Introduction
In India, liver cirrhosis is a significant public health concern, contributing to 2.95% of total deaths. Cirrhosis is the advanced stage of ongoing liver fibrosis, which poses substantial global health challenges due to its fatal consequences, such as gastroesophageal varices.
Need of the study
Gastroesophageal varices are a potentially lethal complication of liver cirrhosis. The severity of these varices directly impacts the prognosis of the patient. Gastroesophageal varices are major contributors to both mortality and morbidity on a global scale. While various parameters have been explored to predict the progression and severity of these varices, platelet indices have not been extensively studied in cirrhosis patients with gastroesophageal varices in India.
Aim
To study the association and correlation of platelet indices with the severity of gastroesophageal varices in patients with liver cirrhosis.
Materials and Methods
A cross-sectional study will be conducted in the Medicine OPD/IPD of Acharya Vinoba Bhave Rural Hospital (AVBRH), Wardha, Maharashtra, India from May 2023 to May 2025, involving 64 patients who meet the inclusion and exclusion criteria. Patients fulfilling the selection criteria will be informed about the study procedure in their native language. The diagnosis of liver cirrhosis will be established based on the patient’s detailed history, physical examination, laboratory tests, and ultrasound scan. Upon enrollment, a detailed history will be taken, and parameters will be recorded in a specifically designed proforma. Initial parameters will include age, gender, weight, co-morbidities (such as Diabetes Mellitus (DM), Hypertension (HTN), Heart Failure (HF), Cardiovascular Disease (CVS), Chronic Obstructive Pulmonary Disease (COPD), kidney failure, liver failure, and malignant conditions), and the aetiology of cirrhosis. Platelet count and indices-Mean Platelet Volume (MPV), Platelet Distribution Width (PDW), and Plateletcrit (PCT)-will be assessed. The categorical and continuous variables will be represented as frequency (percentage) and mean (standard deviation, SD). The Chi-square test and Independent sample t-test will be used to evaluate the association between various categorical variables and continuous variables. The Pearson correlation test will be used to assess any correlation between platelet indices and oesophageal varices, with a significance level set at <0.05.
Introduction
Cirrhosis is the end stage of advancing liver fibrosis, resulting in the distortion of hepatic architecture [1]. Complications associated with cirrhosis are a major cause of mortality and morbidity worldwide. These complications rank among the top causes of death globally. Cirrhosis is the 15th most common cause of morbidity and the 11th most common cause of death [2]. In 2017, cirrhosis accounted for nearly 1.32 million deaths, with almost two-thirds of these being males and one-third females, representing 2.2% of overall deaths [3]. Similarly, in India, liver cirrhosis is a significant health problem. In 2017, deaths from liver disease in India reached an estimated 2.95% of total deaths, accounting for one-fifth (18.3%) of global deaths due to cirrhosis [4]. Nearly all fatalities resulted from decompensated cirrhosis. Decompensation usually refers to the onset of ascites, oesophageal variceal bleeding, hepatic encephalopathy, and, in certain cases, elevated bilirubin levels in individuals with compensated cirrhosis [5]. The mortality and morbidity associated with cirrhosis significantly increase when decompensation occurs. The one-year mortality rate during the progression of the disease can range from 1-57%, depending on the degree of decompensation [6,7]. However, one-year mortality rates as high as 80% have been reported.
Upper Gastrointestinal System (GIS) bleeding is a significant cause of mortality in patients with cirrhosis and portal hypertension [8]. The presence of cirrhosis leads to portal hypertension, resulting in the enlargement of the portal vein, ascites, splenomegaly, and the development of portosystemic collaterals [9]. The main goal in managing cirrhosis is to prevent bleeding from oesophageal varices. In clinical practice, the risk of upper digestive tract bleeding is assessed using Oesophago-Gastro-Duodenoscopy (EGD). Indicators include variceal size, the appearance of cherry-red spots, and the severity of cirrhotic changes as determined by the Child-Pugh classification [10]. Endoscopic colour Doppler ultrasonography, possibly in conjunction with upper EGD, is always considered the gold standard for evaluating the risk of bleeding in patients with oesophageal varices [10,11].
Erdem MG et al., reported that the MPV levels of patients with cirrhosis were higher than those of the control group [11]. Liu H et al., compared platelet indices in cirrhotic patients with and without oesophageal varices and demonstrated that in the group of patients with oesophageal varices, the PCT showed a gradual decrease as the severity of varices increased. In the group with oesophageal collateral veins, a notable difference was observed in PCT, which negatively correlated with the degree of collateral vein formation [12]. However, both groups did not differ significantly in MPV and PDW. Additionally, Erdogan AM et al., found no association between MPV and variceal bleeding [13]. Thus, the role of platelet indices in cirrhotic patients with oesophageal varices needs further evaluation.
The present study aims to evaluate the association and correlation of platelet indices with the severity of gastroesophageal varices in patients with liver cirrhosis.
Primary objectives:
To estimate the various platelet indices (PDW, MPV, PCT Absolute Platelet Count) in cases of liver cirrhosis.
To perform upper gastrointestinal endoscopy for gastroesophageal varices in patients with liver cirrhosis.
To grade the severity of oesophageal varices according to the modified Paquet and Sarin classification.
Secondary objective:
To estimate the correlation and association of various platelet indices (PDW, PCT, MPV) with the severity of oesophageal varices according to the modified Paquet and Sarin classification.
Review of Literature
One of the most frequent side-effects of liver cirrhosis is oesophageal varices, which require immediate medical attention if they burst and bleed. Consequently, early detection of oesophageal varices and their severity positively impacts the long-term prognosis of patients with liver cirrhosis. Therefore, non invasive testing to identify oesophageal varices has emerged as a focal point for study in recent years [14].
Erdem MG et al., examined platelet and MPV levels in 201 liver cirrhosis patients and found no significant correlations with the Child-Pugh classification or cirrhosis aetiology. The patients were divided into groups based on the aetiology of Chronic Liver Disease (CLD). The average platelet count was lower in cirrhosis patients compared to the control group, while the MPV was higher in cirrhotic patients [11]. Similarly, a study by Ma Y et al., concluded that non surviving patients with Hepatitis B Virus-Related Decompensated Cirrhosis (HBV-DeCi) had significantly higher levels of MPV compared to surviving patients. Both MPV and the end-stage liver disease score independently predicted three-month mortality (p-value <0.01), suggesting that elevated MPV may be a standalone indicator for predicting mortality within three months [15].
Furthermore, a retrospective study conducted by Mohamed MS et al., assessed the association of MPV with clinical features, complications, and severity in 114 patients with cirrhosis. The association of MPV was studied with parameters associated with cirrhosis, the model for end-stage liver disease score, and the fibrosis (FIB4) score. The authors noted a positive relationship between MPV and serum bilirubin, international normalised ratio, and lower serum albumin levels. The study also showed that patients with advanced liver disease, as determined by the model for end-stage liver disease and FIB4 scores, had higher MPV values, which were significant. Thus, the study concluded that MPV has the potential to serve as a cost-effective and significant biomarker for assessing the severity and prognosis of cirrhosis [16].
Similarly, using a retrospective approach, Liu H et al., examined the predictive usefulness of platelet markers and a grading system for predicting the presence of collateral veins and oesophageal varices in 94 patients with liver cirrhosis. The patients were categorised into two groups: those without Oesophageal Varices and those with gastroesophageal varices. The gastroesophageal varices group was further divided into mild, moderate, and severe subgroups. The authors observed that in the gastroesophageal varices group, PLT count and PCT decreased gradually with the rise in the severity of oesophageal varices. PCT and PLT count were negatively correlated with the degree of collateral veins in the oesophageal collateral vein group. In the gastroesophageal varices group, the mean diameter of oesophageal collateral veins and maximum cross-sectional diameter were wider compared to the without gastroesophageal varices group. PCT could effectively predict the existence of oesophageal varices. FI, FIB-4, Lok, and FibroQ scoring systems could effectively predict the presence of oesophageal varices and paraoesophageal collateral veins (p-value <0.05), with the Lok Index being better than other rating systems. Thus, the study concluded that PCT and the LOK index are reliable indicators for identifying the presence of oesophageal varices and paraoesophageal veins [12].
Additionally, to verify MPV, PDW, and PCT in 142 patients with alcohol-related liver cirrhosis (ALC), a retrospective study was conducted by Michalak A et al., involving 92 patients with Non alcoholic Fatty Liver Disease (NAFLD) and 68 in the control group. The study observed a significant rise in PDW and a reduction in PCT in patients with ALC (p-value <0.0001) and NAFLD (p-value <0.01) relative to controls. MPV was significantly reduced in NAFLD (p-value <0.0001). PCT correlated with NFS (p-value <0.0001). MPV and PDW correlated with the Model for End-Stage Renal Disease (MELD) scores. PCT and MPV had the greatest diagnostic accuracy in patients with ALC and NAFLD, respectively. Thus, the study concluded that PCT in ALC and MPV in NAFLD can be used as potential diagnostic markers [17].
Materials and Methods
A cross-sectional study will be conducted in the Medicine Department of a tertiary-level hospital (Acharya Vinoba Bhave Rural Hospital) in the Wardha district, Maharashtra, India from May 2023 to May 2025. All consecutive cirrhotic patients with endoscopically diagnosed gastroesophageal varices attending the Medicine OPD/IPD of Acharya Vinoba Bhave Rural Hospital (AVBRH) for two years will be enrolled. IEC approval has been obtained from Datta Meghe Institute of Health, Education and Research, Wardha, with Reference number: DMIMS (DU)/IEC/2023/929 (dated 11/04/2023). Written informed consent will be obtained from the participants before conducting the study.
Inclusion criteria:
Patients aged 18 years or older.
Patients of either gender.
Patients with cirrhosis of the liver.
Patients with endoscopically diagnosed gastroesophageal varices.
Exclusion criteria:
Patients with liver failure.
Patients with portal vein thrombosis who have undergone jugular intrahepatic portosystemic shunt.
Patients with liver cancer or other malignant tumours.
Patients with thrombocytopenia, splenomegaly caused by haematological diseases, splenectomy, gastroesophageal varices ligation, propranolol use, or the use of other vasoactive drugs to reduce portal hypertension.
Patients with infections.
ALT levels greater than 10 times the normal upper limit.
Patients whose platelet count is affected by other significant factors.
Patients unwilling to sign an informed consent form.
Sample size: The sample size was calculated by the following formula:
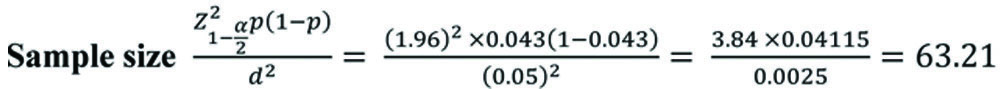
Where:
p=prevalence of ALD=4.3%=0.043, [18]
d=Absolute precision required on either side of the proportion=5% points=0.05 (2-sided), and
Z0.025=1.96 for 95% confidence interval
Thus, the sample size is calculated to be 64 patients. Patients fulfilling the selection criteria are informed about the study procedure in their native language. The diagnosis of liver cirrhosis will be established based on the patient’s detailed history, physical examination, laboratory tests, and ultrasound scan.
Upon enrollment, a detailed history and parameters will be recorded in a specifically designed proforma. Initial parameters will include age, gender, weight, co-morbidities (such as DM, HTN, HF, CVD, COPD, kidney failure, liver failure, and malignant conditions), and the aetiology of cirrhosis. Subsequently, a thorough clinical examination will be performed, and parameters including vital signs (temperature, heart rate, respiratory rate, and mean blood pressure) and the Glasgow Coma Scale (GCS) will be recorded.
Outcomes:
Under aseptic precautions, peripheral venous blood specimens will be collected to analyse the Complete Blood Count (CBC), platelet count, and indices such as MPV, PDW and PCT.
Gastroesophageal varices are serpentine and tortuous, often characterised by the presence of the red sign or gastroesophageal varices in beads, nodules, and tumours (with or without the presence of the red sign). Additionally, patients in the group will undergo endoscopic ultrasonography. The examination will focus on two types of collateral veins: paraoesophageal collateral veins (para-ECV) and perioesophageal collateral veins (peri-ECV). Para-ECV refers to thick collateral veins located outside the oesophageal wall, without contacting the muscular layer. The maximum diameters of para-ECV will be recorded, categorising them into mild (internal diameter ≥2 mm) [12]. The severity of oesophageal varices will be assessed using a modified Paquet and Sarins classification [19].
MPV is defined as the volume of the average circulating platelet and is measured in femtoliters. The MPV value may vary based on the technique used for measurement (i.e., it is instrument-specific). Additionally, a patient’s actual platelet distribution may not fit into a log-normal distribution. Consequently, manufacturers emphasise the importance of referring to the laboratory’s reference values for the study population under consideration. MPV in sodium citrate in normal subjects shows a normal range of 4.5-8.5 fL with a mean of 6.5 fL. Variation in MPV is minimal, with an approximate coefficient of variation (CV) of 2.1%. The expected range of values for MPV in our laboratory is 7.2 to 11.7 fL [20].
Liver function tests, including Alanine Aminotransferase (ALT), Aspartate Aminotransferase (AST), total Bilirubin (TBIL), Blood Urea Nitrogen (BUN), Uric Acid (UA), and Creatinine (Cr), will be evaluated. Additionally, a coagulation profile will be assessed, which includes Prothrombin Time (PT), International Normalisation Ratio (INR), and Activated Partial Thromboplastin Time (APTT).
Subsequently, patients will undergo an abdominal ultrasound to evaluate the shape, size, and echotexture of the liver, as well as the presence of any fluid or dark anechoic areas in the abdominal and pelvic cavities, including the depth of any effusions. This will be followed by an endoscopic examination for the detection of gastroesophageal varices and the estimation of the maximum cross-sectional diameter of paraoesophageal and perioesophageal collateral veins, using endoscopic ultrasonography.
Investigations include:
Complete blood count
Coagulation profile
Abdominal ultrasound
Upper GI endoscopy
Statistical Analysis
Data will be collected, and graphics will be designed using Microsoft Office Excel 2019. The data will be analysed with Statistical Package for the Social Sciences (SPSS) (IBM, Armonk, NY, USA) version 23.0 for Windows. Categorical and continuous variables will be represented as frequency (percentage) and mean (standard deviation, SD), respectively. The Pearson and Spearman correlation tests will be used to assess the correlation between two ranked variables. The Chi-square test and Independent sample t-test will be used to evaluate the association between various categorical and continuous variables, respectively. Receiver Operating Characteristic (ROC) analysis will be performed to determine the best cut-off point of platelet indices in predicting prognosis. Multiple regression analysis will be conducted for platelet indices. A two-tailed probability value of <0.05 will be considered statistically significant.
[1]. Anthony PP, Ishak KG, Nayak NC, Poulsen HE, Scheuer PJ, Sobin LH, The morphology of cirrhosis. Recommendations on definition, nomenclature, and classification by a working group sponsored by the World Health OrganizationJ Clin Pathol 1978 31:395-414.10.1136/jcp.31.5.395649765PMC1145292 [Google Scholar] [CrossRef] [PubMed]
[2]. Global Health Estimates. Geneva: World Health Organization 2016 [Internet]. [cited 2020 June 15]. Available from: https://www.who.int/healthinfo/global_burden_disease/estimates/en/ [Google Scholar]
[3]. Cheemerla S, Balakrishnan M, Global epidemiology of chronic liver diseaseClin Liver Dis (Hoboken) 2021 17(5):365-70.10.1002/cld.106134136143PMC8177826 [Google Scholar] [CrossRef] [PubMed]
[4]. Mishra D, Dash KR, Khatua C, Panigrahi S, Parida PK, Behera SK, A study on the temporal trends in the etiology of cirrhosis of liver in coastal Eastern OdishaEuroasian J Hepatogastroenterol 2020 10(1):01-06.10.5005/jp-journals-10018-131232742964 [Google Scholar] [CrossRef] [PubMed]
[5]. Fleming KM, Aithal GP, Card TR, West J, The rate of decompensation and clinical progression of disease in people with cirrhosis: A cohort studyAliment Pharmacol Ther 2010 32:1343-50.10.1111/j.1365-2036.2010.04473.x21050236 [Google Scholar] [CrossRef] [PubMed]
[6]. Mokdad AA, Lopez AD, Shahraz S, Lozano R, Mokdad AH, Stanaway J, Liver cirrhosis mortality in 187 countries between 1980 and 2010: A systematic analysisBMC Med 2014 12:14510.1186/s12916-014-0145-y25242656PMC4169640 [Google Scholar] [CrossRef] [PubMed]
[7]. D’Amico G, Garcia-Tsao G, Pagliaro L, Natural history and prognostic indicators of survival in cirrhosis: A systematic review of 118 studiesJ Hepatol 2006 44:217-31.10.1016/j.jhep.2005.10.01316298014 [Google Scholar] [CrossRef] [PubMed]
[8]. Arthur MJ, Reversibility of liver fibrosis and cirrhosis following treatment for hepatitis CGastroenterology 2002 122:15252810.1053/gast.2002.3336711984538 [Google Scholar] [CrossRef] [PubMed]
[9]. Czaja AJ, The prevention and reversal of hepatic fibrosis in autoimmune hepatitisAliment Pharmacol Ther 2014 39:385-406.10.1111/apt.1259224387318 [Google Scholar] [CrossRef] [PubMed]
[10]. Yoshiji H, Nagoshi S, Akahane T, Asaoka Y, Ueno Y, Ogawa K, Evidence-based clinical practice guidelines for Liver Cirrhosis 2020J Gastroenterol 2021 56(7):593-619.Epub 2021 Jul 710.1007/s00535-021-01788-x34231046PMC8280040 [Google Scholar] [CrossRef] [PubMed]
[11]. Erdem MG, Çil EÖ, Tükek T, Helvacı ŞA, Evaluation of platelet and mean platelet volume levels in patients with liver cirrhosisArch Clin Experi Med 2018 3:18-21.10.25000/acem.390029 [Google Scholar] [CrossRef]
[12]. Liu H, Chen P, Jiang B, Li F, Han T, The value of platelet parameters and related scoring system in predicting oesophagal varices and collateral veins in patients with liver cirrhosisJ Clin Lab Anal 2021 35:e2369410.1002/jcla.2369433389784PMC7957998 [Google Scholar] [CrossRef] [PubMed]
[13]. Erdogan AM, Benli AR, Acmali SB, Koroglu M, Atayan Y, Danalioglu A, Predictive value of mean platelet volume in variceal bleeding due to cirrhotic portal hypertensionEuroasian J Hepatogastroenterol 2017 7(1):06-10.10.5005/jp-journals-10018-120329201764PMC5663766 [Google Scholar] [CrossRef] [PubMed]
[14]. Dertinger SH, Vestner H, Müller K, Merz M, Hahn EG, Altendorf-Hofmann A, Prospective study of diagnosis, therapy and follow-up of acute gastrointestinal hemorrhage in 397 patientsWien klin Wochenschr 1996 108(22):717-21. [Google Scholar]
[15]. Ma Y, Quan W, Zhu H, High mean platelet volume is associated with worse outcomes in patients with HBV-related decompensated cirrhosisAnn Clin Lab Sci 2018 48:639-45. [Google Scholar]
[16]. Mohamed MS, Bassiony MAA, Elsayed Mohamed AF, The role of mean platelet volume in predicting severity and prognosis of liver cirrhosis in Egyptian patientsEgypt J Intern Med 2019 31:261-65.Available from: https://doi.org/10.4103/ejim.ejim_111_1810.4103/ejim.ejim_111_18 [Google Scholar] [CrossRef]
[17]. Michalak A, Cichoż-Lach H, Guz M, Kozicka J, Cybulski M, Jeleniewicz W, Plateletcrit and mean platelet volume in the evaluation of alcoholic liver cirrhosis and nonalcoholic fatty liver disease patientsBiomed Res Int 2021 2021:886798510.1155/2021/886798533644233PMC7901043 [Google Scholar] [CrossRef] [PubMed]
[18]. Amonker S, Houshmand A, Hinkson A, Rowe I, Parker R, Prevalence of alcohol-associated liver disease: A systematic review and meta-analysisHepatol Commun 2023 7(5):e013310.1097/HC9.000000000000013337102767PMC10146123 [Google Scholar] [CrossRef] [PubMed]
[19]. Boregowda U, Umapathy C, Halim N, Desai M, Nanjappa A, Arekapudi S, Update on the management of gastrointestinal varicesWorld J Gastrointest Pharmacol Ther 2019 10(1):01-21.10.4292/wjgpt.v10.i1.130697445PMC6347650 [Google Scholar] [CrossRef] [PubMed]
[20]. Demirin H, Ozhan H, Ucgun T, Celer A, Bulur S, Cil H, Normal range of mean platelet volume in healthy subjects: Insight from a large epidemiologic studyThromb Res 2011 128(4):358-60.10.1016/j.thromres.2011.05.00721620440 [Google Scholar] [CrossRef] [PubMed]