Chronic Obstructive Pulmonary Disease (COPD) is a top cause of death. It is a lung disease that gets worse over time and includes emphysema and chronic bronchitis, causing blocked airflow. Hospitalisations, mortality and exacerbations of COPD are all increased by poor air quality. Significant occupational dosages include excessive pesticide exposure and home air pollution from burning coal, wood, animal dung and crop residues. Besides medical treatments, pulmonary rehabilitation is crucial for patient recovery from hospital to home. This study focuses on a 67-year-old man who visited a respiratory clinic with breathing problems for the past 15 days and chest pain for the past week. He also had a yellowish cough and occasional fever in the last week. With a 5-year history of COPD, he used an inhaler twice daily. His symptoms worsened in winter but stayed the same throughout the day. A chest X-ray confirmed a flare-up of COPD. A two-week pulmonary rehab plan with physical therapy was recommended. Before starting treatment, a baseline assessment was done, including measures like Modified Medical Research Council (mMRC) grading for breathlessness, 6-Minute Walk Distance (6MWD) and chest movement. Following the completion of the instructed pulmonary rehabilitation, significant improvements in dyspnoea grading, 6MWD, and thoracic were found. The findings imply that when modified to each patient’s specific requirements and capabilities, an organised pulmonary rehabilitation program can have an important beneficial therapeutic impact on those suffering from Acute Exacerbation of Chronic Obstructive Pulmonary Disease (AECOPD).
Breathlessness, Chest movement, 6 minute walk test
Case Report
A 67-year-old male patient visited the respiratory medicine clinic with significant respiratory symptoms, including breathlessness (according to mMRC III) [1] over the past 15 days, productive cough, chest pain and intermittent fever over the past week. The patient reported experiencing an increase in symptoms during the winter season, without any variation throughout the day, and had a history of biomass exposure. Additionally, the patient was a confirmed diagnosed case of COPD for the past five years and was currently being managed with budamate and ipratropium inhalers for the last five years. Remarkably, the patient retained his habit of chewing tobacco but stopped consuming alcohol and smoking three years ago after 30 years of consumption. Furthermore, the patient had experienced a recent loss of appetite and weight loss of 2-3 kilograms.
After investigations, results of routine blood reports showed a decrease in haemoglobin (10.9 gram/deciliter) (normal -13-18 g/dL) and erythrocyte count (3.93 million cells/μL) (normal -4.6 to 6.2 million cells/μL), along with an increased leukocyte count (17,100 cells/μL) (normal -4500 to 11000 cells/μL). Urine tests showed the presence of pus cells (1-2 cells/high power field), whereas chest radiological findings indicated AECOPD. The patient was advised to be admitted to the hospital and instructed to undergo physiotherapy treatment for further care.
The patient was ectomorphic, alert, and oriented to time, person, and place. Vitals were as follows: heart rate: 76 beats/min; Respiratory Rate (RR): 22 breaths/min; blood pressure: 130/70 mmHg; oxygen saturation: 97%, maintained on room air. Pallor and nasal flaring were present. Tracheal tugging was noted. Chest movement was reduced, with an increased in work of breathing due to activation of accessory muscle. Accessory muscles like platysma, sternocleidomastoid, upper traps, scalene was overused. Hollowness present at supraclavicular region.
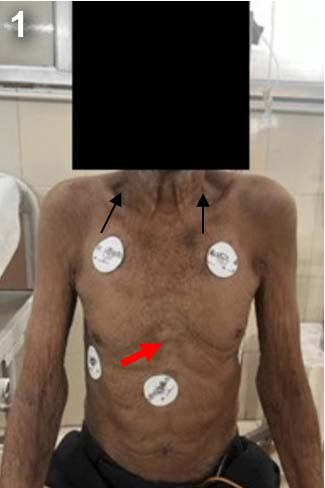
On examination, sunken chest (pectus excavatum) was observed, represented with red arrow [Table/Fig-1]. An abdominothoracic breathing pattern was noted. Tracheal fremitus was decreased in 4th-10th intercostals space. Thoracic excursion confirmed decreased chest expansion. Auscultation revealed reduced air entry in the lower zones with the presence of wheeze.
Lean body mass of patient (red arrow shows pectus excavatum).
[Table/Fig-2,3] represents chest X-ray of the patient before and after rehabilitation, taken as an outcome measure respectively to know the effectiveness of physiotherapy treatment. [Table/Fig-2] shows increased opacity in the mid and lower lung zones bilaterally, mild hyperinflation, mildly flattened, and costophrenic angles are blunted. [Table/Fig-3] shows bilateral lung opacities affecting mid and lower lung zones, and upper lung zones are relatively clear, diaphragms appear slightly flattened, costophrenic angles are sharp and not blunted.
Chest X-ray before rehabilitation.

Chest X-ray after rehabilitation.

Physiotherapy Management
The course of hospitalisation was 19 days, after two days of hospitalisation physiotherapy treatment was initiated. Physiotherapy was administered for 16 days during the hospital stay, with one session conducted each day, resulting in a total of 16 sessions. The main goals of the physiotherapy treatment were to facilitate the patient’s ventilation, improve his airways, lessen their effort during breathing, and promote relaxation. This treatment enabled the patient to perform daily tasks without becoming out of breath. The patient received information about their condition, why physiotherapy was required, and all other required steps. 16 days of intervention were given under supervision, with continuous monitoring of oxygen saturation levels [2].
[Table/Fig-4] represents physiotherapy treatment protocol [3,4]. Education about the significance of dyspnoea-relieving positions, breathing exercises, and daily routine activities was provided to the patient and caregiver. Dyspnoea-relieving positions and active limb movement were taught to the patient. The patient was also instructed to continue with the breathing exercises while doing regular daily business. It was suggested to the patient to show up for follow-up appointment. The patient was taught and instructed to practice breathing techniques in conjunction with all actions. Further progression will be made by increasing the number of repetitions to improve strength and endurance.
Outcome measures: The patient was well explained about framework of the physiotherapy sessions. Pre- and postoutcome measures were assessed. [Table/Fig-5] presents the outcome measures, which include mMRC dyspnoea grading, 6MWD, and thoracic excursion at upper and lower thoracic levels. A follow-up was taken after giving home exercise program [1,5-7].
Physiotherapy treatment protocol.
| No. of days | Problem list | Goal | Treatment |
|---|
| Day 1-Day 3 | Lack of knowledge about the health condition and its management | To educate the patient and his caregiver about patient’s condition and the importance of physiotherapy treatment | Education about the significance of dyspnoea-relieving positions, breathing exercises, and daily routine activities was provided to the patient and caregiver for 5 min. |
| Exertional dyspnoea | To reduce breathlessness and effort of breathing | Dyspnoea reliving positions (forward lean sitting positions, upright sitting in a chair.) For 10-15 minutes;
Pursed lip breathing every 3 hours, 2 sets of 10 repetitions. |
| Anxiety and depression | To reduce anxiety and depression | Buteyko technique for breathing 1 set of 5 repetitions [3,4]. |
| Day 4-Day 7 | Use of accessory muscle | Inhibition of accessory muscle | Diaphragmatic breathing, Every 3 hours, 2 sets of 10 repetitions;
Segmental breathing (coastal expansion exercises)- 2 sets of 10 repetitions. |
| Accumulation of secretion | Loosen and removal of secretion from the lungs | Nebulisation with budecort 4 times/day;
Active Cycle of Breathing Technique (ACBT)- 3 cycles [4]. Huffing. |
| Reduced chest expansion | To improve chest expansion | Active movements of trunk and extremities with breathing. 2 sets of 10 repetitions. |
| Day 8-Day 16 | Reduced strength | To improve the strength | Upper limb mobility exercise with 1 liter water bottle 2 sets of 10 repetitions. |
| Reduced endurance | To improve exercise endurance and general mobility | Spot marching 2 sets of 10 repetition; Ambulation 3 rounds i.e., 180 m Static cycling for 2 min. |
Pre and postoutcome measures [1,5-7].
| Outcome measure | On
assessment | At the time of discharge |
|---|
| mMRC dyspnoea grading [1] | Grade 3 | Grade 1 |
| 6-Minute Walk Distance (6MWD) [5] | 40 m | 320 m |
| Thoracic excursion at upper thoracic level [6,7] | 1 cm | 2 cm |
| Thoracic excursion at lower thoracic level [6,7] | 2 cm | 3 cm |
mMRC: Modified medical research council; m: Meters; cm: Centimeters
Discussion
A patient with AECOPD was managed with proper medication and cardiorespiratory physiotherapy to treat breathlessness and remove secretions. The physiotherapy management focused on breathing exercises, dyspnoea-reliving positions, relaxation techniques, Active Cycle of Breathing Technique (ACBT), and mobility exercises. Apart from pharmacological intervention, pulmonary rehabilitation is an essential component of COPD treatment. The most common and major symptom of this illness is breathlessness, which is characterised by the sensation of difficult or laboured breathing, which is especially distressing for patients [8,9]. Marchetti N and Kaplan A emphasised addressing dyspnoea and enhancing exercise endurance as key goals in COPD care. This necessitates a comprehensive treatment that includes both non pharmacological techniques, like respiratory rehabilitation and pharmacological therapies, such as bronchodilator therapy [8]. Furthermore, strategies such as pursed lip breathing have a positive impact on RR and tidal volume. The reduction in RR, coupled with an increase in tidal volume, results in decreased airway collapse, reduced airway resistance and diminished air trapping within the lungs. Consequently, this contributes to a reduction in the mechanical load imposed on respiratory muscles, ultimately leading to a decrease in dyspnoea [10-14]. Kant S and Singh GV, in their study, stated that breathing exercises are a useful as well as affordable way to manage the symptoms if given as an adjunct in the management of COPD along with standard pharmacological treatment [13]. A study done by Lalwani L et al., concluded that the short-term effect of pursed lip breathing has significant improvement in dyspnoea [15]. Airway clearance technique helps to loosen the secretions, reduce the rate of loss in lung function, lessen the frequency of exacerbations, and accelerate recovery from exacerbations [16]. Thoracic mobility exercises are designed to improve chest wall mobility, increase lung capacity, and decrease shortness of breath. Dimitrova A et al., revealed that there is positive effect on exercise capacity as well as dyspnoea [17]. A study by Arora RD and Subramanian VH concluded that for patients with obstructive airway disease, Buteyko breathing proved beneficial in enhancing breath-holding, controlling breathing and lessening breathing effort [3]. A study by Mulay SU et al., found that shoulder and chest mobility exercises were more effective at improving chest expansion and reducing breathlessness in COPD patients [18]. For hospitalised COPD patients with oxygen levels below 88%, high breathlessness scores even at rest, and who cannot tolerate physical activity, segmental breathing and positive pressure ventilation are helpful [19]. Endurance exercises like spot marching, walking and static cycling improve lung function, reduce inflammation and relieve symptoms like fatigue and shortness of breath. Aerobic exercises require oxygen and energy, which help improve diaphragm function, heart and lung endurance, reduce respiratory muscle fatigue and improve breathing efficiency [20-22]. Zeng Q et al., reported that aerobic exercises are effective and safe ways to support the therapies of stable COPD via decreasing the occurrence of acute exacerbation, as well as the possible advantages of boosting the immune system [20]. The outcome of the current study indicates that there was reduction in dyspnoea and improvement in thoracic mobility and exercise capacity, which shows the positive response towards the patient condition and rehabilitation.
Conclusion(s)
The therapeutic purpose was to reduce dyspnoea, improve thoracic excursion and improve exercise capacity. Pulmonary rehabilitation plays an effective and safe role in the context of AECOPD. When tailored to the unique needs and skills of each patient, a well designed pulmonary rehabilitation program can significantly improve the therapeutic outcome for AECOPD patients. A small 2-week program has been designed as per the requirements, and relaxation techniques have been added to improve psychological status. The baseline assessment, conducted including outcome measures such as mMRC grading for dyspnoea, 6MWD and thoracic excursion, helped in outlining the intervention protocol. This case report highlights the significant positive findings concerning reduction in dyspnoea, improvement in exercise capacity, as well as thoracic excursion.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 22, 2024
Manual Googling: Oct 10, 2024
iThenticate Software: Oct 12, 2024 (9%)
[1]. Munari AB, Gulart AA, Santos K dos, Venêncio RS, Karloh M, Mayer AF, Modified Medical Research Council Dyspnea Scale in GOLD Classification better reflects physical activities of daily livingRespir Care 2018 63(1):77-85.10.4187/respcare.0563628874609 [Google Scholar] [CrossRef] [PubMed]
[2]. Solomen S, Guidelines for the physiotherapy management of chronic obstructive pulmonary diseasePhysiother - J Indian Assoc Physiother 2019 13(2):66-72.10.4103/PJIAP.PJIAP_46_18 [Google Scholar] [CrossRef]
[3]. Arora RD, Subramanian VH, To study the effect of buteyko breathing technique in patients with obstructive airway diseaseInt J Health Sci 2019 9(3):50-64. [Google Scholar]
[4]. Baig B, Anwar M, Rasheed M, Rasul A, Fiaz A, Faisal S, Comparative effects of buteyko breathing technique and active cycle of breathing technique on dyspnea and quality of life in patients with chronic obstructive pulmonary diseaseJ Health and Rehabilitation Res 2024 4(1):250-55.10.61919/jhrr.v4i1.192 [Google Scholar] [CrossRef]
[5]. Anand KR, Raja Amarnath G, Evaluating six minute walk test as a tool to assess the severity of COPDJ Res Med Dent Sci 2021 9(6):269-77. [Google Scholar]
[6]. Bockenhauer SE, Chen H, Julliard KN, Weedon J, Measuring thoracic excursion: Reliability of the cloth tape measure techniqueJ Am Osteopath Assoc 2007 107(5):191-96. [Google Scholar]
[7]. Swathi G, Suneel S, Chakravarthi A, Sunil Kumar T, Raghunadh N, Margret M, Effectiveness of diaphragmatic stretching versus rib stretching on improving pulmonary function and thoracic excursion in subjects with COPDInternational J Innov Sci Res Tech 2021 6(10):359-67.10.52403/ijshr.20211019 [Google Scholar] [CrossRef]
[8]. Marchetti N, Kaplan A, Dyspnea and hyperinflation in chronic obstructive pulmonary disease: Impact on physical activityCCJM 2018 85(2 suppl 1):S3-10.10.3949/ccjm.85.s1.0229494327 [Google Scholar] [CrossRef] [PubMed]
[9]. O’Donnell DE, Hyperinflation, dyspnea, and exercise intolerance in chronic obstructive pulmonary diseaseProc Am Thorac Soc 2006 3(2):180-84.10.1513/pats.200508-093DO16565429 [Google Scholar] [CrossRef] [PubMed]
[10]. Ubolnuar N, Tantisuwat A, Thaveeratitham P, Lertmaharit S, Kruapanich C, Mathiyakom W, Effects of breathing exercises in patients with chronic obstructive pulmonary disease: Systematic review and meta-analysisAnn Rehabil Med 2019 43(4):509-23.10.5535/arm.2019.43.4.50931499605PMC6734022 [Google Scholar] [CrossRef] [PubMed]
[11]. Roberts SE, Stern M, Schreuder FM, Watson T, The use of pursed lips breathing in stable chronic obstructive pulmonary disease: A systematic review of the evidencePhysical Therapy Rev 2009 14(4):240-46.10.1179/174328809X452908 [Google Scholar] [CrossRef]
[12]. Holland AE, Hill CJ, Jones AY, McDonald CF, Breathing exercises for chronic obstructive pulmonary diseaseCochrane Database Syst Rev 2012 10:CD00825010.1002/14651858.CD008250.pub2 [Google Scholar] [CrossRef]
[13]. Kant S, Singh GV, Breathing exercises as adjuvant in the management of COPD: An overviewLung India 2006 23(4):16510.4103/0970-2113.44394 [Google Scholar] [CrossRef]
[14]. Mayer AF, Karloh M, Santos K dos, Araujo CLP de, Gulart AA, Effects of acute use of pursed-lips breathing during exercise in patients with COPD: A systematic review and meta-analysisPhysiotherapy 2018 104(1):09-17.10.1016/j.physio.2017.08.00728969859 [Google Scholar] [CrossRef] [PubMed]
[15]. Lalwani L, Mishra G, Gaidhane A, Quazi Syed Z, Short term effect of pursed lip breathing technique in stable patients of Chronic Obstructive Pulmonary Diseases (COPD)Euro J Mol Clin Med 2020 7(2):1342-47. [Google Scholar]
[16]. Meneses-Echavez JF, Chavez Guapo N, Loaiza-Betancur AF, Machado A, Bidonde J, Pulmonary rehabilitation for acute exacerbations of COPD: A systematic reviewRespiratory Med 2023 219:10742510.1016/j.rmed.2023.10742537858727 [Google Scholar] [CrossRef] [PubMed]
[17]. Dimitrova A, Izov N, Maznev I, Vasileva D, Nikolova M, Physiotherapy in patients with chronic obstructive pulmonary diseaseOpen Access Maced J Med Sci 2017 5(6):720-23.10.3889/oamjms.2017.17629104679PMC5661708 [Google Scholar] [CrossRef] [PubMed]
[18]. Mulay SU, Devi TP, Jagtap VK, Effectiveness of shoulder and thoracic mobility exercises on chest expansion and dyspnoea in moderate chronic obstructive pulmonary disease patientsIJPR 2017 5(2):1960-65.10.16965/ijpr.2017.115 [Google Scholar] [CrossRef]
[19]. Prajapati P, Pawaria S, Reyalch N, Comparison of respiratory proprioceptive neuromuscular facilitation and segmental breathing on pulmonary functions, dyspnoea and exercise tolerance in COPD patients: A comparative studyJ Clin Diagn Res 2023 17(7):YC05-YC09.10.7860/JCDR/2023/62620.18154 [Google Scholar] [CrossRef]
[20]. Zeng Q, Liao W, Fang W, Liu S, Duan C, Dai Y, Clinical effect of aerobic exercise training in chronic obstructive pulmonary disease: A retrospective studyMedicine 2023 102(42):e3557310.1097/MD.000000000003557337861566PMC10589605 [Google Scholar] [CrossRef] [PubMed]
[21]. Li J, Lu Y, Li N, Li P, Su J, Wang Z, Muscle metabolomics analysis reveals potential biomarkers of exercise-dependent improvement of the diaphragm function in chronic obstructive pulmonary diseaseInt J Mol Med 2020 45(6):1644-60.10.3892/ijmm.2020.4537 [Google Scholar] [CrossRef]
[22]. Patel S, Maddocks M, Man WDC, Exercise training in COPDChest 2020 158(1):09-10.10.1016/j.chest.2020.02.04032654732 [Google Scholar] [CrossRef] [PubMed]