Odontogenic inflammatory lesions represent inflammatory changes residing in the pulpal, periapical and periodontal tissue regions that are associated with pain and swelling. Local variations in tissue temperature significantly imply alterations in blood supply and tissue metabolism characteristic of a particular pathology [1]. Body surface temperature changes can be used to detect a variety of diseases since they indicate variations in blood flow and metabolism in particular regions [2]. Therefore, absolute differences in thermal levels should be measured during the diagnostic assessment of the lesion using a non invasive, non ionising and non contact diagnostic imaging technique known as infrared thermography [3].
Thermography can be used as a diagnostic tool in various medical conditions and has potential applications in dentistry, including assessing temperature changes and diagnosing odontogenic foci of infection in the oral cavity, inflamed periodontal diseases, dental abscesses, temporomandibular joint diseases [4], as well as, detecting intraosseous temperature changes during dental implant placements, detecting infra-alveolar nerve deficits [5] and detecting maxillary sinusitis and salivary gland pathologies [6]. It has also been used to assess postoperative pain in extracted teeth, paving the way to assess the progress in healing of the extracted socket [7] and to characterise the orofacial pain, such as burning mouth syndrome [8]. Recent research has been conducted on detecting the burning sensation of the tongue in patients with oral lichen planus [9].
Inflammatory lesions such as periapical and periodontal abscesses can be detected using infrared thermography, as it clearly indicates a hot spot at the affected site. Thermograms are images that capture the heat distribution in tissues using an infrared camera, which is a key indicator of the presence of an underlying medical condition [10]. It is critically important to evaluate the thermal alterations that indicate underlying pathological changes. The main advantage of using this technique is its non ionising radiation, which allows visual perception through the differences in colour changes when capturing thermal patterns.
The change in temperature due to increased blood flow (vasodilation) results in heat and redness of inflammatory lesions [11,12]. On the other hand, pain can be a patient’s subjective experience during this inflammatory process. Upon administration of medications such as Non Steroidal Anti-inflammatory Drugs (NSAIDs) and acetaminophen, the inflammatory signs, including pain and temperature (heat), are usually reduced [13]. The pain threshold is subjective and the patient’s perspective on pain should be considered when measuring physiological and pathological changes. Previous research has compared pain and thermal changes in Temporomandibular Disorders (TMD) patients [14]; however, no studies have been performed in inflammatory odontogenic pathologies. Thus, the present study innovates by correlating pain and thermal levels in patients diagnosed with inflammatory lesions such as apical periodontitis, periapical abscess, periodontal abscess and endo-perio lesions at baseline and on two follow-up days after administering medications, thereby ensuring a gradual reduction in pain and thermal levels during follow-up.
The present study was conducted to measure and compare the thermal levels (°C) of inflammatory lesions, including apical periodontitis, periapical abscess, periodontal abscess and endo-perio lesions.
Materials and Methods
The prospective observational study was conducted in the Department of Oral Medicine and Radiology, Indira Gandhi Institute of Dental Sciences, Puducherry, India, from October 2022 to April 2023. The present study was approved by the Institutional Ethical Committee (IEC) (Ref No: IGIDSIEC2022NRP05PGRJOMR).
Inclusion criteria: Patients who were clinically diagnosed with inflammatory periapical and periodontal lesions were included in the study.
Exclusion criteria: Patients with other inflammatory conditions of odontogenic and non-odontogenic origin, severe cognitive mental and locomotor deficiencies, as well as, those with acute illnesses, critically ill patients, pregnant women and children were excluded from the study.
Sample size: A total of 60 patients (30 males and 30 females) were included, with an age range of 18-60 years, selected by convenience sampling.
Study Procedure
Patient information regarding the demographic data (age and sex), clinical diagnosis, and radiographic diagnosis was also collected. Informed consent was obtained from the patients. Intraoral examinations and radiographic investigations of the affected tooth were conducted using an Intraoral Periapical Radiograph (IOPAR). After obtaining the clinical and radiographic data, the assessment of pain was recorded using the VAS, which involved making a mark on a 10 cm line that represents a continuum between ‘no pain’ and ‘worst pain’. The patient underwent measurement of thermal levels in the affected region using a thermal camera. Thermographic data were acquired using the FLIR One Pro infrared camera with Multi-Spectral Dynamic Imaging (MSX) (FLIR Systems, Oregon, USA) and the images were stored on a memory card in Tagged Image File Format (TIFF) file format and processed using a specialised application (FLIR Tools Thermal Analysis and Reporting; Desktop, FLIR Systems, Oregon, USA).
The camera was calibrated by considering the emissivity parameters of the human body (ε=0.98 and λ>2 μm), ambient conditions (humidity and temperature), a thermal range from 20° to 250°C±3°C, a pixel infrared resolution of 160×120 and adequate shading was selected for optimal colour registration.
Patients were asked to refrain from smoking, eating and drinking prior to the examination and they remained at rest for 10 minutes before the procedure. During this adaptation process, patients did not engage in any physical activity, chew or touch their facial skin. Patients were instructed to rinse their oral cavity with room temperature water for one minute and then wait for five minutes to maintain a stable intraoral temperature. The area of the room was approximately 15 m2, with no artificial lighting and the relative humidity was set between 50% and 70%. The ideal room temperature was also noted.
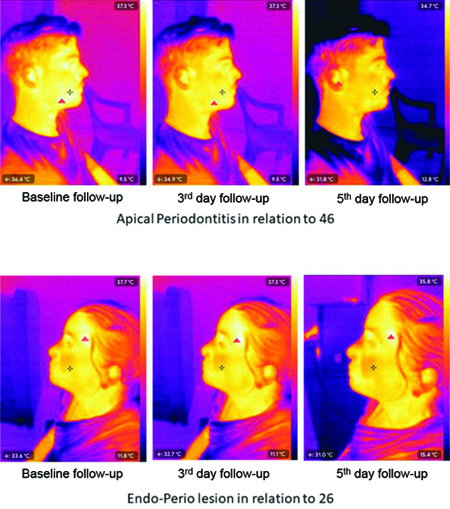
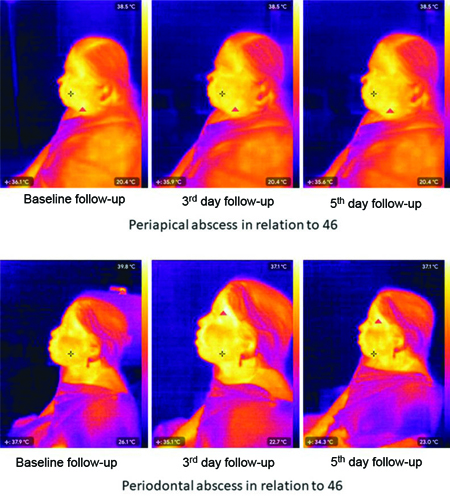
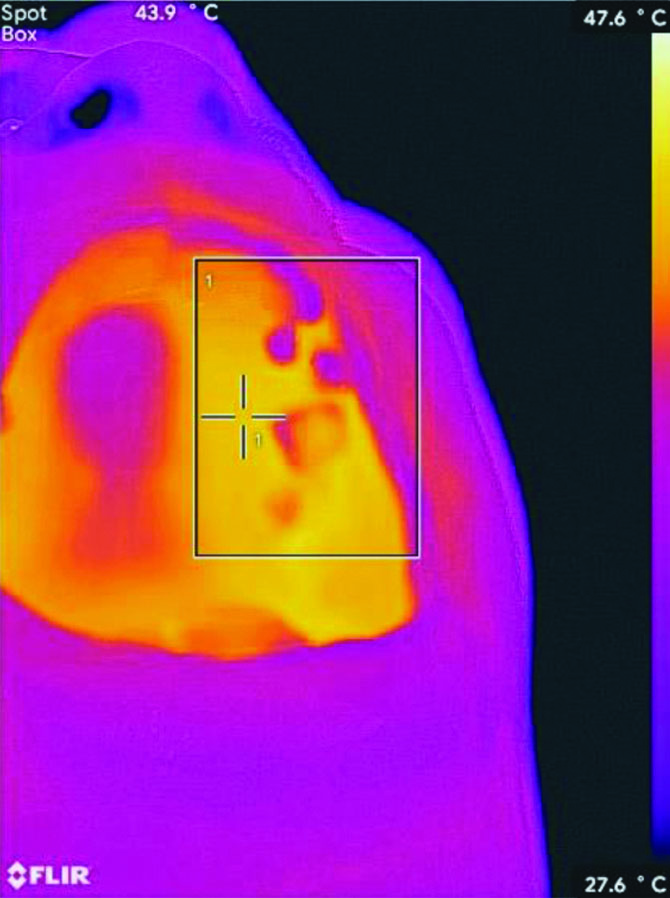
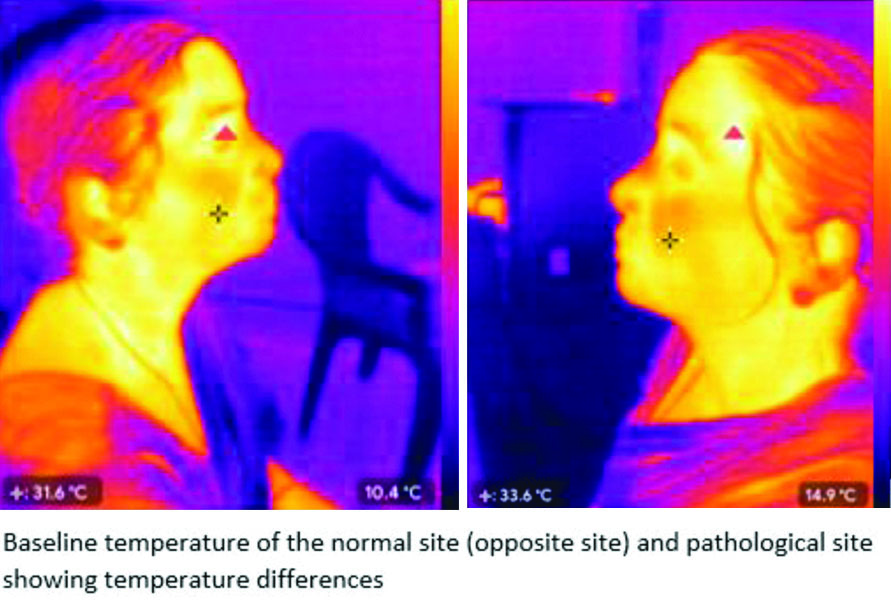
The thermal camera was focused 1 metre from the affected side of the lesion, based on the ideal interdistance between the thermal camera and the object, which ranges from 0.7-1.5 metres [8]. The data were captured using the camera with an accurate focal area and emissivity five times at one-minute intervals. The intraoral temperature of the affected site was also measured and the data were saved in degrees Celsius (°C) [Table/Fig-1,2 and 3]. The thermograms depicted the subject’s face and the surroundings in different colours according to temperature. The collected data consisted of thermal images with reference margins and regions of interest noted on the images. The images were collected in Joint Photographic Experts Group (JPEG)/Portable Network Graphics (PNG) format and the data were recorded [Table/Fig-1,2,3 and 4].
Thermal changes of apical periodontitis and endo-perio lesions measured on the baseline, 3rd day and 5th day of follow-up.
Thermal changes of periapical and periodontal abscesses measured on the baseline, 3rd day and 5th day of follow-up.
Thermal changes measured intraorally at left maxillary molar region.
Thermal changes of the affected side and contralateral unaffected side.
The baseline thermographic data were collected and noted. The patients were advised on medication, informed consent was obtained and the complications were explained. Asymptomatic patients were selected for the study. Since treatment was not initiated for five days, patient safety was ensured with antibiotic coverage and analgesics (standard regimen of antibiotics and analgesics for the management of pain and inflammation for five days) to minimise the risk of infection. However, if any emergency treatment was required, the authors advised the patients to seek treatment. Patients were recalled on the 3rd and 5th days for the measurement of thermographic data.
Statistical Analysis
The collected data were systematically organised using Microsoft Office Excel 2016 and statistical analysis was conducted with Statistical Package for the Social Sciences (SPSS) software version 17.0. The means and standard deviations for age, gender, VAS score and thermal levels of inflammatory lesions were calculated as descriptive statistics. Comparisons among the thermal levels (°C) were analysed using repeated measures ANOVA. The correlation between the VAS score and thermal levels was assessed using Spearman’s correlation coefficient test. The p-value <0.05 was considered statistically significant.
Results
The total number of 60 patients (30 males and 30 females) was assessed in the study, with a mean±SD age of 39.87±13.17 years. The mean thermal level (°C) was highest at baseline (36.08±1.88 °C) and lowest on the fifth day of follow-up. The mean difference in thermal levels (°C) between baseline and the fifth day of follow-up was 2.39 °C [Table/Fig-5]. Pair-wise comparisons of thermal levels between baseline, the third day and the fifth day of follow-up were statistically significant (p-value ≤0.05) [Table/Fig-6].
Mean and standard deviation for thermal level (°C) at the baseline, 3rd day and 5th day of follow-up.
| Thermal level (°C) | N | Mean (°C) | Standard deviation | 95% Confidence interval lower bound upper bound | p-value |
|---|
| Baseline | 60 | 36.08 | 1.88 | 35.59 | 36.56 | 0.0012 |
| 3rd day of follow-up | 60 | 34.80 | 1.52 | 34.41 | 35.19 |
| 5th day of follow-up | 60 | 33.69 | 1.64 | 33.26 | 34.11 |
Comparison of thermal level changes at the baseline, 3rd day and 5th day of follow-up.
| Multiple comparison | Follow-up period | Mean difference | Std. Error | Significance | 95% confidence interval for difference |
|---|
| Lower bound | Upper bound |
|---|
| Baseline | 3rd day of follow-up | 1.275* | 0.104 | <0.01 | 1.018 | 1.532 |
| 5th day of follow-up | 2.391* | 0.176 | <0.01 | 1.957 | 2.826 |
| 3rd day of follow-up | Baseline | -1.275* | 0.104 | <0.01 | -1.532 | -1.018 |
| 5th day of follow-up | 1.116* | 0.132 | <0.01 | 0.792 | 1.441 |
| 5th day of follow-up | Baseline | -2.391* | 0.176 | <0.01 | -2.826 | -1.957 |
| 3rd day of follow-up | -1.116* | 0.132 | <0.01 | -1.441 | -0.792 |
The thermal levels (°C) at baseline, on the third day of follow-up and on the fifth day of follow-up for dental caries with apical periodontitis were 35.38±1.32, 34.38±1.65 and 33.21±1.33, respectively; for periapical abscess, they were 36.41±1.47, 35.04±1.10 and 33.89±1.43; for periodontal abscess, they were 35.61±1.88, 34.13±1.67 and 33.44±1.23; and for endo-perio lesions, they were 34.86±1.59, 34.07±0.69 and 33.23±1.49, respectively. A significant difference was observed in the thermal levels for different odontogenic lesions on all three days (p-value <0.05) [Table/Fig-7].
Thermal level (°C) changes in groups about patients’ age, gender and lesions.
| Parameters | Baseline | 3rd day of follow-up | 5th day of follow-up |
|---|
| Age-wise thermal level changes (Mean±SD) |
| 18-40 years | 36.13±2.02oC | 34.87±1.54oC | 33.80±1.68oC |
| 41-60 years | 36.02±1.75oC | 34.73±1.51oC | 33.56±1.62oC |
| p-value | 0.83 | 0.72 | 0.58 |
| Gender-wise thermal level changes (Mean±SD) |
| Male | 36.10±1.54oC | 34.85±1.37oC | 33.85±1.73oC |
| Female | 36.06±2.19oC | 34.75±1.67oC | 33.52±1.57oC |
| p-value | 0.93 | 0.81 | 0.43 |
| Thermal level changes in odontogenic inflammatory lesions (Mean±SD) |
| Dental caries with apical periodontitis | 35.38±1.32 | 34.38±1.65 | 33.21±1.33 |
| Periapical abscess | 36.41±1.47 | 35.04±1.10 | 33.89±1.43 |
| Periodontal abscess | 35.61±1.88 | 34.13±1.67 | 33.44±1.23 |
| Endo-perio lesion | 34.86±1.59 | 34.07±0.69 | 33.23±1.49 |
| p-value | 0.002* | 0.0073* | 0.0017* |
*The p-value <0.05 was considered statistically significant
The VAS score showed an average of 6.17±1.24 on the baseline day and 3.37±1.15 on the fifth day of follow-up in patients aged 18-40 years. In patients aged 41-60 years, the average VAS score was 6.64±1.33 on the baseline day and 3.22±0.98 on the fifth day of follow-up, respectively. The mean average VAS score for males on the baseline day and the fifth day of follow-up was 6.10±1.40 and 3.40±1.13, respectively, indicating a comparative reduction in VAS score. The mean average VAS score for females on the baseline day and the fifth day of follow-up was 6.63±1.40 and 3.2±0.80, respectively. The mean VAS score reduction for periapical abscess was from 6.48 to 3.17, for endo-perio lesions from 6.5 to 3.5, for periodontal abscess from 6.33±1.50 to 4.0±1.17 and for dental caries with apical periodontitis from 6.0 to 3.5. No significant difference was observed in the VAS scores among different age groups, genders, or odontogenic lesions [Table/Fig-8].
VAS score changes in groups on patients’ age, gender and lesions.
| Parameters | Baseline | 5th day of follow-up |
|---|
| Age-wise VAS score changes (Mean±SD) |
| 18-40 years | 6.09±1.32 | 3.29±1.10 |
| 41-60 years | 6.65±1.54 | 3.30±0.84 |
| p-value | 0.13 | 0.93 |
| Gender-wise VAS score changes (Mean±SD) |
| Male | 6.1±1.47 | 3.4±1.13 |
| Female | 6.63±1.40 | 3.2±0.80 |
| p-value | 0.15 | 0.43 |
| VAS score changes according to odontogenic inflammatory lesions (Mean±SD) |
| Dental caries with apical periodontitis | 6.0±1.12 | 3.5±1.23 |
| Periapical abscess | 6.48±0.96 | 3.17±0.89 |
| Periodontal abscess | 6.33±1.50 | 4.0±1.17 |
| Endo-perio lesion | 6.5±1.23 | 3.5±1.10 |
| p-value | 0.784 | 0.788 |
The correlation coefficient between thermal levels (°C) and VAS scores at baseline and the fifth day was 0.119 and -0.043, respectively, which was not statistically significant (p-value=0.366 and 0.743, respectively) [Table/Fig-9].
Spearman correlation coefficient test comparing the thermal changes and pain.
| Correlation coefficient test | Significance (2-tailed) | Thermal level (follow-up) | VAS (follow-up) |
|---|
| Baseline day | 3rd day | 5th day | Baseline day | 5th day |
|---|
| Thermal level (Baseline day) | Correlation coefficient | - | 0.915** | 0.726** | 0.119 | -0.198 |
| Sig. (2-tailed) | - | <0.01 | <0.01 | 0.366 | 0.130 |
| Thermal Level (3rd day follow-up) | Correlation coefficient | 0.915** | - | 0.781** | 0.094 | -0.213 |
| Sig. (2-tailed) | <0.01 | - | <0.01 | 0.476 | 0.102 |
| Thermal Level (5th day follow-up) | Correlation coefficient | 0.726** | 0.781** | - | 0.110 | -0.043 |
| Sig. (2-tailed) | <0.01 | <0.01 | - | 0.401 | 0.743 |
| VAS (Baseline day) | Correlation coefficient | 0.119 | 0.094 | 0.110 | - | -0.178 |
| Sig. (2-tailed) | 0.366 | 0.476 | 0.401 | - | 0.173 |
| VAS (5th day follow-up) | Correlation coefficient | -0.198 | -0.213 | -0.043 | -0.178 | - |
| Sig. (2-tailed) | 0.130 | 0.102 | 0.743 | 0.173 | - |
p-value=**Correlation is significant at the 0.01 level (2-tailed)
r- value=Correlation coefficient
Discussion
The present study demonstrated no significant correlation between thermal levels and VAS scores at both baseline and on the fifth day. The primary purpose of using infrared thermography in the study was to establish this imaging modality as a diagnostic tool for inflammatory periapical and periodontal lesions. The advantage of a non ionising, non contact method for measuring thermal changes at the inflammatory sites distinguishes it from routine diagnostic tools such as periapical radiography.
The inflammatory periapical lesions, including apical periodontitis, periapical abscess, periapical cysts and periodontal abscess, tend to exhibit changes in temperature at the affected site. These thermal changes are caused by the local vascular and inflammatory response to the infection [11]. Conditions such as apical periodontitis and pulp necrosis are usually asymptomatic in their acute stages and clinical and radiographic examinations do not provide any valuable diagnostic outcomes. Local changes at this site result in modulation of tissue mechanisms and blood supply (vasodilation) of the affected inflammatory lesion, leading to definitive temperature changes [12]. Therefore, quantitative thermal parameters should be measured at the affected site to aid in diagnostic assessment. In conditions such as secondary infiltration or chronic inflammation, pain and oedema develop as the disease progresses, which causes the thermal parameters of the inflammatory site to modulate [15].
With advancements in infrared thermography using portable thermal devices, changes in temperature can be easily detected. The thermal images of the body surface at the area of interest can be assessed, showing tissue metabolism and variability of blood flow. The present study measured thermal changes across different age groups and genders and compared the thermal changes among each inflammatory lesion. Infrared thermography was used to measure thermal levels in patients diagnosed with inflammatory lesions such as apical periodontitis, periapical abscess, periodontal abscess and endo-perio lesions at baseline and during two follow-ups. Follow-ups on the 3rd day and 5th day were performed to ensure the rate of thermal changes at the inflammatory site. The mean thermal level measured at baseline for apical periodontitis was 35.38°C, while for periapical abscess, it was 36.41°C, respectively, which was statistically significant (p-value=0.001). Aboushady MA et al., conducted a study in 2021 to measure thermal levels for patients diagnosed with periapical abscess and apical periodontitis. In this study, the mean thermal level at baseline for acute periapical abscess was 37.26°C, chronic periapical abscess was 35.03°C and apical periodontitis was 36.07°C, respectively, all of which were statistically significant (p-value=0.000) [16]. Ammoush M et al., also conducted a study to measure thermal levels for patients diagnosed with cellulitis and dental abscess using thermography, which showed a significant increase in thermal levels (p-value=0.0485), similar to the present study [17].
The thermal levels among patients diagnosed with inflammatory lesions such as apical periodontitis, periapical abscess, periodontal abscess and endo-perio lesions were not significantly different between genders (p=0.83). However, the study conducted by Ammoush M et al., among male and female patients diagnosed with cellulitis and dental abscess showed an increase in thermal levels in female patients [17]. This may be due to changes in the rate of release of female sex hormones, which could cause an increase in thermal levels in female subjects [18].
The present study showed a significant reduction in the VAS score associated with dental caries, apical periodontitis, periapical abscess, periodontal abscess and endo-perio lesions after medication. The study conducted by da Silva PB et al., Montebugnoli L et al., and Farokh-Gisour E et al., compared the VAS scores among different inflammatory lesions and found a significant reduction [19-21].
In the present study, the correlation between the VAS score and thermal levels at baseline and on the 5th day of follow-up was not statistically significant (p-value=0.366). This observation can be attributed to the fact that the VAS is subjective in nature and depends on an individual’s pain threshold, whereas thermal levels (°C) are objective assessments that are more reliable. Since there is a dearth of literature related to studies correlating pain and thermal changes in odontogenic inflammatory conditions, the authors have compared the results of the present study to the study conducted by Barbosa JS et al., which correlated thermal levels and pain intensity in patients with temporomandibular disorders. They stated that the correlation was not statistically significant (p-value=0.366) [14], which is similar to the findings of the present study.
Infrared thermography is an emerging non invasive tool in medicine and dentistry that aids in the diagnosis of underlying inflammatory conditions. This method helps to complement the clinical routine and provides added value in comparison with other diagnostic methods. It is also an asset in the diagnosis and prognosis of tooth fractures or vertical cracks at an early stage; therefore, it would be important to conduct clinical studies in patients with this indication [22]. Thermography can also help in the diagnosis of myofascial pain and orofacial pain by measuring hot and cold thermographic spots. At the surgical level, this procedure can help control temperature to reduce the possibility of bone necrosis and cell apoptosis, which may improve the success rate of osteotomies and implant placements. The real-time imaging capability of infrared thermography can be indicated for pregnant patients for detecting inflammatory changes, as it is non invasive and non radiating [23].
The present study assessed thermal changes in patients diagnosed with inflammatory periapical and periodontal lesions, conducted in a chair-side setup with appropriate environmental conditions, ensuring a non invasive approach for greater patient convenience. The rate of change in thermal levels after follow-up also indicates regression of inflammation at the pathological site of the lesion.
Limitation(s)
Although infrared thermography has several advantages, the common limitations in the present study include the precise detection of thermal changes in the periapical region of the particular tooth and slight difficulty in differentiating the thermal changes among the periapical sites and the adjacent structures, such as maxillary sinus pathology or underlying bony lesions. However, more studies with a larger sample size and thermography devices with high precision and sensitivity might aid in detecting the inflammatory changes in apical periodontitis, periapical abscess, periodontal abscess and endo-perio lesions.
Conclusion(s)
The results of the present study indicated that the highest thermal changes were recorded in patients diagnosed with periapical abscess, along with a reduction in pain intensity and thermal levels during two follow-ups after medication. However, the correlation between pain and thermal levels was not statistically significant at baseline or on the fifth day of follow-up. Therefore, thermography can be used as a diagnostic tool for inflammatory conditions such as dental caries with apical periodontitis, periapical abscess, periodontal abscess and endo-perio lesions, but it cannot predict pain in patients.
*The p-value <0.05 was considered statistically significant
p-value=**Correlation is significant at the 0.01 level (2-tailed)
r- value=Correlation coefficient