Introduction
Rehabilitation is a vital part of recovery for stroke patients, presenting a complex intervention that requires collaboration among patients, caregivers and the rehabilitation team. Telerehabilitation has emerged as a promising alternative to standard outpatient and home-care rehabilitation, offering advantages such as minimal travel barriers, flexible exercise schedules and the integration of skills into daily activities.
Need of the study
The technologies that can be used for telerehabilitation range from inexpensive internet-based solutions, virtual reality, and robotic systems to more costly telephones and mobile phones, which are present in most homes. Physiotherapists have been suggested as being in the best position to help stroke victims transition from the hospital to their homes. However, there has been significant international professional resistance to using telerehabilitation-based services, based on the belief that the lack of in-person care may result in worse outcomes. Nevertheless, research on numerous chronic health disorders demonstrates that telerehabilitation strategies can effectively enhance results. There is a dearth of literature comparing tele-based supervision for task-oriented exercises with institution-based supervision for task-oriented exercises. Thus, the need for this study is to identify a cost-effective method for rehabilitation in stroke patients.
Aim
To compare the effect of institution-based supervision and tele-based supervision for task-oriented exercises on upper limb motor performance and functional ability among stroke patients.
Materials and Methods
A two-group pretest-post-test randomised clinical trial will be conducted in recognised hospitals in Mullana and Panipat, using purposive sampling from December 2022 to December 2024. A total of 62 male and female patients, aged 45-75 years, who have experienced their first ischaemic or haemorrhagic stroke within the last six months and have scores ranging from 26 to 56 on the Fugl-Meyer Assessment for Upper Extremity (FMA-UE), mild to moderate spasticity (less than 2 on the Modified Ashworth Scale (MAS), >24 on the Mini-mental State Examination (MMSE), and stages II and III of the Brunnstrom score will be included in the study. Group B will receive institution-based supervision for task-oriented exercises, whereas Group A will receive tele-based supervision for live sessions. Both groups will perform task-oriented exercises for 30 minutes, three days a week for eight weeks. There will be a 30-second break before switching tasks. Outcome measures, including the Fugl-Meyer Assessment for Upper Extremity (FMA UE) and the Motor Evaluation Scale for Upper Extremity in Stroke Patients (MESUPES), will be assessed at baseline, the 4th week, and the 8th week of intervention, respectively. Repeated measures of Analysis of Variance (ANOVA) or the Friedman test will be chosen based on normality to find differences within the groups at baseline, the 4th week, and the 8th week (completion). A paired t-test or Wilcoxon signed-rank test will be applied to identify differences between the groups for pre-post intervention changes in outcome measures. An Independent t-test or Mann-Whitney U-test will be applied based on normality to compare the changes in mean values of the outcome measures between Group A and Group B at baseline, the 4th week, and the 8th week of intervention. The level of statistical significance will be set at alpha=0.05.
Introduction
Stroke is the second largest cause of illness and death worldwide and ranks third in terms of disability, with 150,000 deaths annually. Approximately two-thirds of survivors require rehabilitation treatments due to persistent disabilities [1]. The annual incidence of stroke in India is estimated to be between 105 and 152 per 100,000 [2]. Stroke can have a major impact on a person’s life, affecting their physical, mental, social and cognitive wellbeing [3]. Upper limb dysfunction makes it extremely difficult to carry out tasks that demand gross motor skills, such as walking, self-protective reflexes and balance [4]. It also creates obstacles in everyday tasks requiring fine motor skills, such as eating, writing and personal hygiene activities [5]. Various therapies can be employed alone or in combination to address the multifaceted nature of potential post-stroke deficits, incorporating a variety of approaches to tackle issues and side-effects. Task-specific exercises are defined as training or therapy where the patient has to practice context-specific motor tasks and receive some form of feedback; concerning skill learning, it may be associated with different practice conditions, feedback, and conditions of transfer [6]. The focus is on training in functional tasks rather than impairments. Post-stroke, there is evidence that task-specific upper limb training not only impacts functional recovery but also brain activation patterns. Patients have found that telerehabilitation therapies offer fewer travel obstacles, flexible exercise schedules and the opportunity to better integrate skills into everyday activities. These therapies have been effectively employed in the fields of chronic illness management and preventive care [7,8]. Telerehabilitation can be provided through a variety of technologies, from more expensive phones to mobile phones that are common in most households, as well as low-cost internet-based programs, virtual reality and robotic systems. It has been suggested that physiotherapists are the most qualified to assist stroke victims in making the transition from the hospital to their homes; however, a lack of in-person care may lead to worse outcomes, and there has been strong professional opposition to using telerehabilitation-based services across the globe [9]. This study aims to evaluate and compare the effect of institution-based supervision and tele-based supervision for task-oriented exercises on upper limb motor performance and functional ability among stroke patients.
Objectives:
To evaluate the effect of institution-based supervised task-oriented exercises on upper limb motor performance and functional ability among stroke patients.
To evaluate the effect of tele-based supervised task-oriented exercises on upper limb motor performance and functional ability among stroke patients.
To compare the effects of institution-based supervision and tele-based supervision of task-oriented exercises on upper limb motor performance and functional ability among stroke patients.
Null hypothesis: There will be no significant difference between institution-based supervision and tele-based supervision for task-oriented exercises regarding upper limb motor performance and functional ability among stroke patients.
Alternative hypothesis: There will be a significant difference between institution-based supervision and tele-based supervision for task-oriented exercises regarding upper limb motor performance and functional ability among stroke patients.
Review of Literature
Task-oriented training is a behavioural approach in which the therapist focuses on the tasks that need to be performed to meet certain goals or achieve a specific performance standard. Task-oriented training aims to improve control strategies by addressing difficulties through various measures. One objective of rehabilitation after a stroke is to maximise the subject’s independence in gross motor skills and walking, thus improving overall quality of life.
Levy CE et al., conducted a study to examine how a home-based program called the Rural Veterans Telerehabilitation Initiative (RVTRI) helped Veterans with physical therapy. The program used video calls to connect the Veterans with their physical therapists. The researchers studied 26 Veterans who participated in the program between February 22, 2010, and April 1, 2011. They measured the Veterans’ progress using different tests. The results showed that the Veterans made significant improvements in their ability to carry out daily activities, their memory, their walking speed, and their overall health. The Veterans also reported being satisfied with the program. The study also found that by using the RVTRI program, the Veterans were able to save on travel time and costs [9].
A separate study by Cramer SC et al., concluded that activity-based training produced substantial gains in arm motor function, regardless of whether it was provided via home-based telerehabilitation or traditional in-clinic rehabilitation. The findings of this study suggested that telerehabilitation has the potential to substantially increase access to rehabilitation therapy on a large scale [10]. In another study by Dodakian L et al., patients with chronic hemiparetic stroke underwent a 28-day home-based telerehabilitation program, which involved daily individualised exercises, games and stroke education. The study included 12 participants who showed significant improvement in arm motor status, with high compliance and substantial gains in stroke prevention knowledge. The system also demonstrated potential in effectively monitoring and improving the health of stroke patients [5].
Despite significant progress in research on telerehabilitation competencies, there remains a lack of clarity regarding which competencies are essential for effective implementation. Additionally, insufficient research exists on patient competencies and corresponding frameworks aligned with guidelines. By aggregating and mapping available data on telerehabilitation abilities, the goal is to bridge these research gaps and establish a comprehensive competence framework for telerehabilitation.
Materials and Methods
A two-group pretest-post-test randomised clinical trial will be conducted in recognised hospitals of Mullana and Panipat using purposive sampling from December 2022 to December 2024. A total of 62 subjects will complete baseline assessments before randomisation and follow-up assessments in the 4th and 8th weeks. Written informed consent will be obtained from the patients. The study has been approved by the Institutional Research Ethics Committee (IEC-2317). The trial has also been registered under the Clinical Trials Registry-India (CTRI/2023/02/050093).
Inclusion criteria: Both male and female patients aged 45 to 75 years, having a first-ever stroke, between 2 to 6 months post-stroke, with moderate to mild motor impairment scored 26-56 on the FMA-UE [11,12], mild to moderate spasticity scored <2 on the MAS [13], scored >24 on the MMSE [14], and scored stage II and III on the Brunnstrom score [15] and who are willing to participate will be included in the study.
Exclusion criteria: Patients with progressing stroke, visual problems, excessive joint contractures, or other neurological diseases will be excluded from the study.
Sample size calculation: Sample size estimation is done using G*Power 3.1.9.4 software (Heinrich-Heine-Universität Düsseldorf, Germany) with the following parameters:
Effect size of FMA scale: 0.2 (according to the pilot study)
Level of Significance: 0.05
Power: 80%
Calculated sample size=42.
Considering a dropout rate of 20%, the total sample size will be 62. The manual block randomisation approach will be used to evenly split the patients into two groups: Group-A (N=31) and Group-B (N=31). Given that this study has 62 participants, there will be four blocks with a 16 by 4 matrix design [Table/Fig-1].
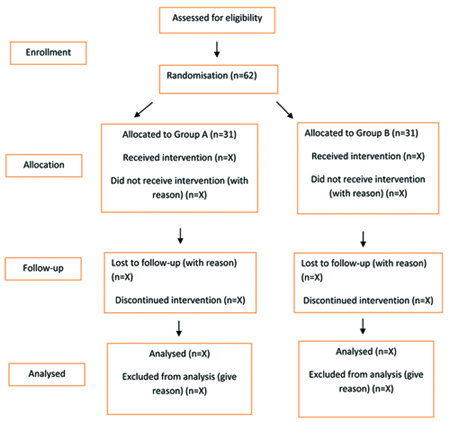
Written consent will be obtained from all patients who meet the inclusion criteria of the study, and the required assessments of every patient will be conducted. A total of 62 subjects will be included, divided into two groups. Group A will receive Tele-based Supervision for task-oriented exercises, while Group B will receive Institution-based Supervision for task-oriented exercises.
Task-oriented exercises will be administered three days per week for eight weeks, for 30 minutes to both groups [Table/Fig-2] [16]. A 30-second rest will be provided before changing tasks. Data will be collected utilising the FMA-UE and MESUPES. Three readings will be taken: one before the treatment, the second after the 4th week, and the third after the 8th week.
Protocol for task oriented exercises [16].
| S. No. | Exercises | Repetition |
|---|
| 1. | To stimulate shoulder movements (flexion, abduction, extension)
Reaching forward to pick up or touch an object Reaching sideways to pick up an object from a table and transferring it to a table in front Grasping and releasing objects with the arm stretched out behind
| 5 Repetitions |
| 2. | To stimulate supination
Fingers around cylindrical object, the patients attempts to supinate the forearm. Try to turn the palm to face upward
| 5 Repetitions |
| 3. | Stimulate wrist extension and radial deviation
Patient sitting with arm supported on the table Forearm in mid position, fingers and thumb around a glass. The patient attempts to lift the object up Try to lift the glass off the table. Try to put it down on the table slowly
| 5 Repetitions |
| 4. | To stimulate palmar abduction and rotation of thumb (opposition)
Holds the forearm in mid position and wrist in extension, while patient attempts to grasp and release a cylindrical object
| 5 Repetitions |
| 5. | To train opposition of radial and ulnar sides of hand (cupping of the hand)
Forearm in supination Patients practices opposing thumb and others fingers, particularly fourth and fifth fingers
| 5 Repetitions |
| 6. | To train control over the manipulation of objects
Practice picking up polystyrene cup around the rim without deforming it. Practice by picking it up, holding it while moving the arm and releasing it, do it with his hand close to his body, away from his body and in conjunction with the other hand. (pouring water from one cup to another) Practice picking a piece of paper from his opposite shoulder
| 5 Repetitions |
Outcomes: Upper limb motor recovery and functional ability will be measured using the FMA-UE. The FMA is a disease-specific performance-based assessment with three distinct impairment sections: sensation, balance and voluntary movement of the upper and lower extremities. Additionally, passive range of motion and discomfort will be assessed. The overall Intraclass Correlation Coefficient (ICC) was 0.96, indicating strong interclass reliability [11,12].
To evaluate the performance of the upper extremities, the MESUPES will be used. The MESUPES assessment instrument uses an ordinal scale. It consists of nine hand items with three answer categories and eight arm tasks with six response categories (scores 0-5) and (scores 0-2). The relative and absolute reliability of the MESUPES was high, with an ICC of 0.98 and a Standard Error of Measurement (SEM) of 2.68 [17].
Statistical Analysis
The data will be analysed using the Statistical Package for the Social Sciences (SPSS) version 23.0 and IBM SPSS software. The collected demographic information and outcome measures will be assessed for normality using the Kolmogorov-Smirnov test. Demographics will be expressed using descriptive statistics. Repeated measures of ANOVA or the Friedman test will be applied based on normality to find differences within the group at baseline, the 4th week, and the 8th week (completion). A paired t-test or Wilcoxon signed-rank test will be used to find differences between the groups for pre- and postintervention changes in outcome measures. An Independent t-test or Mann-Whitney U-test will be applied based on normality to compare the changes in mean values of the outcome measures between Group A and Group B at baseline, the 4th week, and the 8th week of intervention. A p-value of <0.05 will be considered significant.
[1]. Feigin VL, Brainin M, Norrving B, Martins S, Sacco RL, Hacke W, World Stroke Organization (WSO): Global Stroke Fact Sheet 2022Int J Stroke 2022 17(1):18-29.Erratum in: Int J Stroke. 2022;17(4):478. Doi: 10.1177/1747493022108034310.1177/1747493021106591734986727 [Google Scholar] [CrossRef] [PubMed]
[2]. Jones SP, Baqai K, Clegg A, Georgiou R, Harris C, Holland EJ, Stroke in India: A systematic review of the incidence, prevalence, and case fatalityInt J Stroke 2022 17(2):132-40.10.1177/1747493021102783434114912PMC8821978 [Google Scholar] [CrossRef] [PubMed]
[3]. GBD 2019 Stroke CollaboratorsGlobal, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019Lancet Neurol 2021 (10):795-820. [Google Scholar]
[4]. Pollock A, Farmer SE, Brady MC, Langhorne P, Mead GE, Mehrholz J, Interventions for improving upper limb function after strokeCochrane Database Syst Rev 2014 2014(11):CD01082010.1002/14651858.CD010820.pub2 [Google Scholar] [CrossRef]
[5]. Dodakian L, Meckenzie AL, Le V, See J, Pearson Fuhrhop K, Quinlan EB, A home-based telerehabilitation program for patients with strokeNeurorehabilitation and Neural Repair 2017 31(10-11):923-33.10.1177/154596831773381829072556PMC5734923 [Google Scholar] [CrossRef] [PubMed]
[6]. Laver KE, Adey-Wakeling Z, Crotty M, Lannin NA, George S, Sherrington C, Telerehabilitation services for strokeCochrane Database Syst Rev 2020 31:110.1002/14651858.CD010255.pub332002991PMC6992923 [Google Scholar] [CrossRef] [PubMed]
[7]. Bosch JO, Donnell MJ, Barreca S, Thabane L, Wishart L, Does task-oriented practice improve upper extremity motor recovery after stroke? A systematic reviewISRN Stroke 2014 2:01-10.10.1155/2014/504910 [Google Scholar] [CrossRef]
[8]. Seron P, Oliveros MJ, Gutierrez-Arias R, Fuentes-Aspe R, Torres-Castro RC, Merino-Osorio C, Effectiveness of telerehabilitation in physical therapy: A rapid overviewPhys Ther 2021 101(6):pzab05310.1093/ptj/pzab05333561280PMC7928601 [Google Scholar] [CrossRef] [PubMed]
[9]. Levy CE, Silverman E, Jia H, Geiss M, Omura D, Effects of physical therapy delivery via home video telerehabilitation on functional and health-related quality of life outcomesJ Rehabil Res Dev 2015 52(3):361-70.10.1682/JRRD.2014.10.023926230650 [Google Scholar] [CrossRef] [PubMed]
[10]. Cramer SC, Dodakian L, Le V, See J, Augsburger R, Mckenzie A, Efficacy of home-based telerehabilitation vs in-clinic therapy for adults after stroke. A randomized clinical trialJAMA Neurology 2019 76:910.1001/jamaneurol.2019.160431233135PMC6593624 [Google Scholar] [CrossRef] [PubMed]
[11]. Sanford J, Moreland J, Swanson LR, Stralford PW, Gowland C, Reliability of the Fugl-Meyer assessment for testing motor peformance in patients following strokePhys Ther 1993 73(7):447-54.10.1093/ptj/73.7.4478316578 [Google Scholar] [CrossRef] [PubMed]
[12]. Hiragami S, Inoue Y, Harada K, Minimal clinically important difference for the Fugl-Meyer assessment of the upper extremity in convalescent stroke patients with moderate to severe hemiparesisJ Phys Ther Sci 2019 31(11):917-21.10.1589/jpts.31.91731871377PMC6879402 [Google Scholar] [CrossRef] [PubMed]
[13]. Meseguer-Henarejos AB, Sánchez-Meca J, López-Pina JA, Carles-Hernández R, Inter- and intra-rater reliability of the Modified Ashworth Scale: A systematic review and meta-analysisEur J Phys Rehabil Med 2018 54(4):576-90.Epub 2017 Sep 1310.23736/S1973-9087.17.04796-72890111910.23736/S1973-9087.17.04796-728901119 [Google Scholar] [CrossRef] [PubMed] [CrossRef] [PubMed]
[14]. Folstein MF, Folstein SE, McHugh PR, “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinicianJ Psychiatr Res 1975 12(3):189-98.10.1016/0022-3956(75)90026-61202204 [Google Scholar] [CrossRef] [PubMed]
[15]. Brunnstrom S, Motor testing procedures in hemiplegia: Based on sequential recovery stagesPhysical Therapy 1966 46(4):357-75.Available from: https://doi.org/10.1093/ptj/46.4.35710.1093/ptj/46.4.3575907254 [Google Scholar] [CrossRef] [PubMed]
[16]. Carr JH, Shephered RB, Neurological rehabilitation: Optimizing motor performance3rd editionChurchill Livingstone:242-278. [Google Scholar]
[17]. Johansson GM, Häger CK, Measurement properties of the motor evaluation scale for upper extremity in stroke patients (MESUPES)Disabil Rehabil 2012 34(4):288-94.10.3109/09638288.2011.60634321981318 [Google Scholar] [CrossRef] [PubMed]