S et al., [16], they found that the distributions of the pain scores (NRS) for the TAP and II/IH groups were similar. The median pain score was not statistically significantly different between the TAP and II/IH groups at 4, 8, 12, and 24 hours (p-value >0.05). In contrast, the study conducted by Jin Y et al., showed that there was no significant difference between the two groups in the first 12 hours (all p-value >0.05) [23]. However, the VAS score of the II-IH nerve block group was significantly lower than that of the TAP block group at 24 and 48 hours after the surgery (p-value <0.001). The differences in study design and the use of ultrasound in the former study might contribute to the discrepancy.
In present study, there was a statistically significant difference in the mean duration of analgesia (Group T: 606±35.24 min; Group I: 702±40.86 min; p-value: 0.04). Similar results were obtained in studies conducted by Ahemed SA et al., [10]. In their study, the mean time for the first analgesic request was 10.71±7.67 hours in the TAP group and 14.09±8.20 hours in the II-IH group, which was statistically significant, indicating a prolonged duration of analgesia in the II-IH group (p-value=0.03). This result was also consistent with the findings of a study conducted in Russia by Bessmertnyj AE et al., [24]. Their study showed that the II-IH block significantly prolonged the time to the first analgesic requirement compared to the TAP block following caesarean delivery. Similar results were also found by Panda BK et al., [25]. They concluded that the time to first rescue analgesia in Group II-IH (11.19±0.99 hours) was longer than in Group T (7.31±0.63 hours). However, a study conducted by Patel N and Dhuliya SK showed opposite results [17]. They concluded that the TAP block significantly increased the time for the first request for rescue analgesia compared to the II-IH block (p-value <0.05). The contrast in these findings may be due to the different approach used for the II-IH block in their study.
In present study, there was a statistically significant difference in total analgesic consumption (Group T: 105±62.07 mg; Group I: 75±45.49 mg of diclofenac; p-value: 0.014). Similar results were obtained by Fredrickson MJ et al., [26], they conducted a prospective randomised study to compare the analgesic effects of the ilioinguinal block and transversus abdominis plane block after paediatric inguinal surgery. They found that 30% of patients in the ilioinguinal group required ibuprofen, while 62% of patients in the TAP group required ibuprofen postoperatively, which was significantly higher compared to the ilioinguinal group (p-value: 0.037). Present study results were also consistent with the study conducted by Jin Y et al., [23]. In their study, cumulative morphine consumption was lower in the II-IH group compared to the TAP group at 24 and 48 hours after surgery, with p-values of <0.05 and <0.001, respectively. Kamal K et al., conducted a study to evaluate ultrasound-guided TAP block versus II-IH nerve block for postoperative analgesia in adult patients undergoing inguinal hernia repair [27]. They found that in the first four hours, seven patients (23.33%) in Group TAP and two patients (6.67%) in Group II-IH required tramadol. None of the patients required diclofenac in either group. The mean dose of tablet diclofenac was 200±35.96 mg in Group I and 172.5±34.96 mg in Group II (p-value=0.004). They concluded that the ultrasound-guided II-IH block decreases the postoperative analgesic requirement compared to the USG-guided TAP block, which was similar to present study.
The visceral pain impulse from the uterus reaches the spinal cord via sympathetic fibres through the inferior hypogastric plexus, which were not blocked by either block [8]. Therefore, individuals in both groups required at least one dose of systemic analgesics (injection of diclofenac sodium) to attenuate the visceral pain. In present study, there was no statistically significant difference regarding postoperative haemodynamic parameters (pulse rate and MBP), with a p-value >0.05 at any time point. Similarly, in the study conducted by Ahemed SA et al., there was no statistically significant difference in vital parameters between the two groups [10]. No side-effects were observed in either group in our study, similar to the findings of the study conducted by Sundaram A et al., [28].
Limitation(s)
This was a single-centre study, and people of the same ethnic background were studied. A multicentre study that includes various ethnic groups may improve the quality of the research.
Conclusion(s)
Both blocks were safe and provided effective postoperative analgesia for parturients undergoing caesarean sections. There was no statistically significant difference in the VAS between the two groups. However, the time to first rescue analgesia was prolonged in the II-IH group, resulting in a longer duration of analgesia compared to the TAP group. Additionally, total analgesic consumption was lower in the II-IH group compared to the TAP group. Therefore, it is concluded that II-IH nerve block is superior to the TAP block for postcaesarean section pain relief. Authors recommend the II-IH nerve block for parturients undergoing LSCS.
Sample t-test