Incidental Case of Pelvic Haemangiopericytoma: A Clinical Diagnostic Challenge and Clinicopathological Overview
Kailash Kumar Mittal1, Savita Aggarwal2, Jyoti Singh3, Arun Kumar Yadav4, Atul Mishra5
1 Professor, Department of Radiation Oncology, Uttar Pradesh University of Medical Sciences, Etawah, Uttar Pradesh, India.
2 Professor, Department of Pathology, Uttar Pradesh University of Medical Sciences, Etawah, Uttar Pradesh, India.
3 Fellow, Department of Obstretics and Gynaecology, Rainbow IVF Centre, Agra, Uttar Pradesh, India.
4 Assistant Professor, Department of Radiation Oncology, Uttar Pradesh University of Medical Sciences, Etawah, Uttar Pradesh, India.
5 Assistant Professor, Department of Radiation Oncology, Uttar Pradesh University of Medical Sciences, Etawah, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Arun Kumar Yadav, Assistant Professor, Department of Radiation Oncology, Uttar Pradesh University of Medical Sciences, Saifai, Etawah-206130, Uttar Pradesh, India.
E-mail: aruny8732@gmail.com
Haemangiopericytoma is a rare vascular tumour. Given its unusual presentation, location, and the clinical diagnostic challenges it poses, hereby, the authors present a case report of a 38-year-old female sought medical attention in the Outpatient Department (OPD) due to pain in her lower abdomen. A pelvic mass was identified in the right adnexa, pushing the uterus to the left. The patient underwent excision of the pelvic mass, considering leiomyoma as a differential diagnosis. A preoperative large mass, approximately 15×20×15 cm in size, was found between the bladder and uterus, adherent to the broad ligament. Subsequently, mass excision was performed along with total abdominal hysterectomy and bilateral salpingo-oophorectomy. The intraoperative and postoperative periods were uneventful. The histopathological report confirmed the diagnosis of haemangiopericytoma. The patient declined radiotherapy and lost to follow-up; later, she succumbed to distant metastasis to the bone and brain four years after treatment. The tumour of the pericyte cells is called haemangiopericytoma. It is considered one of the rarest types of tumours in the pelvis. Most of these tumours are asymptomatic; if they are symptomatic, it is usually due to the compression of adjacent structures or paraneoplastic effects. Computed Tomography (CT) is relevant in establishing the diagnosis, but histopathological examination is confirmatory. The preferred treatment option comprises surgery; at times, preoperative embolisation is necessary to control bleeding. Some literature has highlighted the role of radiotherapy in adjuvant settings to enhance local control. However, the ideal treatment option remains debatable. Surgery is the preferred course of treatment, occasionally following preoperative embolisation of the mass vascularisation. Surgical resection with clear margins and total removal of the tumour offers survival rates of upto 70 to 80% at five and ten years, respectively. The present case is of interest because of its location, rarity, and size.
Magnetic resonance imaging, Pelvis, Surgery, Tumour, Vascular
Case Report
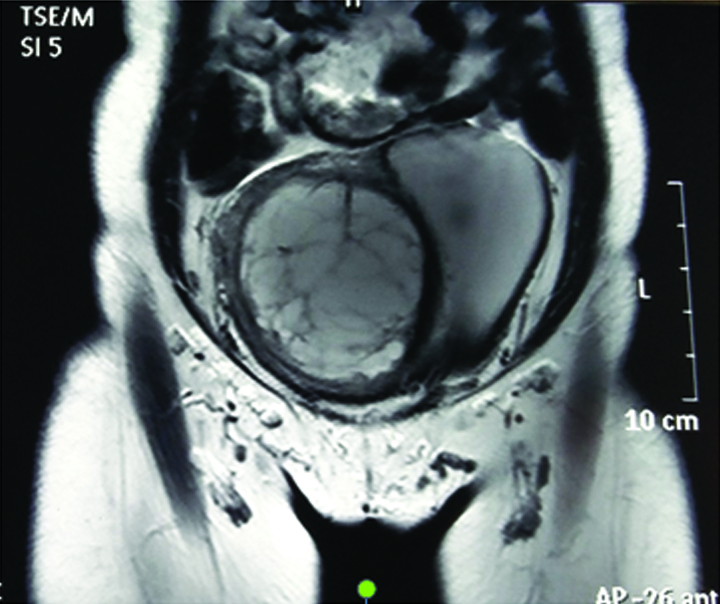
A 38-year-old married female consulted the Obstetrics and Gynaecology OPD for lower abdominal pain that had persisted for the past two months. The abdominal pain was described as dull and aching. Apart from this, there were no other complaints. The general examination was normal, but the local pervaginal examination indicated the displacement of the cervix to the left. The laboratory investigations, which included a complete blood count, liver function tests, kidney function tests, and urine routine and microscopy, were unremarkable. The Magnetic Resonance Imaging (MRI) scans revealed a solid cystic mass measuring 13.4×11.2×15 cm, with areas of high signal intensity that appeared necrotic, along with solid parts and blood vessels has been depicted in [Table/Fig-1]. The mass was located in the right adnexa and had displaced the entire uterus to the left-side. A radiological diagnosis of suspected right parametrial leiomyoma was offered [Table/Fig-1].
Coronal section of MRI showing areas of hyperintensity showing necrosis and increased number of blood vessels.
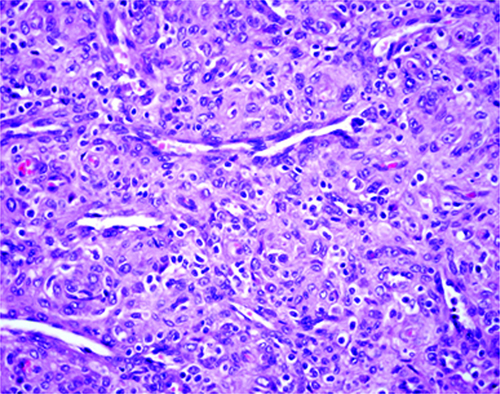
She underwent planned surgery, considering the likelihood of leiomyoma of the parametrium, and successfully had the pelvic mass removed without any intraoperative or postoperative complications. Histology {Haematoxylin and Eosin (H&E) staining} confirmed the diagnosis of pelvic haemangiopericytoma with clear resection margins and it has been depicted in [Table/Fig-2]. She was advised to undergo radiotherapy in an adjuvant setting, but she refused. Furthermore, she failed to follow-up, and four years later, she presented with brain and bone metastasis and succumbed to her progressive disease.
Section shows a spindle cell tumour with oval nuclei and numerous slit-like branching-rich vascular networks (H&E 400x).
Discussion
About 1% of vascular tumours are haemangiopericytomas, which are uncommon and may be malignant [1]. Haemangiopericytoma is a rare pericyte tumour that surrounds capillaries and venules and can occur in any location [2]. The most common locations are the lower limbs, followed by the retroperitoneal area [3]. The pelvic location is quite rare, similar to the present case in terms of the tumour’s location. Most of these tumours are asymptomatic; if they are symptomatic, it is due to the compression of adjacent structures or paraneoplastic effects, as evidenced in the case report published by Mitra AP et al., where compression led to new-onset hydroureteronephrosis [1,4]. In present case, the patient presented with complaints of pain, possibly due to compression of the adjacent organ attributed to the large size of the tumour. CT and angiography usually confirm the diagnosis; however, in this scenario, angiography was not advised because the gynaecologist was under the impression that it was a leiomyoma of the parametrium as the most probable differential diagnosis, along with the limited availability of angiography facilities in public hospitals.
Percutaneous biopsy is not recommended due to the risk of profuse bleeding. The definitive diagnosis is histopathological after analysing the surgical specimen. The distinction between benign and malignant haemangiopericytomas is based on clinical and pathological criteria. A tumour is considered malignant if it invades nearby structures, develops metastases, or recurs during follow-up [5]. Although there is no specific histological pattern of malignancy, it has been shown that size, a high mitotic index, high cellularity, and the presence of necrosis or haemorrhage can promote the development of recurrence and/or metastasis [2,5].
The treatment of choice is complete resection, sometimes preceded by embolisation of the tumour’s vascular supply to decrease the risk of bleeding [6-9]. The case study by Alvarez-Abad I et al., mentions selective embolisation prior to surgery [10]. There is disagreement about the effectiveness of chemotherapy or radiotherapy as the primary treatment. The use of adjuvant radiation therapy has been described as improving local control and reducing recurrences, although the tumour is considered relatively radio-resistant [11]. Radiation therapy was used in an adjuvant setting as per the case report published by Torigoe T et al., where a dose of 60 Gy in 30 fractions was prescribed to downsize the tumour in a recurrent setting prior to surgery; however, in the present case, the patient refused radiation [7].
The prognosis is contingent upon achieving complete resection, with five- and 10-year survival rates between 70% and 80%, depending on the published case series [12]. After resection, the recurrence rate varies between 20% and 50%. Long-term monitoring is highly recommended because recurrence may manifest at a later time [12]. The above-discussed case reports and literature has been summarised in [Table/Fig-3] [1,7,10,12].
Published case reports on pelvic haemangiopericytoma [1,7,10,12].
| S. No. | Parameters | Mitra AP et al., [1] | Alvarez-Abad I et al., [10] | Torigoe T et al., [7] | Kumar S et al., [12] | Present case |
|---|
| 1. | Age | 55 years | 63 years | 55 years | 32 years | 38 years |
| 2. | Gender | Male | Female | Male | Male | Female |
| 3. | Clinical feature | Lower urinary tract symptoms, new onset left hydroureteronephrosis | Abdominal pain | Lower abdominal pain and tenderness | Right lower abdominal pain | Lower abdominal pain |
| 4. | Radiological finding | CT scan-9.3×9.7×10.3 cm centrally necrotic mass | MRI and CT scan- 12×9×9.4 cm solid cystic mass, punctate calcifications and high vascularity | CT* scan showed 12 cm diameter encapsulated mass, central necrosis present | CT scan- 10×7 cm well-defined hyper vascular tumour | MRI scan 13.4×11.2×15 cm solid cystic mass with necrosis and high vascularity |
| 5. | Gross size | 490 gram well circumscribed fleshy mass central necrosis | - | - | Homogenous grey white surface with few areas of necrosis | - |
| 6. | Microscopy | Immunohistochemistry (IHC) Vimentin positive and Cluster of Differentiation (CD) 34 positive
ki67-15% | - | Abundant blood vessels, round or spindle-shaped cells, including dilated staghorn-shaped vessels. Silver impregnation reticulin fibres around vascular spaces and tumour | Round to spindle cells vesicular chromatin, inconspicuous nucleoli, moderate eosinophilic cytoplasm, No capsular breach | Spindle cell tumour with oval nuclei and numerous slit-like vascular structure |
| 7. | Surgery | Wide local excision | Selective embolisation followed by wide local excision | Wide local excision | Wide local excision | Wide local excision |
| 8. | Radiation | Not given | Not given | 60 Gy 30 fractions in recurrent setting to down size the tumour | Not given | Patient refused |
| 9. | Chemotherapy | Not given | Not given | Not given | Not given | Not given |
| 10. | Follow-up | 23 months | Not mentioned | 7 years and 2 months | 2 years | Four years |
| 11. | Recurrence | Not reported | Not reported | Local recurrence only reported for which radiation followed by surgery was done | Not reported | Brain and bone metastasis |
| 12. | Metastasis | Not reported | Not reported | Not reported | Not reported | Brain and bone |
*CT: Computed tomography; MRI: Magnetic resonance imaging
Conclusion(s)
Haemangiopericytoma is a rare vascular tumour that is usually found in the lower limb, followed by the retroperitoneum, although the pelvis is an exception. The invasion of adjacent structures, distant metastases, and histopathological findings can distinguish it as benign or malignant. Surgery plays a pivotal role, with adjuvant radiation providing good local control. Patients with this condition should have regular follow-ups to rule out recurrences or metastases.
*CT: Computed tomography; MRI: Magnetic resonance imaging
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 15, 2024
Manual Googling: Sep 28, 2024
iThenticate Software: Oct 15, 2024 (3%)
[1]. Mitra AP, Maas M, Zainfeld DE, Schuckman AK, Pelvic hemangiopericytoma: A case report and review of the literatureUrol Case Rep 2020 32:10124710.1016/j.eucr.2020.10124732435596PMC7232097 [Google Scholar] [CrossRef] [PubMed]
[2]. Muñoz AK, Berek JS, Fu YS, Heintz PA, Pelvic hemangiopericytomas: A report of five cases and literature reviewGynecol Oncol 1990 36(3):380-82.10.1016/0090-8258(90)90147-D2318448 [Google Scholar] [CrossRef] [PubMed]
[3]. Wilbanks GD, Szymanska Z, Miller AW, Pelvic hemangiopericytoma: Report of 4 patients and review of the literatureAm J Obstet Gynecol 1975 123(6):555-69.10.1016/0002-9378(75)90876-51200042 [Google Scholar] [CrossRef] [PubMed]
[4]. Lorigan JG, David CL, Evans HL, Wallace S, The clinical and radiologic manifestations of hemangiopericytomaAJR Am J Roentgenol 1989 153(2):345-49.10.2214/ajr.153.2.3452665453 [Google Scholar] [CrossRef] [PubMed]
[5]. Goldman SM, Davidson AJ, Neal J, Retroperitoneal and pelvic hemangiopericytomas: Clinical, pathologic correlationRadiology 1988 168(1):13-17.10.1148/radiology.168.1.32890863289086 [Google Scholar] [CrossRef] [PubMed]
[6]. Fard-Aghaie M, Stavrou GA, Honarpisheh H, Niehaus KJ, Oldhafer KJ, Large hemangiopericytoma of the pelvis using a multidisciplinary approachWorld J Surg Oncol 2015 13:26110.1186/s12957-015-0675-626311516PMC4551704 [Google Scholar] [CrossRef] [PubMed]
[7]. Torigoe T, Higure A, Hirata K, Nagata N, Itoh H, Malignant hemangiopericytoma in the pelvic cavity successfully treated by combined-modality therapy: Report of a caseSurg Today 2003 33(6):479-82.10.1007/s10595-002-2505-012768379 [Google Scholar] [CrossRef] [PubMed]
[8]. Wise RA, Hemangiopericytoma: Surgical considerationsAMA Arch Surg 1952 65(1):201-10.10.1001/archsurg.1952.0126002021302114932614 [Google Scholar] [CrossRef] [PubMed]
[9]. Scott M, Reith JD, Mendenhall WM, Radiation therapy for hemangiopericytomaInternational Journal of Radiation Oncology Biology Physics 2013 87:S611-12.10.1016/j.ijrobp.2013.06.1617 [Google Scholar] [CrossRef]
[10]. Álvarez-Abad I, García-González JM, Agirre-Etxabe L, Quintana-Rivera AM, Colina-Alonso A, Pelvic hemangiopericytoma. An unusual location of a vascular tumorRev Esp Enferm Dig 2017 109(1):69-70.10.17235/reed.2016.4165/201526912344 [Google Scholar] [CrossRef] [PubMed]
[11]. Krengli M, Cena T, Zilli T, Radiotherapy in the treatment of extracranial hemangiopericytoma/solitary fibrous tumor: Study from the Rare Cancer NetworkRadiotherapy and Oncology 2019 144:114-20.10.1016/j.radonc.2019.11.01131805515 [Google Scholar] [CrossRef] [PubMed]
[12]. Kumar S, Savlania A, Sandeep M, Rastogi P, Hypervascular pelvic hemangiopericytoma successfully excised without embolizationIndian J Surg Oncol 2020 11(Suppl 2):250-52.Available from: https://doi.org/10.1007/s13193-020-01176-610.1007/s13193-020-01176-633364711PMC7732949 [Google Scholar] [CrossRef] [PubMed]