In recent years, bupivacaine has emerged as a popular and effective Local Anaesthetic (LA) agent for providing spinal anaesthesia in a hyperbaric solution [1]. It is an amino amide compound that is also long-acting. However, accidental i.v. injection of bupivacaine is known to cause precipitous hypotension, cardiac dysrhythmias and atrioventricular heart block [2]. In fact, studies have found that the threshold for cardiac toxicity produced by bupivacaine is somewhat reduced in patients being treated with drugs that inhibit myocardial impulse propagation (β-adrenergic blockers, digitalis preparations, calcium channel blockers) [3-6], which means that one must proceed with caution whenever using bupivacaine in patients who are on antiarrhythmic drugs or other cardiac medications known to decrease impulse propagation. These shortcomings of this otherwise novel LA drug have resulted in the development of a newer LA agent, namely, ropivacaine.
Ropivacaine, the S-(-)-enantiomer of l-propyl-2,6-pipecolo-xylidid, is a newer amino amide LA agent similar to bupivacaine in chemical structure, though it is 30-40% less potent than bupivacaine [7-10]. The shorter length of the hydrocarbon chain of ropivacaine makes it lipid-soluble, thereby decreasing its potency [11]. However, this significantly increases its threshold for cardiotoxicity and Central Nervous System (CNS) toxicity compared to bupivacaine [12,13].
In the principal study by Dar FA et al., titled ‘Hyperbaric Spinal Ropivacaine in Lower Limb and Hip Surgery: A Comparison with Hyperbaric Bupivacaine’ [14], they concluded that although in terms of quality of block achieved with hyperbaric ropivacaine 0.5% was comparable to that of 0.5% hyperbaric bupivacaine, the onset of sensory and motor block, as well as, the total duration of sensory block, was significantly less in the former group. Keeping in mind the pharmacokinetic profile of ropivacaine vs bupivacaine, the authors pondered whether the use of a higher concentration of ropivacaine (0.75% in this case) would help us scale this difference in the studied characteristics and associated side-effects. Hence, the present study was an attempt to practically compare the clinical efficacy of 0.75% hyperbaric ropivacaine and hyperbaric 0.5% bupivacaine, using equal volumes of drug to assess the suitability of ropivacaine as an alternative to bupivacaine for intermediate-duration day care surgeries under spinal anaesthesia.
Materials and Methods
The present randomised double-blind clinical study was carried out in the Department of Anaesthesia, Dr. D. Y. Patil Medical College, Hospital and Research Centre (tertiary healthcare centre), Pune, Maharashtra, India, from March 2023 to August 2023. The study was authorised by the Institutional Ethics Committee (Research Protocol No. IESC/FP/42/2023), and informed consent was obtained from the patients participating in the study. Clinical Trials Registry India (CTRI) registration of the study was promptly obtained thereafter (CTRI/2023/02/050035).
Inclusion criteria: Thirty patients of American Society of Anaesthesiologists (ASA) grade I-II of either sex, with age range of 18-60 years, scheduled to undergo elective inguinal and perineal surgery under spinal anaesthesia, were included in the study.
Exclusion criteria: Patients with ASA physical status III or above, patients aged less than 18 years or over 60 years, undergoing emergency procedures, patients with major neurological, cardiac, respiratory, metabolic, renal, or hepatic diseases, any coagulation abnormalities, contraindicated for spinal anaesthesia, or known allergies to the study drugs were excluded from the study.
Sample size calculation: Based on the study by Dar FA et al., regarding hyperbaric spinal ropivacaine in lower limb and hip surgery: a comparison with hyperbaric bupivacaine [14], and considering the mean time of onset of sensory block at T10 level, total sample size was calculated to be 14, with 7 patients in each group, by keeping the confidence limits at 95%. So, in order to overcome observer bias, we decided to take a total of 30 patients, with 15 patients in each group. Hence, we included 15 patients in each group for better validity of results. Sample size was calculated using WinPEPI software.
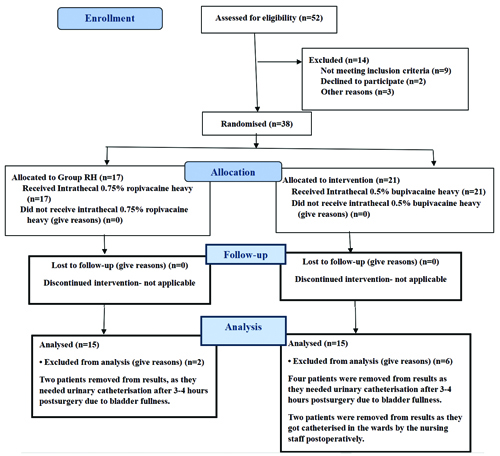
Informed consent was obtained from the patients posted for elective inguinal and/or perineal surgery, and they were then randomly divided using computer-generated numbers into two groups, with 15 patients in each group. The guidelines stated by Consolidated Standards of Reporting Trials (CONSORT) for randomised trials were followed for the present study [Table/Fig-1].
Group RH (ropivacaine heavy group): This group consisted of 15 patients who received 4 mL intrathecal injection of 0.75% hyperbaric ropivacaine (30 mg).
Group BH (bupivacaine heavy group): This group consisted of 15 patients who received 4 mL intrathecal injection of 0.5% hyperbaric bupivacaine (20 mg).
Study Procedure
Preanaesthetic check-ups were done 24 hours prior to surgery, and written informed consents were obtained. Patients were kept nil per oral from midnight before surgery. On the day of surgery, an intravenous line was established using 20G size intravenous cannula, and preloading was done in every patient (using 10-15 mL/kg of body weight of Ringer’s lactate), with baseline haemodynamic parameters {pulse rate, Mean Arterial Pressure (MAP) and Oxygen Saturation (SpO2)} noted.
Under all aseptic precautions, the subarachnoid blocks were performed using 26G Quincke spinal needle, with patient in the sitting position at L3-L4 intervertebral space. The patients were made supine immediately afterward. After the block, vitals were monitored every two minutes up to 10 minutes, and thereafter, every five-minutes interval until 20 minutes, followed by every 30 minutes interval till the completion of surgery. In order to avoid procedural and technical bias, the spinal anaesthesia was performed by the same principal investigator for all the cases included in the study. Whereas, individuals who assessed of block characteristics, haemodynamic parameters, side-effects and data entry were blinded, as well as, the individual performing statistical analysis and interpretation of the said results were blinded regarding the drug in use.
The onset and extent of sensory block (analgesia to pinprick), onset and degree of lower limb motor block (with modified Bromage Scale: 0-no motor block; 1-inability to raise extended leg, able to bend knee; 2-inability to bend knee, can flex ankle; and 3-no movement), were recorded at similar intervals as the haemodynamic parameters by an anaesthesiologist, who was unrelated to the present study. The anaesthesiologist also taking care to limit the maximum allowable height of sensory block till level T-8 by checking the sensory blockade level (analgesia to pinprick) every two minutes and providing a slight reverse Trendelenburg tilt to the bed whenever necessary.
Following surgery, the sensory block was assessed at 30-minute intervals until complete regression. The complaint of pain following pinprick at the S2 dermatome level signalled the complete recovery of sensory block, and the time was noted. The duration for regression of motor block was also noted. It was assessed using modified Bromage scale by asking the patient to flex the limb at hip, knee, and ankle joints to grade 0, which is no paralysis of lower limb movement at all the three joints mentioned above.
Postoperatively, each patient was assessed hourly for the first six hours and then every two hourly thereafter for next six hours for urinary bladder fullness using per abdomen palpation method. They were also given minimal intravenous fluids (approximately 40-50 mL of intravenous fluid per hour) in the postoperative nil per oral period (usually assigned as either 4-5 hours nil per oral postoperatively, as per surgeon’s discretion), targeting a mean arterial blood pressure of 60-65 mmHg in order to avoid excessive urinary bladder fullness. The time of the first micturition was noted. However, if evident bladder fullness was noted, then immediate Foley’s catheterisation was done and that subject was excluded from the study results.
Hypotension, defined as a decrease in systolic pressure >20% from baseline, were treated with i.v. bolus of 5 mL/kg Ringer’s lactate, and if needed, i.v. mephentermine 6 mg was administered. Bradycardia (heart rate <50 beats/min), if encountered, was treated with intravenous atropine, which was administered in small incremental doses. Fluids were administered to replace intraoperative losses. All patients were visited for 24 hours to identify any occurrences of nausea, vomiting, or other adverse sequelae.
Statistical Analysis
The continuous variables like age, Heart Rate (HR), Bromage scale and MAP, were compared across the two groups using an unpaired t-test. The statistical software SPSS software version 16.0 was used for the analysis. An alpha level of 5% was set; thus, any p-value <0.05 was considered as significant. Unpaired t-test is used to compare the two means.
Results
The distribution of the demographic profile in terms of age and gender in either group was not significant. The average duration of surgery in both group RH and group BH was found to be similar, at 85.67 minutes and 98.40 minutes, respectively [Table/Fig-2]. The time taken in both groups for the onset of sensory block and the time taken to reach T8 level has been shown in [Table/Fig-3]. The onset of the motor block for patients in group RH was faster in comparison to group BH (p-value <0.0001).
Patient characteristics and types of surgery.
| Demographic profile and type of surgery | Group RH (ropivacaine heavy)
(n=15) | Group BH (bupivacaine heavy)
(n=15) | p-value |
|---|
| Male/Female (n) | 11/4 | 11/4 | - |
| Age (years) (Mean±SD) | 42.93±14.73 | 39.06±11.94 | - |
| Hernia (n) | 4 | 5 | - |
| Fissure in ano (anal fissure surgery) (n) | 3 | 0 | - |
| Fistula in ano (n) | 3 | 0 | - |
| Excision (n) | 2 | 2 | - |
| Hydrocoele (n) | 2 | 2 | - |
| Circumcision (n) | 1 | 2 | - |
| Others (Haemorrhoids/Hysteroscopy/Ureteric calculi) (n) | 0 | 2/1/1 | - |
| Duration of surgery (min) (mean±SD) | 85.67±39.5 | 98.4±32.8 | 0.345 |
Unpaired t-test
| Observations of SAB | Group RH (n=15) | Group BH (n=15) | T value | p-value with significance |
|---|
| Onset of sensory block (min) | 2.09±0.69 | 3.66±0.55 | 6.89 | <0.001 |
| Time to T8 sensory block (min) | 3.40±0.93 | 6.68±1.67 | 6.64 | <0.001 |
| Onset of motor block (min) | 3.52±0.66 | 6.2±0.77 | 10.23 | <0.001 |
| Duration of motor blockade (min) | 261.93±73.21 | 398.93±31.03 | 6.672 | <0.00001 |
| Time taken for recession of sensory block to S2 (min) | 351.4±66.78 | 441.46±38.90 | 4.513 | <0.00001 |
| Time taken for complete recession of motor block to Bromage scale 0 (min) | 291.93±64.93 | 408.6±33.86 | 6.138 | <0.00001 |
| Time of first micturition (min) | 338.73±31.29 | 489.0±56.05 | 9.06 | <0.00001 |
Values are presented as mean±SD; SAB: Subarachnoid block; Unpaired t-test is used to compare the two means; The p-value <0.05 was considered statistically significant
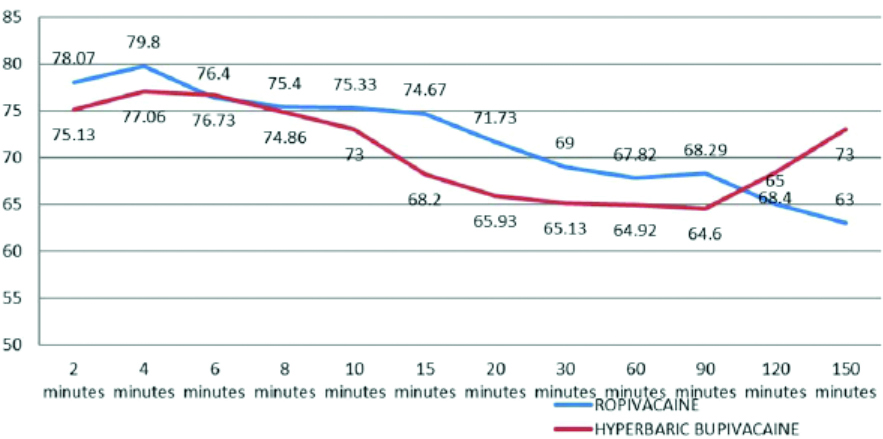
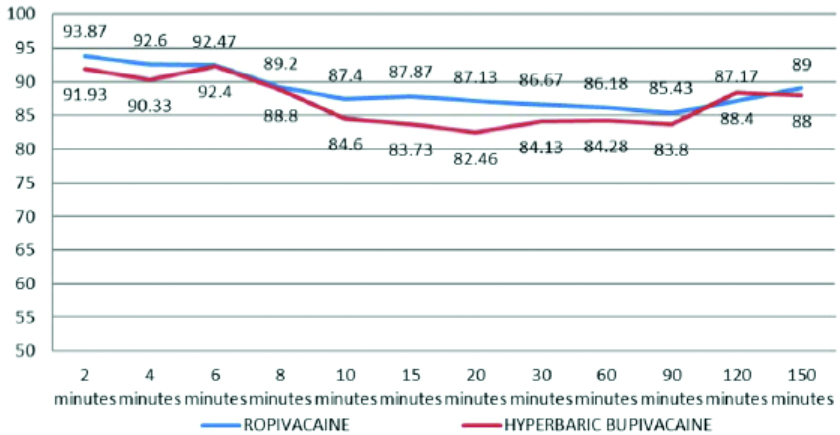
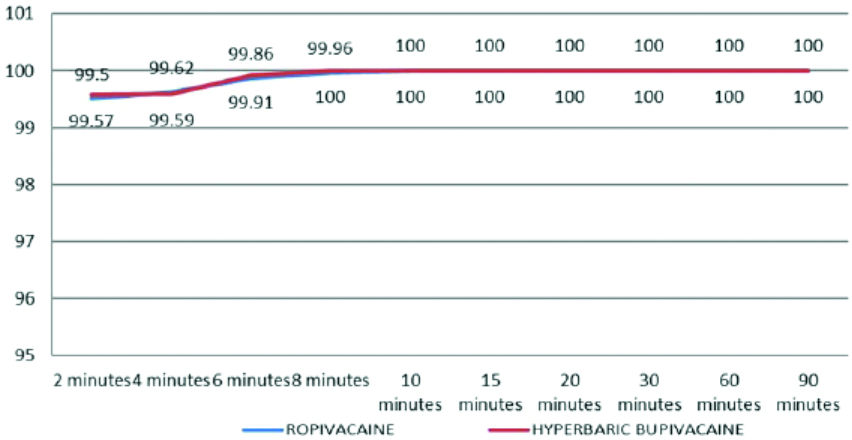
A comparison of the haemodynamic parameters, such as HR, MAP, and SpO2, between the two groups displayed a similar trend throughout the intraoperative period. HR and MAP showed a similar trend of slow decrease within the first 20 minutes from their preoperative values before settling down following spinal anaesthesia with either drug [Table/Fig-4,5]. However, none of the readings noted a fall in HR to be less than 50 beats per minute or MAP less than 20% of the baseline value preoperatively (p-value >0.05) [Table/Fig-4,5]. Same was noted with SpO2 values in either group [Table/Fig-6]. Bromage scale score for assessing motor block was found to be comparatively non significant amongst the two groups. In either group, the Bromage scale score was 2 at around two minutes following spinal anaesthesia due to the onset of motor block. By 4-6 minutes, Bromage scale score was 4 in both the groups until the end of surgery or 150 minutes post spinal anaesthesia (p-values >0.05).
Unpaired t-test is used to compare the two groups means of HR.
Unpaired t-test is used to compare the two means
Results of movement in mean arterial blood pressure in both groups.
Unpaired t-test is used to compare the two means
Results of movement in mean SpO2 in both groups.
Unpaired t-test is used to compare the two means
Although, degree of motor block achieved, in terms of the Bromage scale (Bromage score of 3 i.e., no lower limb movement), was the same for both drugs, the degree of sensory block achieved (no pain on pinprick) was also comparable. The duration of motor block and time taken for the regression of the sensory block to S2, as well as, regression of the motor block to Bromage scale 0, was longer in group BH than in group RH (p-value <0.00001) [Table/Fig-3]. Patients in group BH took, on average, 150 minutes more in pass urine post-subarachnoid block than the time taken for first micturition in group RH (p-value <0.00001) [Table/Fig-3].
In addition, there were no reported incidence of any significant intraoperative hypotension, bradycardia, nausea and vomiting, PDPH, backaches, neurological sequelae, or urinary retention post-subarachnoid block from patients in either group. The ascent of sensory block beyond T8 was noted in six cases in group RH and four cases in group BH. In all aforementioned cases, sensory blockade level has ascended to T6 without any noteworthy affliction of the haemodynamic parameters.
Discussion
As our practice gradually progresses towards ambulatory surgeries, which now also include lower abdominal surgeries like inguinal and perineal procedures, its imminent for us anaesthesiologist to devise a plan of anaesthesia to be able to adequately manage the rising challenges of daycare procedures and associated patient co-morbidities. And spinal anaesthesia has always been considered as a safe and efficient technique for inguinal and perineal surgical procedures, as it circumvents issues such as postoperative nausea and vomiting, airway manipulation, delayed recovery, and polypharmacy for pain management, which are commonly associated with general anaesthesia.
In the same vein, the resurgence of shorter-acting local anaesthetics for spinal anaesthesia, like chloroprocaine, seems like a necessary step in the right direction. However, it has not consistently produced satisfactory results, especially if there is an inadvertent increase in the duration of surgery. So, most research have shifted to finding alternatives, with the use of hyperbaric ropivacaine, often dubbed as the less potent but safer counterpart of bupivacaine.
McDonald SB et al., in her study conducted in 1999 compared 0.5% hyperbaric bupivacaine and 0.5% hyperbaric ropivacaine in eighteen healthy volunteers to assess the duration of sensory blockade with pin-prick method, transcutaneous electrical stimulation, tolerance to high tourniquet and electromyography, and isometric force dynamometry [15]. They stated that the dose-response data for bupivacaine and ropivacaine demonstrated an approximate relative potency of 2:1; that is, the effect of 4 mg of bupivacaine is similar to that of 8 mg of ropivacaine, but with a faster recovery profile for ropivacaine [11]. So, this prospective, randomised, double-blind comparative study was designed to compare clinical efficacy of 0.75% hyperbaric ropivacaine (4 mL, 30 mg) and 0.5% hyperbaric bupivacaine (4 mL, 20 mg) for inguinal and perineal surgeries.
The present study showed that the use of 30 mg of 0.75% hyperbaric ropivacaine produced faster onset of both sensory (2.09±0.69 min) and motor (3.52±0.66 min) blocks compared to 20 mg of 0.5% hyperbaric bupivacaine (time taken for sensory block onset was 3.66±0.55 min and for motor block onset was 6.20±0.77 min, respectively). Gupta R et al., concluded in their study with 0.6% hyperbaric ropivacaine that hyperbaric ropivacaine produced more consistent, reliable, and higher quality of sensory and motor block, with faster onset, as well [16].
The achievement of T8 level of sensory block was also relatively faster in the hyperbaric ropivacaine group (3.40±0.93 min) vs 6.68±1.67 min in hyperbaric bupivacaine group. Quan Z et al., also observed in their work with 0.5% hyperbaric ropivacaine in parturients for caesarean section that hyperbaric ropivacaine required less time to achieve T8 sensory blockade [17]. Interestingly, the authors noted that the level of sensory blockade ascended to T6 in six cases in the hyperbaric ropivacaine group and in four cases in hyperbaric bupivacaine group. The common factor for this finding was the positioning of these ten patients for their respective surgeries; they all required lithotomy positioning for surgical ease and access. We noticed that 10 minutes post-lithotomy positioning and spinal anaesthesia block, the sensory level blockade had ascended to reach T6. This perhaps can be explained by the fact that the tissue concentration of LA in spinal anaesthesia is controlled by the tissue blood flow in addition to Cerebrospinal Fluid (CSF) flow [18]. Also, in the lithotomy position, due to the upward positioning of the lower limbs increases both venous return to the torso and raises the intra-abdominal pressure, as well as, eliminate the concave curvature of the lumbar vertebrae, facilitating the thoracic spread of the spinal drug. However, after 20-25 minutes of the spinal anaesthesia block, the sensory blockade level did not ascend further in these ten patients.
The present study showed that the duration of motor block (398.93±31.03 minutes), followed by the time taken for the regression of the motor block to Bromage scale 0 (408.6±33.86 min), was evidently longer in the hyperbaric bupivacaine group. In comparison, the hyperbaric ropivacaine group the total duration of motor block was shorter at 261.93±73.21 min, including less time taken for the motor block regression to Bromage scale 0 (291.93±64.93 min). Casati A et al., and Kulkarni KR et al., had a similar finding in their respective researches, that the complete regression of motor block was faster in patients receiving hyperbaric ropivacaine in comparison to hyperbaric bupivacaine and levobupivacaine [19,20].
Regression of sensory block to S2 also showed faster recovery (351.4±66.78 min) in the hyperbaric ropivacaine group in comparison to the hyperbaric bupivacaine group (441.46±38.90 min). This can be ascribed to the greater lipid solubility and marginally increased protein binding capacity of bupivacaine relative to ropivacaine [21,22]. Higher lipid solubility of any LA agent means there will be greater sequestration of the LA within the myelin sheath and adjacent neural compartments, which will, in turn, act as storage depots for a gradual and slow release of these agents, consequently leading to a longer duration of action of the local anaethesia agent (bupivacaine) [23]. This finding too, in agreement with the results of a study carried out by Dar FA et al., and Luck JF et al., where they found that the duration of sensory block and its regression, both to T10 level as well as complete regression, were shorter in the hyperbaric ropivacaine group [14,24].
One of the hallmarks of early ambulatory discharge protocol is a shorter time for the voiding of urine postspinal anaesthesia, was also significantly shorter in our study with hyperbaric ropivacaine group (338.73±31.29 min) by almost 150 minutes versus hyperbaric bupivacaine group (489.0±56.05 min). In a similar vein, Whiteside JB et al., and Kulkarni KR et al., concluded that good sensory blocks with hyperbaric ropivacaine were associated with a favourable recovery when compared with bupivacaine, with earlier mobilisation and shorter time taken for first micturition [7,20].
Thus, on completion of the present study, the authors can now concentrate on using 0.75% hyperbaric ropivacaine in smaller doses and with adjuvants on individuals with known systemic and/or functional limitations, ASA class III or IV. The present study would probably be amongst the few studies [25-29] that has compared 0.75% hyperbaric ropivacaine with 0.5% hyperbaric bupivacaine recently, in terms of efficacy as an equivalent or maybe even a more potent contender for day care surgeries.
Limitation(s)
The limitations of the present study would definitely be the need for rating patients’ experience and comfort level in terms of the relative recovery profile. Also, the effect of addition of additives such as opioids and study their respective potencies and duration of spinal action/regression with a smaller volume of the parent LA agents. As this was the first time 0.75% hyperbaric ropivacaine was used, the authors wanted to evaluate its action and drug profile in comparison to 0.5% hyperbaric bupivacaine. Hence, the authors decided to use full dose of both the drugs while keeping in mind the dose toxicity limits of each, which made it safer to include only ASA class I and II patients in the study. Thus, on completion, the authors can now concentrate on using 0.75% hyperbaric ropivacaine in smaller doses and with adjuvants on individuals with known systemic and/or functional limitations, ASA class III or IV.
Conclusion(s)
The 0.75% hyperbaric ropivacaine turns out to be faster in terms of both sensory and motor blockade onset, as well as, the time taken to achieve T8 level sensory block, in comparison to 0.5% hyperbaric bupivacaine. Though, degree of motor block achieved, in terms of Bromage scale (Bromage score of 3 i.e., no lower limb movement), is the same for both drugs, as is the degree of sensory block achieved (no pain on pin prick). The main take away, however, would definitely have to be faster reversal of motor block and early recovery of sensation of urination in the hyperbaric ropivacaine group, in comparison to the bupivacaine group patients.
Unpaired t-test
Values are presented as mean±SD; SAB: Subarachnoid block; Unpaired t-test is used to compare the two means; The p-value <0.05 was considered statistically significant